- Submissions

Full Text
Orthopedic Research Online Journal
Albumin And Hypoalbuminemia: Relevance in Orthopaedic Surgery
Michelle J Lespasio*
Nurse Practitioner and Assistant Professor, Department of Orthopaedic Surgery, Boston Medical Center, USA
*Corresponding author: Michelle J Lespasio, Nurse Practitioner and Assistant Professor, Department of Orthopaedic Surgery, Boston Medical Center, Boston, USA
Submission: November 11, 2022;Published: December 21, 2022

ISSN: 2576-8875 Volume10 Issue2
Abstract
The primary purpose of this article is to report the latest medical research on hypoalbuminemia (low serum albumin) and its association with the following postsurgical outcomes: (a) impaired wound healing, (b) prolonged hospitalization, (c) higher complication rates, and (d) possible systemic infection (leading to), (e) higher mortality and morbidity, and (f) increased health care burden. Additionally, this article will address hypoalbuminemia in terms of: (a) pathogenesis (b) prevalence, (c) clinical significance and (d) management. A six-item true or false quiz in the beginning of the article serves as a primer to orient the readers with their understanding of the material.
Keywords: Serum albumin; Hypoalbuminemia; Postoperative outcomes; Inflammation; Infection; Sepsis; Malnutrition; Malnourished; Orthopaedic surgery
List of Abbreviations and Definitions: mg/kg: Milligram Per Kilogram; g/dL: Grams Per Deciliter; g/L: Grams Per Liter, AKI: Acute Kidney Infection; ICU: Intensive Care Unit; NF: Necrotizing Fasciitis; SSI: Surgical Site Infection; SII: Superficial Incisional Infection; SSTI: Skin and Soft-Tissue Infection; DII: Deep Incisional Infection; DTI: Deep Tissue Infection; GI: Gastrointestinal; MD: Mean Deviation; BMI: Body Mass Index; THA: Total Hip Arthroplasty; MR: Mendelian Randomization; RR: Relative Risk; IFP: Infection Following A Procedure; IMN: Intramedullary Nailing; FSR: Fractional Synthesis Rates; PLE: Protein-Losing Enteropathy; CMP: Comprehensive Metabolic Panel; BUN: Blood Urea Nitrogen; IV: Intravenous; OR: Odds Ratio; CI: Confidence Interval
Introduction
Advance organizer - please answer true or false to the following questions:
1. Hypoalbuminemia is an indicator of inadequate nutrition intake that can only be relieved by nutritional support. FALSE
2. Patients with hypoalbuminemia who undergo orthopaedic surgery may be at increased risk for postoperative surgical infection and increased mortality and morbidity. TRUE
3. There is a strong correlation between the level of nutrition intake and serum albumin level. FALSE
4. Diminished synthesis of albumin is the trigger of hypoalbuminemia in malnourished patients. FALSE
5. Numerous adverse surgical outcomes are associated with hypoalbuminemia. TRUE
6. An albumin level <3.5g/dL has an almost 2.5 fold increased risk of SSI in orthopaedic surgery. TRUE
Albumin
Albumin is one of the most important serum proteins distributed in the bloodstream, the interstitial space and cells in humans, providing essential physiologic functions in the body. Synthesized in the liver, the average adult liver produces approximately 15g a day (200mg/kg per day) of which approximately 300 to 500g a day is distributed in the body fluids [1]. Thus, a normal albumin level in the blood ranges from 3.5g/dL to 5g/dL.
Among the essential physiological functions of albumin, the most important ones include, (1) maintaining oncotic pressure (osmotic pressure generated by large molecules, especially proteins, in a blood vessel’s plasma (blood/liquid) that causes a pull on fluid back into the capillary), (2) transporting various agents (fatty acids, bile acids, cholesterol, metal ions and drugs), (3) tracking free oxygen radicals, (4) acting as a most important antioxidant, and (5) exerting an antiplatelet effect [2,3]. In addition, albumin is associated with providing a value for identifying potential risk of surgical postoperative infection, and when stratified for age and gender, there is a highly significant correlation between serum albumin level and mortality risk [4].
Hypoalbuminemia
In contrast, hypoalbuminemia is defined by an intravascular albumin level of <3.5g/dL. Often observed in hospitalized patients, hypoalbuminemia has long been associated with suboptimal postoperative clinical outcomes [5]. In adult surgical patients, hypoalbuminemia has a strong predictive value on mortality and morbidity [6,7].
Common Causes of Hypoalbuminemia
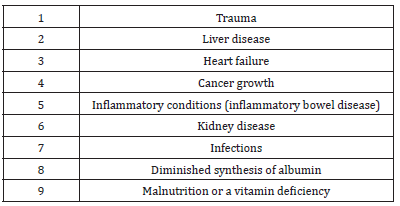
Hypoalbuminemia is often associated with various disorders including cirrhosis, malnutrition, and nephrotic syndrome. In addition to these disease states, other conditions, including major surgery, trauma, cancer growth, inflammation, infection and sepsis can affect the concentration of serum albumin. Decreased hepatic (liver) synthesis, increased leakage into the interstitial compartment (fluid-filled space between cell membranes and organs in the body) and persistent catabolism (degradation of enzymes) caused by these disorders and conditions can lead to hypoalbuminemia [6,8].
The cause of low serum albumin may be the result of decreased production of albumin in the liver. While decreased production of albumin is rare, it may present in significant and severe chronic hepatic impairment as hypoalbuminemia is a feature of chronic and advanced liver cirrhosis. Most commonly, inadequate synthesis of albumin is the presence of increased catabolism due to significant systemic illness that contributes to overall hypoalbuminemia [9]. Increased loss of albumin can occur through the kidneys, Gastrointestinal (GI) tract or gut, skin or extravascular space (3-space loss), burns and sepsis. Amino acids from the liver synthesize albumin allowing normal levels of serum albumin to maintain the colloid osmotic pressure of plasma and prevent the development of tissue edema [6,8]. Many conditions (e.g., major surgery, trauma, and infection), however, can affect the concentration of serum albumin leading to reduced hepatic synthesis, increased leakage into the interstitial compartment and persistent catabolism [6,8]. Albumin and critical illness, and cardiac failure can lead to decreased production of albumin. A combination of two or more of these mechanisms can lead to decreased production of albumin [9]. The administration of exogenous albumin usually corrects the cause of hypoalbuminemia in critical illness [3].
Hypoalbuminemia is seen in Kwashiorkor (a severe form of protein-energy malnutrition) resulting in nutritional deficiency that presents in infants and children. Low serum albumin levels occur due to a decreased supply of amino acids to the liver as well as other dietary deficiencies, notably iron and zinc [9]. Very low or undetectable serum albumin (<1g/L) characterizes a rare disorder known as analbuminaemia. Under normal conditions, individuals with this condition appear to have sufficient amounts of albumin to survive. They present in adulthood with peripheral edema, fatigue and hyperlipidemia but usually have no associated atherosclerosis and are hemodynamically stable [9].
In clinical practice, inflammatory conditions are often associated with hypoalbuminemia [4]. Although not extensively studied, existing studies reveal a correlation between severe inflammatory disorders (e.g., trauma and sepsis) and progressively lower serum albumin levels. After severe trauma or in severely septic patients, immune cells and platelets swell, causing a persisting positive fluid balance and decreasing serum albumin levels, leading to grave or fatal consequences [4]. Correction of this progression, thereby allowing for a reversal of the condition, requires shifting to a negative fluid balance (polyuria) and increasing serum albumin levels [4]. In critically ill patients, (e.g., severe burn injury or those with liver cirrhosis), exogenous albumin therapy is widely used to correct this cause of hypoalbuminemia [3]; (Table 1).
Table 1:Common causes of hypoalbuminemia.
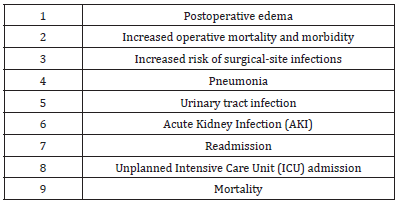
Hypoalbuminemia and postsurgical infection
In surgery, an association between hypoalbuminemia and adverse outcomes relating to postoperative infection is well established. In orthopaedic surgery, the presence of serum albumin <3.5g/dL is associated with numerous complications that account for the detrimental consequences of postoperative infection [10]. Some of these postsurgical outcomes may include, (a) impaired wound healing, (b) prolonged hospitalization, (c) higher complication rates, and (d) possible systemic infection (leading to), (e) higher mortality and morbidity, and (f) increased health care burden [11]; (Table 2).
Table 2:Adverse surgical outcomes associated with hypoalbuminemia.
Surgical Site Infection (SSI)
A Surgical Site Infection (SSI) is one type of postoperative infection and a common complication in orthopedic patients. As defined by the Centers for Disease Control (CDC) [12], a surgical site infection is one that occurs after surgery (postoperatively) in the part of the body where the surgery took place. SSIs can sometimes be superficial infections involving the skin only. Other SSIs are more serious and may involve tissues under the skin, organs, or implanted material. (CDC provides guidelines and tools to the healthcare community to help end surgical site infections and resources to help the public understand these infections and take measures to safeguard their own health when possible.)
Superficial Incisional Infection (SII):A superficial incisional infection (SII) occurs just in the area of the skin where the incision was made [12,13].
Skin and Soft-Tissue Infection (SSTI):Skin and Soft-Tissue Infections (SSTIs), which include infections of skin, subcutaneous tissue, fascia, and muscle, encompass a wide spectrum of clinical presentations, ranging from simple cellulitis to rapidly progressive necrotizing fasciitis [13,14]. Diagnosing the exact extent of the disease is critical for successful management of a patient with a soft-tissue infection [14].
Deep Incisional Infection (DII):A Deep Incisional Infection (DII) occurs beneath the incision area in muscle and tissue surrounding the muscles [13,14]. This type of infection, known as an organ or space SSI, can be in any area of the body other than skin, muscle and surrounding tissue that was involved in the surgery [14].
Deep Tissue Infection (DTI):Less commonly, the infection can spread to the deep layer of tissue called the fascial lining and is referred to as a deep tissue infection (DTI) [14]. Necrotizing fasciitis (NF) is an example of a deep-layer infection and is an extreme emergency [14]. Recurrent episodes of cellulitis may damage the lymphatic drainage system and cause chronic swelling of the affected limb [13].
Hypoalbuminemia and sepsis
Hypoalbuminemia frequently accompanies sepsis (a severe blood infection) [13,15]. Sepsis is defined as the presence of infection together with systemic inflammatory response syndrome (SIRS, diagnosed when two or more of the following criteria are met: body temperature <36 °C or >38 °C; heart rate >90 beats/ min; tachypnea >20 breaths/min, or an arterial partial pressure of carbon dioxide <32mmHg; white blood cell count less than 4 × 109/L or greater than 12 × 109/L, or the presence of >10% immature neutrophils) [15]. Sepsis plus sepsis-induced organ dysfunction or tissue hypoperfusion is indicative of severe sepsis [16,17]. Severe sepsis plus hypotension not reversed by fluid resuscitation suggests septic shock [16,17].
Related orthopaedic studies
Some suggest that preoperative hypoalbuminemia (serum albumin <3.5g/dL) is an independent risk factor for postoperative SSI in patients undergoing a spinal fusion [18]. A meta-analysis of 112,183 patients undergoing spinal fusion surgery involving 13 studies compared an infection group to a non-infection group of orthopaedic surgery patients [10]. The pooled mean deviation (MD) of albumin between the infection group and the non-infection group was MD = -2.28 (95% CU -3.97 – 0.58) which was statistically significant (z = 2.63, P = 0.0008). The pooled Relative Risk (RR) of infection when comparing albumin <3.5 with albumin >3.5 was 2.39 (95% CI 1.57 3.64), which was significantly significant P < 0.001. The conclusions of this study determined that an albumin level <3.5g/dL had an approximately 2.5 times increased risk of SSI in orthopaedics [10], and these outcomes were statistically significant, P <0.05 [10].
A study of N= 437 patients with femoral neck fractures examined the value of serum albumin estimations on admissions. Noting that antibiotic prophylaxis may reduce the rate of postoperative infection after peritrochanteric fractures [19], and that the incidence of deep wound infection after operation had not been established for femoral neck fractures [20], it was not known whether such prophylaxis was essential. The researchers looked at the incidence of deep wound infection after surgery to repair femoral neck fractures and identified variables that might affect the rate of infection. They concluded that while serum albumin is a good predictor of mortality, and low albumin levels warrant additional nutritional support in patients with hypoalbuminemia, serum albumin was not particularly useful in predicting deep wound infection [20]. Additionally, while the reported rate of infection after hip fracture surgery in general varied from 2% to 17%, [19,21] their deep wound infection rate was low, at 3%, indicating that an infection rate of 3% did not warrant the use of antibiotic prophylaxis in this population [20].
A study (part of a National Surgical Quality Improvement Program) directed at health care reform in clinical practice looked at improving outcomes and minimizing complications in patients with morbid obesity and hypoalbuminemia who underwent Total Hip Arthroplasty (THA). Between 2006 and 2013, researchers identified 49,475 patients undergoing total hip arthroplasty (THA). Patients with morbid obesity (Body Mass Index [BMI] 18.5-40kg/ m (2) were compared with nonmorbidly obese patients. Patients with hypoalbuminemia (serum albumin <3.5g/dL) were compared against those with normal albumin levels. The researchers reported that hypoalbuminemia is a significant risk factor for mortality and major morbidity among patients undergoing Total Hip Arthroplasty (THA) while morbid obesity was only associated with an increased risk of superficial surgical site infection [22]. Patients with hypoalbuminemia carried a 5.94-fold risk of 30-day mortality, P<0.01 [22].
In a retrospective cohort study of geriatric patients (>65 years of age) with hip fractures who met inclusion criteria, the status of hypoalbuminemia predicted postoperative complaints for patients with hip fractures [23]. Outcomes compared patients with and without hypoalbuminemia. Of 29,377 geriatric patients, a significant number (P<0.01) 17,651 (60.1%) had serum albumin available for analysis. The researchers looked at serum albumin levels and associations with death, specific postoperative complications (e.g., pneumonia), lengths of hospital of stay and readmission rates following geriatric hip fracture. They found that in comparison with patients with normal albumin concentration, patients with hypoalbuminemia had higher rates of death, sepsis and unplanned intubation [23]. The mean length of stay was longer among patients with hypoalbuminemia compared to those with normal albumin levels. The rate of readmission between the two groups did not differ.3Based on these findings, the researchers opined that hypoalbuminemia is a powerful independent risk factor for mortality following a surgical procedure for geriatric hip fracture, recommending further investigation into postoperative management for the patients with hypoalbuminemia [23].
Utilizing a National Surgical Quality Improvement Program database identified by the American College of Surgeons, 20,278 patients with hip fractures and available serum albumin levels were evaluated using multivariate logistic regression analysis.
The results revealed that hypoalbuminemia was predictive of readmission, reintubation, mortality and length of hospital stay.
The researchers concluded that if assessed preoperatively, based on the fracture pattern, the albumin level might guide surgical decision-making in equivocal cases where multiple modalities are used [24]. This study also asserted that compared with other interventions, intramedullary nailing (IMN) was associated with fewer postoperative complications in patients with hypoalbuminemia [24].
In a retrospective cohort study utilizing the American College of Surgeons National Surgery Quality Improvement database, the effect of malnutrition (using admission serum albumin levels as a marker for malnutrition) following surgery for distal radius fractures, was examined [25]. As denoted by hypoalbuminemia, the investigators asserted that malnutrition was associated with detrimental effects on outcomes after surgeries involving arthroplasty, geriatric hip fractures, and multiple general surgeries [25]. Noting that while there were considerable studies on hypoalbuminemia in the critically ill population, hypoalbuminemia in the orthopaedic literature (i.e., trauma) was less studied, and therefore warranted evaluation. The researchers identified 9,274 patients in the database who underwent operative fixation of a distal radius fracture between 2007 and 2015. Of this population, they identified 1,989 patients between the ages of 18-90 years old (mean age 56 years range) with available albumin levels of which 14.7% had hypoalbuminemia (albumin <3.5g/dL). Multivariant regression revealed that patients with hypoalbuminemia (whom they designated as malnourished), had higher rates of postoperative complications (6.5% v 1.3%, odds ratio [OR], 4.88; 95% confidence interval [95% CI]. 2.47-9.66, P < 0.01) [25]. These included life-threatening complications, readmission, increased lengths of stay and mortality. Based on these results, they concluded that hypoalbuminemia is an independent risk factor for 30-day mortality, postoperative complications, readmission and reoperation in the operative lower extremity orthopaedic trauma patient [25].
A more recent study looked at albumin and infection following a surgical procedure [11] using a two-sample Mendelian Randomization (MR) analysis. The investigators acknowledged that Infection Following a procedure (IFP) has detrimental consequences including impairment of wound healing, prolonged hospitalization, higher complication rates and in some cases, systemic infection, leading to considerable morbidity and mortality for patients, and immense burden on the healthcare system [11]. In addition, they noted the importance of identifying risk factors and existing preventative measures to minimize the development of the IFP. Referencing other retrospective cohort studies that reported albumin as an independent risk factor for infection, their results did not support the causal effect of albumin on infection following a procedure [11]. The investigators went on to question the benefits of perioperative albumin supplementation and recommended additional studies with more randomized control trials [11]. Thus, based on the conclusions of this study, the predictive value of serum albumin level on SSI was determined to be equivocal and inconclusive, although remaining an important prognostic indicator [11].
Hypoalbuminemia and malnutrition
Serum albumin is the most established serum marker of malnutrition and disease, with a serum albumin concentration <3.5g/dl suggestive of malnutrition. Malnutrition has links with serious complications in orthopaedics but up to 50% of cases of pre-existing malnutrition are underrecognized in the hospital population (explained by reasoning that observable signs of malnutrition appear only in extreme cases) [10]. Although uncomplicated undernutrition (not combined with inflammation) generally does not lead to lower serum albumin levels (or if it does, only very modestly), in areas with endemic malnutrition, undernutrition is usually associated with infectious or noninfectious inflammation [4].
Contrary to the accepted belief that diminished synthesis of albumin in malnourished or stressed individuals leads to malnutrition-associated hypoalbuminemia, in most disease states where synthesis rates are actually measured, Fractional Synthesis Rates (FSR) in plasma are normal or only mildly increased [4]. The synthesis rate can double in situations where there is rapid albumin loss or a fall in the serum albumin concentration [1].
In addition to synthesis rates, another factor often overlooked that influences total serum albumin mass in the body is the halflife of serum albumin. The half-life of a drug is the time taken for the plasma concentration of a drug to reduce to half its original value. In other words, half-life is an estimation of how long it takes to eliminate a drug from the body. While synthesis rates in the plasma of healthy individuals generally increase after nutritional support, it remains uncertain whether synthesis rates in the plasma of critically ill or septic patients similarly increase after nutritional support. Thus, although commonly perceived as an indicator of inadequate nutritional intake in which hypoalbuminemia is relieved by nutritional support alone, a poor correlation exists between the level of nutrition intake and the serum albumin level [4]. Therefore, rather than seeing this as a correlation between serum albumin levels and undernutrition as such, some suggest that viewing hypoalbuminemia as a reflection of the extent of physiologic stress resulting from disease or trauma-related inflammation, is more accurate [4].
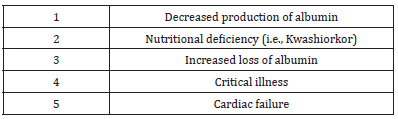
Pathogenesis of hypoalbuminemia
While the pathogenesis of hypoalbuminemia is not particularly well defined, low serum albumin is largely a function of increased vascular permeability (a conclusive response in the progress of inflammation) and increased interstitial volume (excess edema formation causing swollen tissue) [9]. These increases can affect the diffusion distance for oxygen and other nutrients leading to compromise of the cellular metabolism in the swollen tissue [4]. Thus, acknowledging the role of inflammation in mediating these responses in both pathologic states related to surgery, trauma and infection and in life stressor events such as pregnancy, lactation and cancer growth is essential to understanding the pathogenesis of underlying hypoalbuminemia [4].
Identifying the potential cause of low serum albumin may provide clues to the particular pathogenesis of hypoalbuminemia. If the cause is inadequate synthesis of albumin, the presence of increased catabolism due to significant systemic illness often contributes to overall hypoalbuminemia [9]. Increased loss of albumin can occur through the kidneys, gastrointestinal (GI) tract or gut, skin or extravascular space (3-space loss), burns and sepsis. Amino acids from the liver synthesize albumin allowing normal levels of serum albumin to maintain the colloid osmotic pressure of plasma and prevent the development of tissue edema [6,8]. Many conditions (e.g., major surgery, trauma, and infection) can affect the concentration of serum albumin leading to reduced hepatic synthesis, increased leakage into the interstitial compartment and persistent catabolism [6,8]. Albumin and critical illness, and cardiac failure can lead to decreased production. Additionally, a combination of two or more of these mechanisms may lead to hypoalbuminemia [9]; (Table 3).
Table 3:Pathogenesis of hypoalbuminemia.
Prevalence of hypoalbuminema
The prevalence of hypoalbuminemia is highest among hospitalized, critically ill and elderly patients [9]. Several studies report the incidence of hypoalbuminemia is as high as 60-80% in critically ill patients [6,26]. One report by Brock et al. [27] determined the prevalence in elderly hospitalized patients is greater than 70% [27].
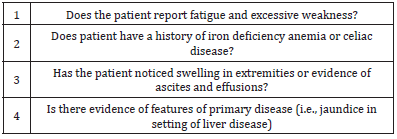
Clinical presentation of hypoalbuminemia
Clinical evaluation of patients with hypoalbuminemia may reveal reported fatigue, weak muscle tone, jaundice (yellowish discoloration of skin or eyes caused by liver disease, bile duct obstruction or abnormal breakdown of red blood cells), swelling in legs and feet, dark colored urine and/or frequent urination, shortness of breath or difficulty breathing and loss of appetite. Patients may report fatigue and excessive weakness and other features of related nutritional deficiencies, for example, iron deficiency anemia in celiac disease.
History and physical examination
History may provide important information about the potential for exposure to known causes of hepatic injury such as drug therapy, surgical and anesthetic procedures, and toxins or infectious agents. Patients may report fatigue and excessive weakness and other features of related nutritional deficiencies. For example, iron deficiency anemia in Celiac disease.
On physical examination, evaluation of the sclera, oral mucous membranes and skin for jaundice (yellowing) is important. Patients may present with features of the primary disease, for example, jaundice in liver disease or diarrhea due to Protein-Losing Enteropathy (PLE). PLE occurs when albumin and other protein rich materials leak into the intestine. Evidence of bleeding in the skin and mucous membranes or pallor may be indicative of acute blood loss anemia. Patients with hypoalbuminemia can present with peripheral (pitting) edema and central edema (ascites and effusions) and anasarca (condition that leads to general swelling of the body). (Table 4).
Table 4:Hypoalubminemia specific evaluation questions to ask.
Associated risk factors for hypoalbuminema
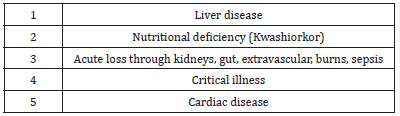
Risk factors for hypoalbuminemia include acute trauma, inflammatory conditions, infectious disease, vascular abnormalities, gynecologic and space occupying lesions, dormant activities (sedentary lifestyle) and female gender. Potential risk factors for hypoalbuminemia include liver disease, conditions with nutritional deficiency, acute loss through kidneys, gut, burns, critical illness and cardiac disease [4,9]; (Table 5 & 6).
Table 5:Risk factors for hypoalbuminemia.
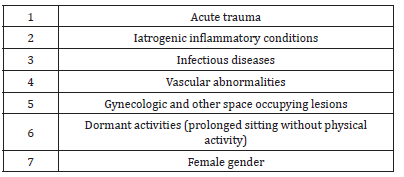
Table 6:Potential risk factors for hypoalbuminemia.
Laboratory testing
Clinical suspicion of the underlying disease process should guide appropriate lab studies [28]. Hypoalbuminemia is often a finding on routine laboratory testing with a Comprehensive Metabolic Panel (CMP) at which time patients present for routine testing or other primary medical conditions or diseases.
Measurement of serum albumin using routine assays on automated chemistry analyzers is a quick and simple method of determining the presence of hypoalbuminemia. The color change that occurs when albumin binds to a particular dye measured spectrophotometrically provides the basis of assays. Other methods used to measure albumin include immunoephelometric and immunoturbidometric techniques [9].
Evaluation of the urine with a urine dipstick for proteinuria is useful to detect the presence of proteinuria. Known also as albuminuria, evidence of protein in the urine is not a disease but rather a symptom of various conditions that can affect the kidneys.
In malnutrition, laboratory results generally show decreased lymphocyte count and Blood Urea Nitrogen (BUN) levels. Transferrin, prealbumin, and retinol-binding protein have shorter half-lives compared with albumin and better reflect short-term changes in nutritional status than albumin, which has a long halflife.
Diagnostic imaging
Imaging studies as appropriate assist to seek infectious causes of inflammation and hypoalbuminemia [28-31]. For example, if clinically warranted, chest radiography is important to rule out an infectious process or inflammation in the chest.
Management of Hypoalbuminemia
Management of hypoalbuminemia should focus on correcting the causes of ongoing inflammation rather than by the infusion of albumin [4]. Thus, the cause of hypoalbuminemia directs the treatment since it is a consequence of some disease or medical condition. In the critically ill patient, such as burn patients, albumin infusions may be given. It is controversial whether albumin infusions are of clinical benefit to other groups of critically ill patients. Albumin infusions also have some value in patients with cirrhosis with certain complications [9].
Discussion
While a direct cause and effect between low albumin levels and adverse surgical outcomes appears to exist, interventions designed solely to correct preoperative hypoalbuminemia, in particular intravenous (IV) albumin infusion, do little to change a patient’s course of hospitalization. Surgeons may use albumin levels on admission for their prognostic value, but experts recommend against using therapeutic strategies whose main endpoint is correction of this abnormality [5].
Hypoalbuminemia can be a powerful predictor of acute postoperative course and mortality in certain orthopaedic populations (i.e., after surgical fixation in nongeriatric, lower extremity orthopaedic trauma patients) [7]. Admission albumin should be a routine part of the orthopaedic trauma and other related presurgical evaluation. However, research into the utility of albumin supplementation as a modifiable risk factor prior to orthopaedic surgery is lacking, and additional research in this area would be helpful.
In patients with hip fractures, hypoalbuminemia may be a predictor for postoperative complications and, if utilized preoperatively, used as a guide to surgical decision-making in equivocal cases were based on fracture pattern, multiple surgical modalities are under consideration. For example, the use of IMN is associated with fewer postoperative complications in patients with hypoalbuminemia compared with other interventions [24].
Conclusion
In surgical patients, albumin levels may have prognostic value on admission to the hospital, and as a predictor of acute postoperative course and mortality in certain populations. However, experts advise against utilizing albumin levels as therapeutic strategies whose main objection is correction of this abnormality. As an indicator of malnutrition intake, studies actually reveal a poor correlation between the level of nutrition intake and a low albumin level corrected solely by nutritional support. Thus, some suggest that rather than focusing on a correlation between serum albumin levels and undernutrition per se, it may be more accurate to view hypoalbuminemia as a manifestation of the extent of physiologic stress resulting from disease or trauma-related inflammation.
References
- Friedman L (2022) Tests of the liver’s biosynthetic capacity (e.g., albumin, coagulation factors, prothrombin time). Literature review current through.
- Levitt D, Levitt M (2022) Human serum albumin homeostasis: a new look at the roles of synthesis, catabolism, renal and gastrointestinal excretion, and the clinical value of serum albumin measurements. Int J Gen Med (15) 9: 229-255.
- Paar M, Rossmann C, Nusshold C, Wagner T, Schlagenhauf A, et al. (2017) Anticoagulant action of low, physiologic, and high albumin levels in whole blood. PLoS One 12(8): e0182997.
- Soeters P, Wolfe R, Shenkin A (2019) Hypoalbuminemia: pathogenesis and clinical significance. J Parenteral and Enteral Nutrition (43)2: 181-193.
- Kim S, McClave S, Martindale R, Miller K, Hurt R (2019) Hypoalbuminemia and clinical outcomes: what is the mechanism behind the relationship? Am Surg 83(11): 1220-1227.
- Gatta A, Verardo A, Bolognesi M (2012) Hypoalbuminemia. Intern Emerg Med 3: S193-199.
- Gibbs J, Cull W, Henderson W, Daley J, Hur K, et al. (1999) Preoperative serum albumin level as a predictor of operative mortality and morbidity. Arch Surg 134(1): 36-42.
- Nicholson J, Wolmarans M, Park G (2000) The role of albumin in critical illness. Br J Anaesth 85(4): 599-610.
- Gounden V, Vashisht R, Jialal I (2022) Hypoalbuminemia. Stat Pearls Treasure Island (FL): Stat Pearls Publishing.
- Yuwen P, Chen W, Lv Hongzzzhi, Feng C, Li Yansen, et al. (2017) Albumin and surgical site infection risk in orthopedics: a meta-analysis. BMC Surg 17(1): 7.
- Tang Y, Wei F, Yu M, Zhou H, Wang Y, et al. (2022) Albumin and infection following a procedure: a Mendelian Randomization study.
- Surgical site infection.
- Infection After Surgery? Texas Infectious Disease Institute.
- Singhal H. Skin and soft tissue infections- Incision, Drainage, and Debridement.
- Sun J, Sun F, Wang X, Yuan S, Zheng S, et al. (2015) Risk factors and prognosis of hypoalbuminemia in surgical septic patients. PeerJ 3: e1267.
- Dellinger R, Levy M, Carlet J, Bion J, Parker M, et al. (2008) Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 36(1): 296-327.
- Dellinger R, Levy M, Rhodes A, Annane D, Gerlach H, et al. (2013) Surviving sepsis campaign guidelines committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41(2): 580-637.
- Adogwa O, Martin JR, Huang K, Verla T, Fatemi P, et al. (2014) Preoperative serum albumin level as a predictor of postoperative complication after spine fusion. Spine (Phila Pa 1976) 39(18): 1513-1519.
- Tengve B, Kjellander J (2022) Antibiotic prophylaxis in operations on trochanteric femoral fractures. JBJS 60(1): 97-99.
- Hedstrom M, Grondal L, Ortquist A, Dalen N, Ahl T (1998) Serum albumin and deep infection in femoral neck fractures. International Orthopaedics 22: 182-184.
- McQueen M, Littlejohn M, Miles R, Hughes S (1990) Antibiotic prophylaxis in proximal humerus femoral fractures. Injury 21(2): 104-106.
- Walls J, Abraham D, Nelson C, Kamath A, Elkassabany N, et al. (2015) Hypoalbuminemia more than morbid obesity is an independent predictor of complications after total hip arthroplasty. J Arthoplast 30(12):2290-2295.
- Bohl D, Shen M, Hannon C, Fillingham Y, Darrith B, et al. (2017) Serum albumin predicts survival and postoperative course following surgery for geriatric hip fracture. JBJS 99(24): 21110-21118.
- Ryan S, Politzer C, Fletcher A, Bolognesi M, Seyler T (2018) Preoperative hypoalbuminemia predicts short-term outcomes for hip fracture surgery. Orthopedics 41(6): 789-796.
- Wilson J, Lunati M, Grabel Z, Staley C, Schwartz A, et al. (2019) Hypoalbuminemia is an independent risk factor for 30-day mortality, postoperative complications, readmission, and reoperation in the operative lower extremity orthopaedic trauma patient. J Orthop Trauma 33(6): 284-291.
- Aguayo-Becerra O, Torres-Garibay C, Dassaejv M, Macías-Amezcua, Fuentes-Orozco C, et al. (2013) Serum albumin level as a risk factor for mortality in burn patients. Clinics 68(7): 940-945.
- Brock F, Bettinelli L, Dobner T, Stobbe J, Pomatti G, et al. (2016) Prevalence of hypoalbuminemia and nutritional issues in hospitalized elders. Rev Lat Am Enfermagem 24: e2736.
- Peralta R (2022) Hypalbuminemia workup. Medscape.
- Mbagwu C, Sloan M, Neuwirth A, Baldwin K, Kamath A, et al. (2019) Albumin as a Predictor of Total Joint Arthoplasty Complications: A Systematic Review. University of Pennsylvania Orthopaedic Journal 29: 150-163.
- Cellulitis, symptoms and causes. Mayo Clinic, USA.
- Sun J, Sun F, Wang X, Yuan S, Zheng S, et al. (2015) Risk factors and prognosis of hypoalbuminemia in surgical septic patients. PeerJ. 3: e1267.
© 2022 Michelle J Lespasio. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






