- Submissions

Full Text
Orthopedic Research Online Journal
Giant Liposarcoma in Left Thigh
Leopoldo Maizo1* and Fedor Marín2
1Orthopedic Surgeon, Medical Specialist in Joint Replacement Surgery, Venezuela
2Orthopedic Surgeon, Medical Specialist in Joint Replacement Surgery, Venezuela
*Corresponding author: Leopoldo Maizo, Orthopedic Surgeon, Medical Specialist in Joint Replacement Surgery, Venezuela
Submission: January 19, 2023;Published: February 20, 2023

ISSN: 2576-8875 Volume10 Issue3
Abstract
The liposarcoma is located epidemiologically second of all tumors affecting soft tissues in adults, with an incidence between the 4th and 6th decade of life and a slight tendency towards males, their location commonly can have observed in the lower extremities by 80%, however, it is important to mention that may appear in other areas of the body such as chest or abdominal cavity. It can be classified according to the degree of aggressiveness of the same in 4 subtypes being the most common and less aggressive well-differentiated liposarcoma. The treatment of choice is surgical and aesthetic and functional results are almost always satisfying.
Case report: A male patient aged 62 who presented progressive increase in volume in the left thigh, after imaging and analysis of biopsy is scheduled for surgical resection of well-differentiated liposarcoma. marginal resection is performed with biopsy confirmatory free margins control tumor tissue, without infectious complications and with adequate functional recovery
Keywords:Liposarcoma; Tumor; Soft tissue
Introduction
Although a high percentage of tumors located in soft tissues are usually benign, it is important to be aware of the existence of malignant tumors in order to make an accurate differential diagnosis [1]. Liposarcoma is epidemiologically located in the second place of all tumors affecting soft tissues in adults, representing 10 to 30% of all tumors affecting soft tissues, with an incidence between the 4th and 6th decade of life and a slight tendency towards the male sex, Its location can be commonly observed in the lower extremities in 80% [2], particularly in the thigh where its location predominates in 50%, gluteal region and inguinal region, however it is important to mention that it can appear in other areas of the body such as the thorax, mediastinum, retro peritoneum, small intestine and mesentery [3]. Liposarcoma in the thigh is located mainly in the deepest layers, in its initial stages there are no symptoms, so most of the time it is usually detected with the presence of a palpable mass that increases progressively, many times this increase in volume can occupy large spaces and can cause compression of blood vessels and nerves [4]. The dimensions of the liposarcoma and the compromise it generates according to its location can be determined by means of X-ray studies, Magnetic Resonance and Computed Axial Tomography [5], the surgical treatment will depend on a good histopathological study which will determine the prognosis of the evolution of the pathology [6].
The World Health Organization (WHO) currently admits four types of liposarcoma:
A. Well-differentiated (or atypical lipoma): the most frequent (50% of all liposarcomas). Low degree of aggressiveness (does not metastasize but can relapse locally). It can dedifferentiate [7,8].
B. Myxoid: Intermediate degree of aggressiveness, it includes as the highest grade subtype, the variant called “round cell”. It is the most frequent subtype in children. There is a risk of metastasis, especially in the round cell variant [7,8].
C. Pleomorphic: The most infrequent (5-10% of
liposarcomas). It can simulate a malignant fibrohistiocytoma or
even a carcinoma or melanoma. It presents a high risk of local
recurrence and metastasis [7,8].
D. Undifferentiated: It is a high grade sarcoma (malignant
fibrohistiocytoma, fibrosarcoma or others) originated on
a well-differentiated liposarcoma. It is more frequent in
retroperitoneal lesions and has a high risk of metastasis [7,8].
The main consideration is the preservation of the extremity, which will be determined by the type of liposarcoma. Although amputation has historically been the surgical option of choice for these tumors, currently most of them can be treated by limbsparing surgery. However, the performance of limb-sparing surgery should not compromise the primary oncologic goal, which is cure, and should ensure a limb whose function is better than that which would be provided by a post-amputation prosthesis [9]. The resection of liposarcoma must be performed in a wide manner since this can prevent the lesion from recurring [10].
The use of chemotherapy and radiotherapy before and after the surgical procedure is mentioned in a very controversial way due to its advantages and disadvantages that can be generated, the indication of radiotherapy sessions can give us benefits since the tumor can really diminish in size after its application, making the surgery more technically feasible. On the other hand, surgical complications increase, especially those related to the incision area, where the complications are 25% [5,11]. It has been suggested, however, that the improvement in the oncologic prognosis of patients with liposarcomas and the decrease in the incidence of permanent late complications would justify the use of preoperative radiotherapy, despite the higher rate of complications [12]. The role of chemotherapy in the treatment of liposarcoma remains controversial; optimally, its use should be assessed in each individual case.
Case Report
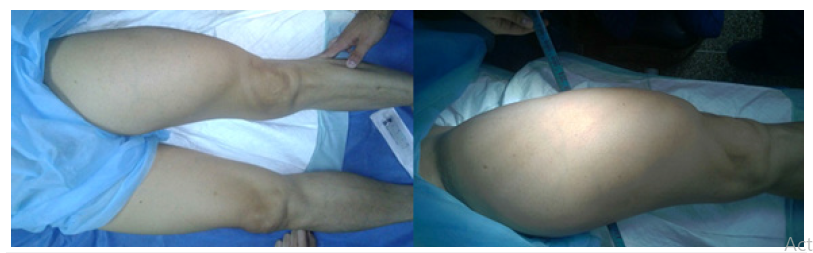
This is a 62-year-old male patient with progressive enlargement of 4 years of evolution in the left thigh, who came to the outpatient clinic of musculoskeletal tumors of the Military Hospital Coronel Elbano Paredes Vivas in June 2015, in view of functional limitation and mild pain during walking, it is indicated complementary imaging studies and take a biopsy in July 2015, where the result of the same reports well-differentiated liposarcoma. Nuclear magnetic resonance images show a large volume tumor mass of approximately 16.47cm in transverse length, 11.52cm thick and 37.65cm in vertical length (Figure 1).
Figure 1:An increase in volume can be seen in the anterolateral aspect of the left thigh.
In April 2016, surgery was performed under general anesthesia, anterolateral approach of the left thigh was performed by double longitudinal incision of approximately 40cm, section of the femoral fascia, identification of the undamaged femoral bundle, direct visualization of the soft tissue tumor and peripheral divulsion of the tumor respecting 2cm of healthy tissue, identification of tumor vascular pedicle and satisfactory ligation of the same, phenolization of the nerve branches, adequate marginal resection of the tumor with section of 50% of the rectus femoris, presence of adhesions of distal portion of vastus intermedius, synthesis by planes and final closure, transferring the patient in stable general conditions to the recovery area (Figure 2). A sample of tumor piece of 40x20cm approx. is sent for a new biopsy study and the patient is discharged satisfactorily after 72 hours. In May 2016, biopsy results were obtained confirming the presence of well-differentiated liposarcoma with tumor-free margins (Figure 3). After 4 months of follow-up, surgical scar without complications, left thigh with hypotrophy of muscle mass and without limitation of hip and knee joint mobility compared to the contralateral limb. Patient denies pain and currently with adequate reintegration and in the beginning of physical therapy and rehabilitation for strengthening of muscle groups of the anterior compartment of the left thigh (Figure 4).
Figure 2:Nuclear magnetic resonance of the left thigh before surgery
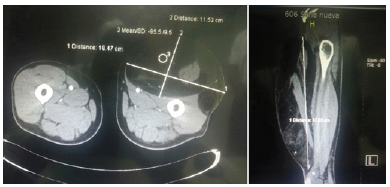
Figure 3:Marginal resection of Liposarcoma of 3.8Kg.
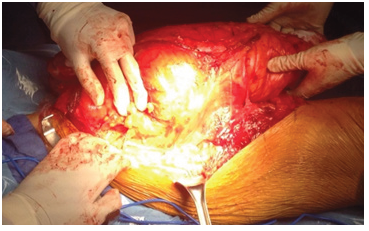
Figure 4:Aspect of the surgical scar on the left thigh.

Discussion
Well-differentiated liposarcoma represents the most frequent subtype of liposarcoma, it increases progressively in size and is usually painless unless it compresses nerve structures [7,8]. The treatment of choice even today continues to be surgery, which in order to achieve oncologically acceptable results must resect the whole piece with adequate resection margins of approximately 1cm [13]; which is particularly favorable when it is not adhered to the neurovascular bundle of the limb and the tumor vascular pedicle is identified to avoid important hematic losses. Generally, the exeresis of these tumors is not difficult since they present a pseudocapsule. Survival and recurrence-free time depend on the histological subtype and the surgical resection margin [13]. In some centers chemotherapy is used as adjuvant. The most commonly used drug are Adriamycin and Isofosfamide. A response is obtained in up to 50% of cases without being able to demonstrate an increase in survival [14].
Well-differentiated liposarcomas treated with surgery and perioperative radiotherapy (before or after surgery) have a local recurrence rate of less than 10% and a metastasis rate very close to 0%. In contrast, pleomorphic liposarcomas relapse in one third of cases and spread in 40%. The 5-and 10-year survival rates for patients with liposarcomas are 100% and 87% for the welldifferentiated variant, 88% and 76% for the myxoid type, and 56% and 39% for the pleomorphic variant [15].
Conclusion
It can be concluded that after marginal resection of a giant liposarcoma favorable functional results can be achieved without alteration of joint biomechanics, the identification of the tumor vascular pedicle is essential to avoid blood loss and soft tissue infections, the follow-up of this type of patients is important, as well as the results obtained by biopsy of the margins free of tumor tissue.
References
- Pike JM, Clarkson PW, Masri BA (2008) Soft tissue sarcomas of the extremities: How to stay out of trouble. BCMJ 50(6): 310-317.
- Ortiz-Ibáñez B, Amaya JV, Baixauli F, Angulo M, Mayordomo-Aranda E, et al. (2015) Surgical resection of massive liposarcomas at the extremities: A 10-year experience in a referral musculoskeletal sarcoma unit. World Journal of Surgical Oncology 13: 206.
- Sultan M, Burezq H, Bang RL, El-Kabany M, Eskaf W (2008) Giant gluteal lipoma-like liposarcoma: A case report. World Journal of Surgical Oncology 6: 81.
- Costea R, Vasiliu E, Zarnescu N, Hasouna M, Neagu S (2011) Large thigh liposarcoma-diagnostic and therapeutic features. Journal of Medicine and Life 4(2): 184-188.
- Colman MW, Lozano-Calderon S, Raskin KA, Hornicek FJ, Gebhardt M (2014) Non-neoplastic soft tissue masses that mimic sarcoma. Orthop Clin North Am 45(2): 245-255.
- Issakov J, Soyfer V, Kollender Y, Bickels J, Meller I, et al. (2006) Liposarcoma in adult limbs treated by limb-sparing surgery and adjuvant radiotherapy. Bone & Joint Journal 88(12): 1647-1651.
- Deka M, Saikia CJ, Sarma S (2016) Morphological spectrum of liposarcoma of extremities: A series of 13 cases from a tertiary care center of North-East India. Int J Sci Stud 4(3): 82-86.
- Peterson JJ, Kransdorf MJ, Bancroft LW, O Connor MI (2003) Malignant fatty tumors: Classification, clinical course, imaging appearance and treatment. Skeletal Radiology 32(9): 493-503.
- Spiro IJ, Gebhardt MC, Jennings C, Mankin HJ, Harmon DC, et al. (1997) Prognostic factors for local control of sarcomas of the soft tissues managed by radiation and surgery. Seminars in Oncology 24(5): 540-546.
- Jawad MU, Scully SP (2010) In brief: Classifications in brief: Enneking classification: Benign and malignant tumors of the musculoskeletal system. Clinical Orthopaedics and Related Research 468(7): 2000-2002.
- Robinson E, Neugut AI, Wylie P (1988) Clinical aspects of postirradiation sarcomas. J Natl Cancer Inst 80(4): 233
- Zagars GK, Goswitz MS, Pollack A (1996) Liposarcoma: Outcome and prognostic factors following conservation surgery and radiation therapy. Int J Radiation Oncology Biol Phys 36(2): 311-319.
- Singer S, Antonescu CR, Riedel E, Brennan MF (2003) Histologic subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann Surg 238: 358-371.
- Henricks WH, Chu YC, Goldblum JR, Weiss SW (1997) Dedifferentiated liposarcoma: A clinicopatological analysys of 155 cases with a proposal for an expanded definition of dedifferentiation. Am J Surg Pathol 21(3): 271-281.
- Prendergast B, Fiveash JB, Gibbs CP, Scarborough MT, Indelicato DJ (2010) Radiotherapy for soft tissue sarcoma of the proximal lower extremity. Sarcoma 2010: 829498.
© 2023 Leopoldo Maizo. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






