- Submissions

Full Text
Orthopedic Research Online Journal
Medial Calcar Osteotomy in Revision of Total Hip Arthroplasty
Alireza*
Tehran university of medical science, Iran
*Corresponding author: Alireza, Tehran university of medical science,Iran
Submission: November 18, 2022;Published: January 06, 2023

ISSN: 2576-8875 Volume10 Issue3
Introduction
Total Hip Arthroplasty (THA) is one of the most successful orthopedic surgeries. However, occasionally, due to certain postoperative complications such as infections, aseptic osteolysis or joint instability, the artificial joint may be destroyed and re-surgery is needed, particularly in younger people and those with excessive physical activity. As a result, the longer period of artificial joint is being used, the higher is the number of Revision Total Hip Arthroplasty surgeries. Furthermore, the improvement of diagnostics tools to detect those patients who required re-surgery, as well as increasing the number of orthopedic surgeons, have led to more and more THA surgical procedures. This fact can be more documented by available data indicating a 79% increase in number of THA surgeries between 1990 and 2002 in the United States [1]. This trend is expected to continue in future.
The available data indicate that about 1.2 percent of THA receiving patients in the United States suffered from postoperative infection complication. Joint infection is one of the cases in which re-surgery is required. Re-surgery costs more than primary surgery, takes longer to operate, and is more difficult in terms of surgical technique. Also, there is possibility of complications during surgery such as bone fractures and cortical perforations.
Revision total hip arthroplasty may need stem revision as a part of the procedure in both cemented and non-cemented total hip arthroplasties. In both types of stems, sometimes it may be necessary to do proximal femur osteotomy to remove stem or cement from the femur. Conventional osteotomy is the osteotomy of the greater trochanter that separates abductors and greater trochanter from the femur and disrupts the abductor function. It is necessary to reattach the greater trochanter to the femur to restore this function. It is obvious that if the abductor mechanism cannot be fully restored, total hip arthroplasty may result is an abnormal function which in turn may lead to at least persistent limping. With Calcar osteotomy, it is possible to remove stem and cement from the femur without disruption of the extensor mechanism.
In one approach, after exposing the proximal femur, the distal part of the stem or cement should be located. This can be achieved by preoperative planning to estimate the length of stem or cement mantle or may be done via intraoperative fluoroscopy. Following the determination of the exact point of the distal part of the stem or cement mantle, it should be marked on the femur. Afterward, a line from the midpoint of the proximal femur would be drawn toward the marked point at the tip of the stem.
Prophylactic wiring is done about one centimeter distal to the stem tip. Then a transverse line is drawn toward the medial cortex of the femur. Finally, longitudinal osteotomy and transverse osteotomies are done. With one or two broad osteotomes, the osteotomy should be opened over the intact opposite hinge. Then the stem and cement removal from the femur can be performed. After preparing the femur and inserting the new stem, the osteotomy segment will be closed and fixed in place by wiring.
However, there may be some complications. For instance, the fracture of lateral cortex of femur can change calcar osteotomy to three-part osteotomy. If this occurs, both medial and lateral segments should be wired over the inserted stem. Gentle handling of the lateral side of the femur can prevent this complication. Comminution and shattering of the osteotomized segment are another complication. Cracking of the distal part of the femur is a complication that makes distal fixation impossible. Nonunion of osteotomy also complicate the result of surgery.
Methods
This study was carried out in Sina Hospital, Tehran University of Medical Sciences, from 2015 to 2019. During calcar osteotomy, the stem was removed from the medial of the femur shaft and below the lesser trochanter. This method is different from the conventional method which involves the stem removal from the lateral and greater trochanteric regions.
Results
A total of 28 cases of calcar osteotomy was investigated. The gender distribution was as 12 males (42%) and 16 females (58%). The mean age of the studied population was 59.2 years old (34 to 80) with an average BMI of 25.1 (from 21 to 28). The patients were followed up to six months. Figure 1 shows an example of a series of images acquired during a short time follow-up.
Figure 1:The radiographic images of two patients followed up for a period of 6 months. A and D: Before surgery, B and E: Early post-op of Medial calcar osteotomy and C and F: after 6 months of Medial calcar osteotomy.
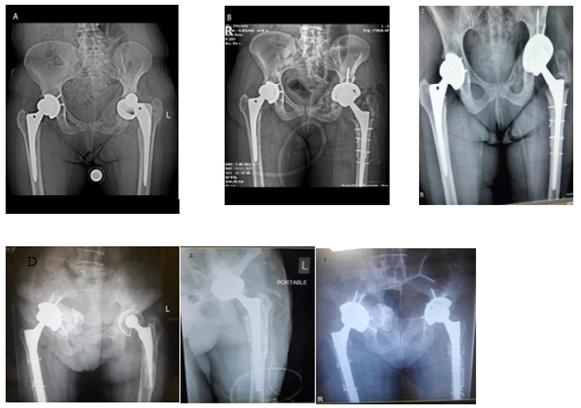
All of the cases needed distal fixation stems. Fracture of lateral cortex occurred in 6 cases (21.4%) and comminution and fracture of the osteotomy segment occurred in 5 cases (17.8%). There were 4 non-unions of the osteotomy segment (14.2%) that all of them were asymptomatic. There was no extension of the fracture line to the distal segment and there was no subsidence of stem. The average Harris Hip score in the last visit was 82.1 (69 to 96). There was a case of acute deep infection (3.5%) treated with irrigation and debridement. There was one dislocation (3.5%) treated with closed reduction. The average Leg length discrepancy is 0.6 centimeter (0 to 3 centimeters). There were three heterotopic ossifications (10.7%) that all of them were stage 2 in brook classification. There were 27 lateral approaches (96.5%) and one posterior approach (3.5%). The average operation time was 145 minutes (110 to 180 minutes).
Discussion
In this study, 28 patients who were candidates for THA revision by calcar osteotomy were evaluated. According to the studies of Kavanagh et al. [2], Chareancholvanich et al. [3] and Marcos et al. [4], the selected sample size is acceptable. The studied patients were approximately the same as the patients evaluated in similar studies [5-7]. All studies were applied within the same age range, indicating that people between 60 and 70 years of age are most exposed to artificial joint damage after surgery. In this sense, paying more attention to this age population can control the risk of developing Arthroplasty and reoperation. The number of males and females was almost equal, as seen in other studies, demonstrating the equal chance of reoperation for both sexes [5,8].
Our patients were followed up for 6 months. The rate of lateral cortex fracture during surgery was 21.4%, which is lower than the study of McLaughlin et al (reported to be 29%). Besides, the rate of dislocation was 21% in the mentioned study, which was higher than our report (only 3.5%). In contrast to McLaughlin et al. report which highlighted the pain and the need for walker/cane usage in complicated patients, all of our patients were asymptomatic. The overall rate of complications during and after surgery in our study was lower than that of McLaughlin et al. [9]. In this sense, in our study, the HHS was found to be 82 which was slightly lower than McLaughlin report (HSS:84).
Marcos et al. have reported that two patients needed further surgery due to acetabular failure, which was not showed up in our study [4]. The incidence of complications such as superficial infection (debridement treatment and antibiotics) and joint dislocation was similar (one case of infection and two cases of dislocation).
In a study done by McCallum and colleagues [10], in 15 patients who underwent THA revision, the existing cement was reshaped by using ultrasonic devices. This manipulation caused fewer complications during or after surgery in the patients and the resurgery was reported only in one case, a year after THA revision due to instability. No other complications were observed. However, due to the small sample size and low follow-up time (2 years), more researches are needed on this topic. Nevertheless, the lower incidence of complications in this type of surgery can urge us to use this method to help patients for better conditions.
In our study, the non-union rate was 14.2%. Based on F. Langlais et al. report [11], these non-union cases required reoperation, while in our study did not. Also, in the mentioned study, the muscle strength of the abductor group was reduced to 5.4, but in ours, we did not observe any decrease in abductor muscle strength, which may indicate that claudication is more likely to occur in their studied patients.
Another study by Dearborn, JOHN T (6) et al found that patients had an average limb-length discrepancy of 1.6cm before reoperation which decreased by an average of 0.9cm after surgery. In our study, this average was 0.6cm, which was less than the above study. This can increase the quality of life in these patients, which can be measured by Harris hip score. In the study by DEARBORN, the HHS was 52 before surgery and 80 after surgery, which is slightly less than our study.
In another study by Lecerf et al. [12], among the 50 studied patients, only one case of infection and two cases of bone dislocation were seen, which is less than our reports. In addition, Harris hip score in this study increased from 47 (before reoperation) to 92 (after surgery) and the size difference between the legs decreased from 4cm to 2cm on average.
Conclusion
In conclusion, we found that the revision surgery rate was higher in patients with 60 to 70 years of age , accompanied by higher efficacy (higher Harris hip score, lower discrepancy, and higher abductor muscle strength) and the overall lower rate of complications (including, acetabular failure, reoperation of nonunion cases and infections) during and after surgery in patients undergoing calcar osteotomy. Because in this type of surgery, the abductors stayed in line with femoral shaft, it results in a better outcome for those patients who need to have THA.
Statement of Ethics
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and its later amendments. Informed consent was obtained from all patients for being included in the study.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
- Bumpass DB, Nunley RM (2012) Assessing the value of a total joint replacement. Curr Rev Musculoskelet Med 5(4): 274-282.
- Kavanagh BF, Fitzgerald RH (1987) Multiple revisions for failed total hip arthroplasty not associated with infection. J Bone Joint Surg Am 69(8): 1144-1149.
- Chareancholvanich K, Tanchuling A, Seki T, Gustilo RB (1999) Cementless acetabular revision for aseptic failure of cemented hip arthroplasty. Clin Orthop Relat Res 1999(361): 140-149.
- Marcos L, Buttaro M, Comba F, Piccaluga F (2009) Femoral cement within cement technique in carefully selected aseptic revision arthroplasties. Int Orthop 33(3): 633-637.
- Kutzner KP, Emanuel R, Stefanie D, Ralf B, Joachim P, et al. (2020) Mid-term migration pattern of a calcar-guided short stem: A five-year EBRA-FCA-study. J Orthop Sci 25(6): 1015-1020.
- Bozic KJ, Patricia K, Miriam C, Linda O, Michael DR, et al. (2005) Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Joint Surg Am 87(3): 570-576.
- Dearborn JT, Harris WH (1999) High placement of an acetabular component inserted without cement in a revision total hip arthroplasty. Results after a mean of ten years. J Bone Joint Surg Am 81(4): 469-480.
- Fernández FM, Antonio M, Agustin B, Antonio M, Jorge B (2010) Revision of failed total hip arthroplasty acetabular cups to porous tantalum components: a 5-year follow-up study. J Arthroplasty 25(6): 865-872.
- McLaughlin JR, Harris WH (1996) Revision of the femoral component of a total hip arthroplasty with the calcar-replacement femoral component. Results after a mean of 10.8 years postoperatively. J Bone Joint Surg Am 78(3): 331-339.
- McCallum JD, Hozack WJ (1995) Recementing a femoral component into a stable cement mantle using ultrasonic tools. Clin Orthop Relat Res 1995(319): 232-237.
- Langlais F, Lambotte JC, Ph Collin, Langlois F, Fontaine JW, et al. (2003) Trochanteric slide osteotomy in revision total hip arthroplasty for loosening. J Bone Joint Surg Br 85(4): 510-516.
- Lecerf G, Fessy MH, Philippot R, Massin P, Giraud F, et al. (2009) Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res 95(3): 210-219.
© 2023 Alireza. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






