- Submissions

Full Text
Orthopedic Research Online Journal
Functional Outcome of Primary Total Hip Arthroplasty
Ahmad Zeb1, Farmanullah Khan2*, Sabir Khan khattak3, Akhtar Husain4, Shehryar Khan2 Muhammad Shoaib Khan5 and Khalid Iqbal4
1Consultant Orthopedic Surgeon, Khyber Teaching Hospital Peshawar, Pakistan
2Medical Officer, Khyber Medical Collage Peshawar, Pakistan
3Trainee Medical Officer, Hayatabad Medical Complex Peshawar, Pakistan
4Senior Registrar orthopedics Peshawar Medical Collage Peshawar, Pakistan
5Professor & Chairman Department of Orthopedics, Khyber Teaching Hospital Peshawar, Pakistan
*Corresponding author: Farmanullah Khan, Medical Officer, Khyber Medical Collage Peshawar, 25120, Pakistanc
Submission: October 11, 2022;Published: October 19, 2022

ISSN: 2576-8875 Volume10 Issue2
Abstract
Background: Being a synovial joint hip can have a number of end stage diseases like primary osteoarthritis, secondary osteoarthritis, and avascular necrosis of femoral head. Total hip replacement is the ultimate treatment for end stage diseases of hip to improve hip functions and relieve pain. To evaluate functional outcome of artificial hip joint postoperatively, Harris hip score is used.
Method: This prospective study was carried out in Khyber Teaching Hospital Peshawar, Pakistan from January 2018 to January 2022. 96 patient of age group 30 years and above of both gender with total hip arthroplasty for end stage osteoarthritis of hip (both primary and secondary to trauma) and osteonecrosis who fulfilled the inclusion/ exclusion criteria were included in the study. Age, sex, site, operative indication and pre-operative Harris Hip Score were documented. Uncemented total hip replacement was done. Postoperative Harris hip score was documented at 3 months after surgery.
Results: Among total 96 patients 58.33% were male and 41.67% where females with age rang 30 to 76 years. Avascular necrosis of hip (44%), primary osteoarthritis (36%), secondary osteoarthritis due to trauma (30%), and sequel of hip infection (20%) were indication of surgery. Preoperative Harris Hip Score ranged from 20 to 50 and it ranged from 70 to 95 at 3 months after surgery. Postoperatively Harris hip score were excellent in 80%, good in 12% while fair in 8% patients. Only 6.25% cases developed complications, 2 (2.08%) skin incision site infections and 4(4.17%) dislocations.
Conclusion: Total hip replacement is an excellent function preserving and pain-relieving procedure for end stage diseases of hip joint with less number of complications.
Abbreviations: Harris hip score; Total hip arthroplasty; Osteoarthritis hip; Avascular necrosis hip
Introduction
Hip joint is a synovial joint having ball and socket mechanism [1]. A number of diseases can destroy this joint including osteoarthritis (both primary and secondary), avascular necrosis of femoral head, inflammatory diseases, congenital diseases, trauma, and joint infections. All these conditions lead to end stage arthritis. Unbearable pain may result due to end stage arthritis of the hip which greatly restrict daily living activities. When all the conservative measure fails to manage end stage arthritis of hip then hip joint replacement or arthroplasty is indicated [2,3].
Total hip replacement or arthroplasty is the reconstruction of articular surfaces to relieve hip joint pain, improve hip functions and restore hip movements. It is the restoration of the ball and socket mechanism surgically by replacing the involved femoral head as well as the acetabulum. In case of end stage arthritis of hip, total hip replacement is the most beneficial surgical procedure [4,5]. It is having 85% survival rate over 20 years [6].
Majority of patients are having improvement in hip pain, improved functions, and better quality of life after total hip replacement on one hand while on the hand there are also some patients who claim no or less improvement in these parameters postoperatively. Some 30% of patients experience significant daily activity disturbances post hip replacement at 2 years interval. The exact mechanisms for these functional limitations of total hip surgery are not clearly understood [7]. To assess hip functions both preoperatively and post surgically, a number of functional assessment tools are developed. Harris Hip Scoring (HHS) system is one of these tools [8].
In current era total hip arthroplasty procedure is performed in most of the centers in our country but we are still facing many challenges like lack of dedicated operative setups, expertise, specialized auxiliary staff and high rate of infection. All these shortcomings of our health system may contribute to poor functional outcomes of total hip arthroplasty. We aim to conduct this study to know postoperative improvement in patients who had undergone uncemented total hip arthroplasty, in terms of functional outcome and pain relief, using Harris hip score at 3 months postoperatively.
Methodology
This prospective study was carried out in Khyber Teaching Hospital Peshawar, Pakistan from January 2018 to January 2022. Patient of age group 30 years and above of both gender with total hip arthroplasty for end stage osteoarthritis of hip (both primary and secondary to trauma) and osteonecrosis were included in the study. Patients with hip arthroplasty for hip arthritis due to any other cause like inflammatory disease, DDH, protrusio-acetabuli, girdlestone and revision total hip replacements were excluded from the study. Total uncemented hip replacements during this period and fulfilling the inclusion/ exclusion criteria (96 patients) were included in study.
All the participants of the study were admitted in the orthopedic ward. Written consent of the patients was obtained both for surgery and their inclusion in the study after explaining them the operative procedure, its complications and purpose of the study.
Age, sex, site, disease for which total hip replacement was indicated, duration of disease and Harris Hip Score (pre-operative and post-operative) were noted. All the participants were assessed through Harris hip score preoperatively. Total Harris hip score is 100 points. Score 90-100 was termed excellent, score 80-89 was termed good, sore 70-79 was termed fair and score below 70 was termed as poor functional outcome.
All the patients were evaluated according to our hospital protocol. Modified Hardinge lateral approach was used for hip arthroplasty. Intravenous ceftriaxone 1 gm will be given before skin incision. Spinal anesthesia was used in all cases. Uncemented total hip arthroplasty was done according to standard protocol. Meticulous soft tissues closure was done in each patient. Each patient was mobilized on second day of surgery with the help of crutches allowing only toe touch down for 6 weeks. Patients were sent home on 3rd postoperative day. Intravenous antibiotics were used for 7 days and changed to oral antibiotics to be used for next 7 days. Standard physiotherapy was started on 2nd postoperative day. All the participants were again assessed through Harris hip score at 3 months postoperatively. All the data obtained were recorded and analyzed by SPSS-23.
Results
Among total 96 patients with uncemented total hip arthroplasty, 56 (58.33%) were male and 40 (41.67%) were females. Age varied between 30 to 76 years with mean age of 60 years (SD = 10.42). Most of the patient were with right hip joint involvement (60%) and only 40% were having left hip joint involvement. Disease condition for which total hip arthroplasty was done were avascular necrosis of hip (44%), primary osteoarthritis (25%) and post-traumatic osteoarthritis (25%).
Figure 1:Harris hip score.
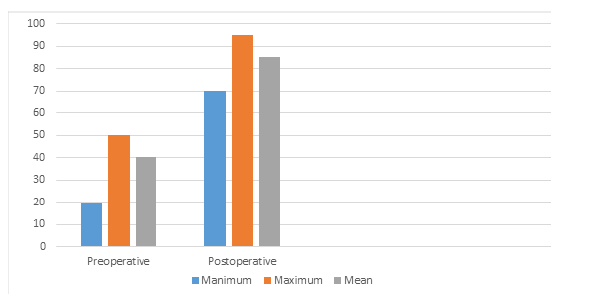
Figure 2: Postoperative harris hip score categorization.

Harris Hip Score ranged from 20 to 50 before surgery with mean 40.5 and it ranged from 70 to 95 with mean 85 at 3 months after surgery (Figure 1). The results for Harris hip score were 80% excellent, 12% were good and 8% were fair after surgery at 3 months (Figure 2).
Only 6.25% cases developed complications, 2 (2.08%) skin incision site infections and 4(4.17%) dislocations.
Discussion
Total hip replacement is a very beneficial reconstructive procedure for adults with end stage hip diseases. Besides pain relief it also restores functional anatomy of diseased hip joint, and the patients are able to gain normal or satisfactory equivalent to normal mobility. In recent era both functional capacity and durability of hip joint increased [3].
In our study the minimum age of the patients was 30 years while the maximum age of the patients was 76 years, and the average age was 60 years. The average age in a similar study of 100 patients, by Siwach R et al. was 52.56 years [9]. Sekhar C et al. observed the average age of the patient to be 59.68 year in another similar study [10]. one of these studies is having similar observations and the other one is showing quite different observations regarding patients age for total hip replacement. So, it shows that age cannot be considered as an indication for total hip replacement.
In current study the numbers of male patients 56 (58.33%) predominates the numbers of female patients 40 (41.67%). Some other similar studies are also having the same observations [10,11]. Avascular necrosis of hip (44%) was the major indication for total hip replacement, followed by primary osteoarthritis (25%) and post-traumatic osteoarthritis (25%). A study conducted by Marahatta SB et al also shows that avascular necrosis of hip (36%) and primary osteoarthritis (24%) are the is the major indications for total hip replacement [3].
Pre-operative calculation of Harris Hip Score was minimum of 20 and maximum of 50 with a mean of 40.5 while postoperatively it ranged from 70 to 95 with a mean of 85 at 3 months after surgery. Our results are having similarities with other studies conducted for functional outcomes of total hip replacement using Harris hip score. Ram GG et el studied the functional outcomes of total hip replacement of in-patient having osteoarthritis and found that the mean score before surgery was 44 and the mean score after one year of surgery was 86 [12]. Another similar study was conducted by Siddique et al Preoperatively mean Harris hip score was 41.15. It was 68.13 after one month and 78.64 after six months postoperatively [11].
We have only 6.25% cases who developed complications postoperatively. 2 (2.08%) patients developed skin incision site infections and 4(4.17%) patients were having arthroplasty hip dislocations. All these complications were conservatively managed. These results are comparable to study conducted Marahatta SB et al according to this study 2 % of patient were having superficial skin infection postoperatively and 2% of patients were having postoperative hip dislocations. All these patients were conservatively managed [3]. other complications found on literature search in similar studies are aseptic loosening, osteolysis, and symptomatic failure of both acetabular and femoral components. No such complications were found in our study. One valid reason for such complications found in these studies and absent in our study is follow up in these studies which was for years, and we determined short term functional outcome. We have no mortality and morbidity in our study like other similar studies [9,13].
Conclusion
Total hip replacement relieves pain and improves functional outcome in patients of avascular necrosis of hip and both primary and secondary osteoarthritis. It is an effective and safe procedure which can be safely opted for end stage diseases of hip as it is having very much less complication rate and with excellent functional outcome.
References
- Jafar O, Rehman A, Shaukat MK (2015) Functional outcome of total hip. J Uni Med Dent Coll 6(3): 61-69.
- Park KD, Park JB (2000) Interfacial strength of compression molded specimens between PMMA powder and PMMA/ MMA monomer solution-treated ultra-high molecular weight polyethylene (UHMWPE) powder. J Biomed Mater Res 53(6): 737-747.
- Marahatta SB, RC DR, KC KM, Sigdel A (2020) Functional outcome of primary total hip arthroplasty using harris hip score in arthritic hip. Europasian J Med Sci 2(2): 4-10.
- Kim YH, Kim JS, Park JW, Joo JH (2011) Comparison of total hip replacement with and withoutcement in patients younger than 50 years of age: the results at 18 J Bone Joint Surg 93-B: 449-455.
- Shahabud-ud-din, Ahmad I, Hayat S (2005) Cemented total hip replacement inpatients younger than fifty years of age. J Poatgraduate Medical Institute 19(4): 416-419.
- Saeed UB, Khan RD, Rehman MZ, Yasin A. (2015) Short term evaluation of total hip arthroplasty; our experience at tertiary care center. J Pak Med Assoc (Suppl.3) 65(11): 190-194.
- Buirs LD, Van Beers LWAH, Scholtes VAB, Pastoors T, Spragueet S, et al. (2016) Predictors of physical functioning after total hip arthroplasty: a systematic review. BMJ Open 6(9): e010725
- Marchetti P, Binazzi R, Vaccari V, Girolami M, Morici F, et al. (2005) Long-term results with cementless Fitek (or Fitmore) cups. J Arthroplasty 20(6): 730-737.
- Siwach R, Kadyan VS, Sangwan S, Gupta R (2007) A retrospective study of total hip arthroplasty. Indian J Orthop 41(1): 62-66.
- Sekhar AC, Mittal A, Rallapalli R, Biju, Prasad S (2015) Evaluation and outcome of total hip replacement in adults with arthritis. J Dent Med Sci 14(4): 65-72.
- Siddique T, Sah RK, Masood F, Awais SM (2015) Improvement in Harris Hip Score after cementless total hip arthroplasty in young active adults with secondary hip arthritis- a short-term follow-up result. J Pak Med Assoc 65(11 Suppl 3): S63-6.
- Ram GG, Thamodaran B, Ashok TR, Perumal S, Varthi VP (2013) Analysis of functional and radiological outcome of total hip replacements in rheumatoid and osteoarthritis patients. Open J Rheumatol Auto Dise 3(4): 720-726.
- Gupta DL, Lal DM, Aggarwal DV, Rathor DLP (2018) Assessing functional outcome using modified Harris hip score in patients undergoing total hip replacement. Inter J Orthop Sci 4(2): 1015-1017.
© 2022 Farmanullah Khan. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






