- Submissions

Full Text
Orthopedic Research Online Journal
Anatomical Three-Point Coracoclavicular Ligament Reconstruction: A Surgical Technique
Philippe Vial*, Nermine Habib*, Paolo Fornaciari, Mauro Maniglio, Moritz Tannast and Gregoire Thürig
Department of Orthopedics and Traumatology, Fribourg University Hospital, Switzerland
*Corresponding author: Philippe Vial & Nermine Habib, Department of Orthopedics and Traumatology, Fribourg University Hospital, Switzerland
Submission: September 30, 2022;Published: October 13, 2022

ISSN: 2576-8875 Volume10 Issue1
Abstract
Introduction:Acromioclavicular joint reconstruction is a frequently performed procedure for high-grade Rockwood injuries. Scientific and commercial interest has led to the development and performance of surgical techniques that more reliably restore horizontal stability to improve patient outcomes. Therefore, we have adopted a modified surgical technique. We present clinical and radiological findings from our experience at a single institution using a three-point anatomical reconstruction of the coracoclavicular ligament. We questioned (i) Quality of reduction, (ii) Complication rate, (iii) Clinical function in terms of ASES, OSS, VAS scores, (iv) Time to return to work.
Materials & Methods:Retrospective analysis of patients with acute ACL dislocation (Rockwood types III-V) from 2015 to 2019. Nineteen patients, with a mean age of 41 years, had a mean clinical and/or radiological follow-up of 20 months. The coracoclavicular distance was measured and compared on preoperative, postoperative, and follow-up radiological images. Clinical assessment was done using the above-mentioned scores. The time required to return to work was recorded..
Results: The difference in coracoclavicular distance was significant between preoperative and postoperative radiographs. Three patients showed secondary displacement of more than 5mm. Clinical evaluation performed at a mean of 20 months showed a median ASES of 98.3, OSS of 48, and VAS of 0. All patients returned to their previous jobs after a mean recovery of 11 weeks.
Conclusion:This study describes an open surgical technique for an anatomic three-point reconstruction of the CC ligaments. All patients resumed their professional activities in a timely manner. It showed promising clinical results and potential benefits. However, long-term studies are needed to show socioeconomic and clinical benefits.
Abbreviations:Acute acromioclavicular injury; Acromioclavicular dislocation; Coracoclavicular ligaments
Introduction
Acromioclavicular (AC) joint reconstruction is a frequently performed procedure for Rockwood type III or higher according to the classification [1-3]. AC joint reconstruction has been shown to prevent joint deformities and adverse outcomes, including persistent discomfort and secondary AC joint arthritis [4,5].
A multitude of surgical techniques have been described in the treatment of AC joint injuries [6-12]. The most frequently performed procedures are the modified Weaver-Dunn procedure and the anatomic reconstruction of Coracoclavicular (CC) ligaments, which may include a single or double bundle repair technique using an autograft, allograft, or synthetic ligament [13]. Although there are several comparative studies, there is still no clear consensus on which treatment method is preferable [14]..
A review by Gowd et al. [3] showed no difference in loss of reduction, complication rate, or the revision rate between open and arthroscopic AC joint reconstruction. Scientific and commercial interest has led to the development and execution of surgical techniques that more reliably restore horizontal stability to improve patient outcomes.
Anatomy
Reviewing the literature on CC ligament anatomy, we introduce
a 3-point suspension technique that can better reproduce and
reconstruct the acromioclavicular joint. We present our singleinstitution
experience using our novel three-point anatomical
reconstruction of the CC ligament. The objective of this study is to
investigate:
A. The quality of reduction
B. The rate of complications
C. Clinical function in terms of the American Shoulder and
Elbow Society Score (ASES), the Oxford Shoulder Score (OSS),
the Visual Analogue Scale (VAS)
D. The time to return to work.
Indications/contraindications
For this single-center retrospective case series, we reviewed all consecutive patients in our database who underwent AC joint stabilization with the aforementioned technique for the treatment of acute, traumatic AC joint dislocation between January 2015 and April 2019. Indications were: (1) age >18 years, (2) an acute AC dislocation of Rockwood type III-VI, (3) clinical and/or radiological follow-up of at least 1 year. Contraindications were: (1) ipsilateral concomitant fractures of the shoulder or clavicle joint, (2) pathological fractures, (3) pretraumatic functional deficit of the ipsilateral shoulder, (4) subacute injury defined as a delay of surgery up to 3 weeks after injury, and (5) patient refusal to participate in the study.
Ultimately, 19 patients (corresponding to 19 shoulders) were included in the study, 18 males and 1 female, with a mean age of 41 years (18-68).
Technique
The patient is placed in a beach-chair position. Disinfection, draping with 3M™ Ioban, and drawing of bony landmarks is performed. The approach uses a 5cm sagittal saber incision at 2cm medial to the AC joint. Special attention is paid to identifying supraclavicular nerve branches. The delto-trapezial fascia is incised longitudinally, if it has not already been traumatically torn, and two periosteal flaps are dissected. Anterior and posterior subperiosteal dissection of the clavicle is performed. The AC joint can be visualized and, if necessary, cleaned of interposed tissue or hematoma.
Identification of the CC ligament interval that is bluntly widened. Exposure of the coracoid process and identification of the CC impression on the coracoid process. A 3.5mm coracoid tunnel is drilled at a 30° angle from posterior to anterolateral with a 20° medial inclination. The coracoid Endo button™ (Smith+Nephew, Andover, MA) is mounted with two Fiber Tapes® (Arthrex, Naples, FL) and passed through the coracoid tunnel. Three clavicular tunnels are performed with a 2.5mm drill in a triangular fashion: two posterior tunnels (1 medial and 1 lateral) and one anterolateral tunnel. The Posterolateral (PL) and Posteromedial (PM) tunnels are drilled from superior to anteroinferior at a 20° angle, and the Anterolateral (AL) tunnel is created from superior to anteroinferior at a slight 0°-5° angle. The PL tunnel is then enlarged with a 3.5mm drill. One Fiber Tape® is passed from caudal to cranial through the PM and PL tunnels, respectively, and the other one through the PL and AL tunnels from caudal to cranial to be knotted over the clavicle (Figures 1-3).
Figure 1: Ventral view of the acromioclavicular joint showing the mediolateral inclination for drilling the coracoid tunnel: (thick green line) angle for drilling.
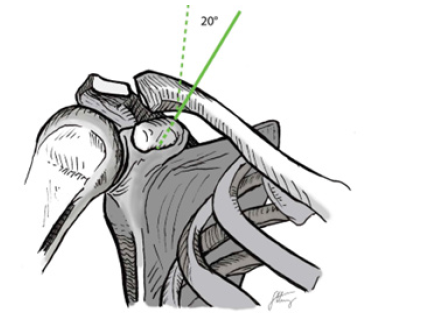
Figure 2: Cranial view of the acromioclavicular joint showing tunnel positioning: (AL) anterolateral tunnel, (PL) posterolateral tunnel, (PM) posteromedial tunnel.

Figure 3:Sagittal cuts of the clavicula showing angle to drilling: (AL) Anterolateral Tunnel, (PL) Posterolateral Tunnel, (PM) Posteromedial Tunnel, (green line) angle for drilling, (blue line) coronal reference line.

Aftercare: The shoulder is immobilized with a sling. Mobilization under the guidance of a physical therapist in the postoperative period is allowed by enabling active abduction/anteversion up to 90° without weight-bearing for 6 weeks. Then, physical therapy is prescribed to regain full range of motion and strengthening. Heavy lifting and overhead activities were limited until 12 weeks postoperatively.
Expected outcomes
Clinical analysis: Clinical follow-up was done at 6 weeks and at 3, 6, and 12 months. Clinical outcomes were documented using the American Shoulder and Elbow Society Score (ASES), the Oxford Shoulder Score (OSS), and the Visual Analogue Scale (VAS) in all patients at their last clinical follow-up. Time to return to work, complications, and revision rates were also determined. Surgical time and complications such as infection or neurovascular injury were also documented.
Radiological analysis: Radiographs of the clavicle (anteroposterior and tangential views) were collected before surgery, in the immediate postoperative period, and at 12-month follow-up. CC distance (CCD) was measured in the tangential views of the preoperative radiographs. The same distance was also measured in the immediate postoperative period and in the final radiographs. The radiographs were analyzed by two examiners (G.T. and N.H.). A loss of reduction was defined as an increase in CCD of more than 5mm on postoperative radiographs. Complications such as bone erosion, fractures, button dislocation, and heterotopic ossification were also documented.
Statistical analysis: Statistical analysis was performed using SPSS version 23.0 software (SPSS, Chicago, Illinois). The Wilcoxon Signed-Ranks test was used for qualitative data analysis. The significance level was set at p≤0.05.
Ethics: Informed consent was obtained from all patients, and all investigations were conducted in accordance with research ethics principles. The study was approved by the Ethics Cantonal Committee (CER-VD 2019-00092).
Results
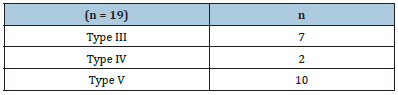
Nineteen patients (corresponding to 19 shoulders) were included in the study, 18 males and 1 female, with a mean age of 41 years (18-68). Patients had a mean clinical and/or radiological follow-up of 20 months (10-37) after AC stabilization. The mean time to surgery was 13 days (5-21) (Table 1). Of the 19 patients operated, 7 had a Rockwood III type lesion, 2 had a Rockwood IV type lesion, and 10 had a Rockwood V type lesion (Table 2). The surgery was performed by 4 surgeons (consultant level) with a mean time of 62 minutes.
Table 1:Patient demographics.
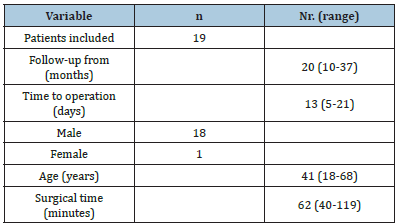
Table 2:Acromioclavicular dislocation according to rockwood classification.
Quality of reduction
Figure 4:Coracoclavicular distance at preoperative, postoperative and last control; (*) significant, (°) outliers.

The mean preoperative coracoclavicular distance was 17.2mm (4, range 9.1-25.7) while the postoperative distance was 7.6mm (2.2, range 4.4-12.2) and on the last one 10.6mm (3.6, range 5.9-20.9). Because the data was skewed for one of the variables, a Wilcoxon Signed-Ranks Test was performed, and the output indicated that postoperative scores, Mdn = 7.4, were statistically significantly lower than preoperative scores, Mdn = 17.1, Z = -3.823, p < .000, that the last control scores, Mdn = 9.9, were statistically significantly lower than preoperative scores, Mdn = 17.1, Z = -3.662, p < .000, and that postoperative scores, Mdn = 7.4, were statistically significantly lower than the last control scores; Mdn = 9.9, Z = -3.824, p < .000. (Figure 4).
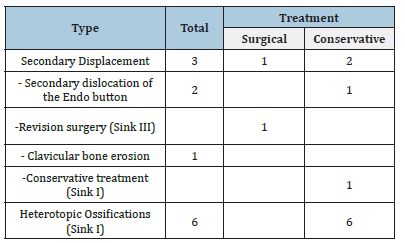
Complications
Three patients showed a secondary displacement of more than 5mm. Two of which presented with secondary dislocation of the Endo button. One of the cases was diagnosed at 6 weeks after surgery. The patient was asymptomatic and clinical examination showed no instability; therefore, revision surgery was not necessary. The second case presenting with Endo button dislocation was at 5 months postoperatively after additional trauma. Clinical examination showed anteroposterior instability. Revision surgery was performed with reconstruction using a palmaris longus graft. After rehabilitation, the patient returned to work.
The third patient presented with a loss of reduction secondary to bone loss at the clavicular site, without Endo button dislocation. Clinically, the patient showed no signs of instability and resumed all his usual activities, so no further action was taken. Heterotopic ossifications were visualized in 6 patients: all asymptomatic. No cases of infection or neurovascular injuries were reported (Table 3).
Table 3:Complications.
Clinical analysis
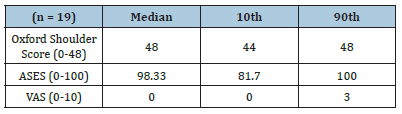
The median ASES was 98.3 (44-48; 10th-90th percentile), OSS 48 (44-48; 10th-90th) and VAS 0 (0-3; 10th-90th) (Table 4). The detailed analysis is shown in (Figure 5). The patient with the lowest scores (ASES 63, OSS 36, VAS 5) was the patient who sustained additional trauma mentioned above, requiring revision surgery with a palmaris longus graft and with a total follow-up of 19 months.
Figure 5:Scores.

Table 4:Scores.
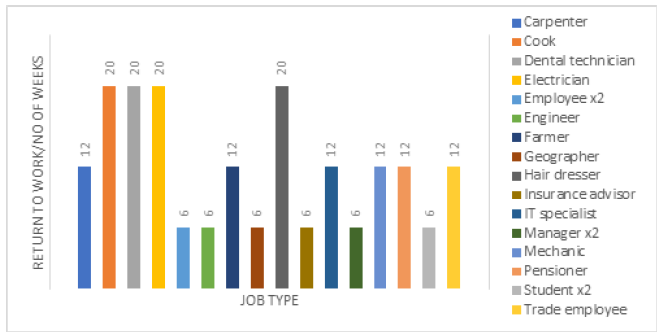
Return to work
Ten patients were manual workers and nine of them had office jobs. The mean recovery time was 11 weeks (5-20). At 6 weeks, eight patients (41.2%) returned to their previous occupation. At 12 weeks, seven more patients (78.9%) returned to their jobs, and at 20 weeks, the final four patients (100%) returned to work. One of the patients was a retiree, so the return to work was considered when he resumed all his daily activities. It was particularly noted that patients with an office job returned to work at 6 weeks after surgery, whereas manual workers at 12 to 20 weeks after surgery (Figure 6).
Figure 6:Time after surgery needed to return to employment.
Discussion
In arthroscopic and open CC reconstruction techniques, construct stability depends on a fixation point on the inferior base of the coracoid. Different combinations can be used, either a metal button, or a ring with biological graft or synthetic material around the base of the coracoid [15-18]. Even though the Weaver JK et al. [19] procedure has been considered the gold standard since its description in 1972, in recent years, the general surgical trend has shifted away from non-anatomic reconstructions towards more anatomic reconstructions [20-28]. A systematic review was able to show significantly better results of anatomic versus non-anatomic reconstruction [28]. Postoperative dislocation and last followup compared with preoperative dislocation showed a significant reduction in CCD. Although the loss of reduction at last follow-up showed statistical significance, it is still in concordance with the literature (Table 5.1).
Table 5.1:Review of the literature.

Despite attempts to recreate the native anatomy of the CC ligament with reconstruction procedures, loss of reduction is still a major problem [29,30]. In a study by Tsou [31] on CC fixation, the failure rate was 32%. Rush [32] reported a reduction loss of 39% [33]. Cook [33] reported that intraoperative reduction was lost in an average of 80% of patients, while 40% required revision and only 50% had good or excellent results. Shin [34] demonstrated that causes of failure included residual horizontal instability and excessive stress of the suture button on the bone causing osteolysis of the clavicle.
Because long-term radiographic studies with different techniques have shown a high rate of partial loss of reduction ranging from 11% to 53% [32,35-43], a slight over-reduction of 2-3mm at the time of surgery is recommended to achieve anatomic reduction thereafter [43-45]. Three cases were found with a loss of reduction of more than 5mm. Two were asymptomatic and did not need further treatment. The third experienced re-injury 5 months after the primary surgery and needed revision surgery. Regarding horizontal stability, an emerging concept is to address not only vertical instability, but also persistent horizontal instability of the AC joint. Studies have shown that persistent horizontal instability after surgical reconstruction is associated with inferior outcomes, both because of clinical instability [46], and because of pain related to the amount of anteroposterior translation [47].
Although AC ligaments and the surrounding muscles are important for horizontal stability, the CC ligaments also play an important role in providing stability in both planes. Debski et al. [48] demonstrated that in cases of complete AC ligament rupture, the conoid ligament is the main restraint against anterosuperior loading and the trapezoidal ligament is the main restraint against posterior loading. In a Magnetic Resonance Imaging (MRI) study, in addition to the AC joint capsule, the trapezoidal ligament has been shown to limit posterior translation and the conoid ligament to limit anterior translation [49].
As described in anatomical reference texts such as Testut [50] and subsequent clavicle anatomy literature the shape of the footprint on the clavicle of the ligaments is “L”, with the anteroexternal ligament, commonly the trapezoid defect developing in the sagittal plane [51-53]. For this reason, the addition of a third tunnel just anterior to the PL tunnel can recreate a condition more similar to the original anatomy and allow for better biomechanics. Several studies have discussed CC ligament reconstruction techniques focusing on clavicular attachments rather than coracoid insertions [18,26]. However, a biomechanical study by Hislop et al. [54] reported that failure occurred more frequently at the clavicle (15/22 [68.2%]) probably because the cortex of the lateral clavicle is weaker than that of the coracoid because the lateral clavicle has a metaphysis composed of cancellous bone. Other drilling techniques such as transacromial-transclavicular carry the risk of fracture of the coracoid or lateral clavicle, or of nonanatomic reconstruction [55] and therefore must be applied with care.
Although double-tunnel techniques for CC fixation were introduced to minimize the loss of reduction of the single-tunnel technique [38,42,56-58] they have been associated with an increased risk of clavicle and coracoid fracture. In the technique described by Rush et al. [32], the incidence of coracoid fractures is 11%. Several studies have suggested smaller drill holes and sufficient bone bridging to prevent this complication [32,38,56,58,59]. Meticulous attention to surgical technique can also help minimize the risk of clavicle fracture, and adequate visualization of the coracoid is essential [58]. Preoperative measurement of the total length of the clavicle is recommended to place the PM tunnel at a point between 20% and 25% of the total length of the clavicle and the lateral (trapezius) tunnel at a point less than 16% of the total length of the clavicle [38]. This series demonstrates that drilling three small clavicular and one coracoid hole with sufficient bony bridging does not result in an increased risk of fracture.
In this study, clinical outcome was measured using the ASES, the OSS, and the VAS. The ASES is based on patient responses to questions regarding joint pain, instability, and activities of daily living. It has been shown to be a valid score with excellent reliability and responsiveness. One limitation, however, is that higher functioning patients may experience ceiling effects due to the response structure [60]. The second clinical score is the OSS, a score directed at self-assessment of shoulder pain and function, with the advantage of being easy to read, understand, and interpret, and an internal consistency/cross-sectional reliability comparable to that of the DASH and limited by its rather weak validity and usability for research [61]. We also clinically assessed the patients using the VAS which is presumed to produce ratio-level data [62]. We decided to use it to avoid the possible problems caused by the use of noncontinuous, ordinal scales [63] This study shows similar results to those cited in the literature (Table 5.2).
Table 5.2:Review of the literature (2nd part).
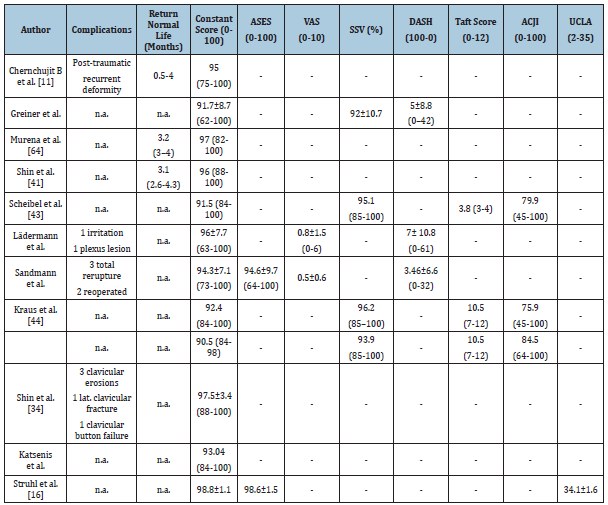
In the literature, not many studies address the issue of return to work as before surgery [41,64]. In a society where resources are finite and surgeries must also be justified in correspondence with a recovery of productive capacity, this parameter seems very relevant. An interesting finding of the present study is the very high overall rate (100%) of early return to work with an average recovery time of less than 12 weeks. This is particularly important for patients in an active population facing surgery for AC dislocation, such as manual workers. One limitation of our study is the small sample size and the fact that it was performed retrospectively. Another limitation is that radiological controls were performed with conventional radiography leaving a margin of error in the measurements. It is also difficult to compare different clinical scores with those used in a multitude of studies. The ASES has been shown to have a high correlation with Constant-Murley (CS), the University of California Los Angeles (UCLA) and the Simple Shoulder Test (SST) scores. The results obtained with this modified technique showed very good scores that are similar to those reported in the literature (Tables 5.1. & 5.2.). In our opinion, this could be due to the reproduction of a more accurate biomechanics by obtaining an anatomical reconstruction.
Conclusion
The study describes an open surgical technique for an anatomic three-point reconstruction of the CC ligaments. All patients were able to resume their professional activities in a timely manner. It showed promising clinical results and potential benefits. However, long-term studies in a larger population are needed to show socioeconomic and clinical benefits.
References
- Rockwood CJ, William GYD (1998) Disorders of the acromioclavicular joint. In: CJ R, III MF (Eds.), The Shoulder. (2nd edn), WB Saunders, Philadelphia, USA, pp. 483-553.
- Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, et al. (2013) Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 29(2): 387-397.
- Gowd AK, Liu JN, Cabarcas BC, Cvetanovich GL, Garcia GH, et al. (2019) Current concepts in the operative management of acromioclavicular dislocations: A systematic review and meta-analysis of operative techniques. American Journal of Sports Medicine 47(11): 2745-2758.
- Beris A, Lykissas M, Kostas-Agnantis I, Vekris M, Mitsionis G, et al. (2013) Management of acute acromioclavicular joint dislocation with a double-button fixation system. Injury 44(3): 288-292.
- Muench LN, Berthold DP, Uyeki C, Kia C, Cote MP, et al. (2020) Conversion to anatomic coracoclavicular ligament reconstruction (ACCR) shows similar clinical outcomes compared to successful non-operative treatment in chronic primary type III to V acromioclavicular joint injuries. Knee Surgery Sports Traumatology, Arthroscopy 29(7): 2264-2271.
- Cisneros LN, Reiriz JS(2017) Management of chronic unstable acromioclavicular joint injuries. Journal of Orthopaedics and Traumatology 18(4): 305-318.
- Scheibel M, Dröschel S, Gerhardt C, Kraus N (2011) Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. American Journal of Sports Medicine 39(7): 1507-1516.
- Sirin E, Aydin N, Topkar OM (2018) Acromioclavicular joint injuries: Diagnosis, classification and ligamentoplasty procedures. EFORT Open Reviews 3(7): 426-433.
- Wylie JD, Johnson JD, DiVenere J, Mazzocca AD (2018) Shoulder acromioclavicular and coracoclavicular ligament injuries: Common problems and solutions. Clinics in Sports Medicine 37(2): 197-207.
- Braun S, Beitzel K, Buchmann S, Imhoff AB (2015) Arthroscopically assisted treatment of acute dislocations of the acromioclavicular joint. Arthroscopy Techniques 4(6): e681-e685.
- Chernchujit B, Tischer T, Imhoff AB (2006) Arthroscopic reconstruction of the acromioclavicular joint disruption: Surgical technique and preliminary results. Archives of Orthopaedic and Trauma 126(9): 575-581.
- Salzmann GM, Walz L, Schoettle PB, Imhoff AB (2008) Arthroscopic anatomical reconstruction of the acromioclavicular joint. Acta Orthopaedica Belgica 74(3): 397-400.
- Jordan RW, Malik S, Bentick K, Saithna A (2019) Acromioclavicular joint augmentation at the time of coracoclavicular ligament reconstruction fails to improve functional outcomes despite significantly improved horizontal stability. Knee Surgery Sports Traumatology Arthroscopy 27(12): 3747-3763.
- Moatshe G, Kruckeberg BM, Chahla J, Godin JA, Cinque ME, et al. (2018) Acromioclavicular and coracoclavicular ligament reconstruction for acromioclavicular joint instability: a systematic review of clinical and radiographic outcomes. Arthroscopy 34(6): 1979-1995.
- Nicholas SJ, Lee SJ, Mullaney MJ, Tyler TF, McHugh MP (2007) Clinical outcomes of coracoclavicular ligament reconstructions using tendon grafts. American Journal of Sports Medicine 35(11): 1912-1917.
- Struhl S, Wolfson TS, Kummer F (2016) Axial-plane biomechanical evaluation of 2 suspensory cortical button fixation constructs for acromioclavicular joint reconstruction. Orthopaedic Journal of Sports Medicine 4(12): 1-6.
- Weiser L, Nüchtern JV, Sellenschloh K, Püschel K, Morlock MM (2017) Acromioclavicular joint dislocations: Coracoclavicular reconstruction with and without additional direct acromioclavicular repair. Knee Surg Sports Traumatol Arthrosc 25(7): 2025-2031.
- Wolf EM, Pennington WT (2001) Arthroscopic reconstruction for acromioclavicular joint dislocation. Arthroscopy 17(5): 558-563.
- Weaver JK, Dunn HK (1972) Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. The Journal of bone and joint surgery American volume 54(6): 1187-1194.
- Haber DB, Spang RC, Sanchez G, Sanchez A, Ferrari MB, et al. (2017) Revision acromioclavicular-coracoclavicular reconstruction: Use of precontoured button and 2 allografts. Arthroscopy Techniques 6(6): e2283-2288.
- Takase K, Yamamoto K (2016) Arthroscopic procedures and therapeutic results of anatomical reconstruction of the coracoclavicular ligaments for acromioclavicular joint dislocation. Orthopaedics and Traumatology: Surgery and Research 102(5): 583-587.
- Tauber M, Valler D, Lichtenberg S, Magosch P, Moroder P, et al. (2016) Arthroscopic stabilization of chronic acromioclavicular joint dislocations: Triple-versus single-bundle reconstruction. American Journal of Sports Medicine 44(2): 482-489.
- Triantafyllopoulos IK, Lampropoulou-Adamidou K, Schizas NP, Karadimas EV (2017) Surgical treatment of acute type V acromioclavicular joint dislocations in professional athletes: An anatomic ligament reconstruction with synthetic implant augmentation. Journal of Shoulder and Elbow Surgery 26(12): e369-375.
- Xue C, Song LJ, Zhang H, Tang GL, Li X, et al. (2018) Truly anatomic coracoclavicular ligament reconstruction with 2 endobutton devices for acute Rockwood type V acromioclavicular joint dislocations. Journal of Shoulder and Elbow Surgery 27(6): e196-e202.
- Li Q, Hsueh PL, Chen YF (2014) Coracoclavicular ligament reconstruction: A systematic review and a biomechanical study of a triple endobutton technique. Medicine (Baltimore) 93(28): e193.
- Mazzocca AD, Santangelo SA, Johnson ST, Rios CG, Dumonski ML, et al. ( 2006) A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. American Journal of Sports Medicine 34(2): 236-246.
- Thomas K, Litsky A, Jones G, Bishop JY (2011) Biomechanical comparison of coracoclavicular reconstructive techniques. American Journal of Sports Medicine 39(4): 804-810.
- Xará-Leite F, Andrade R, Moreira PS, Coutinho L, Ayeni OR, et al. (2019) Anatomic and non-anatomic reconstruction improves post-operative outcomes in chronic acromio-clavicular instability: A systematic review. Knee Surgery Sports Traumatology Arthroscopy 27(12): 3779-3796.
- Clavert P, Meyer A, Boyer P, Gastaud O, Barth J, et al. (2015) Complication rates and types of failure after arthroscopic acute acromioclavicular dislocation fixation: Prospective multicenter study of 116 cases. Orthop Traumatol Surg Res 101(8 Suppl): S313-S316.
- Cook JB, Shaha JS, Rowles DJ, Bottoni CR, Shaha SH, et al. (2013) Clavicular bone tunnel malposition leads to early failures in coracoclavicular ligament reconstructions. American Journal of Sports Medicine 41(1): 142-148.
- Tsou PM (1989) Percutaneous cannulated screw coracoclavicular fixation for acute acromioclavicular dislocations. Clinical Orthopaedics And Related Research (243): 112-121.
- Rush LN, Lake N, Stiefel EC, Hobgood ER, Ramsey JR, et al. (2016) Comparison of short-term complications between 2 methods of coracoclavicular ligament reconstruction: A multicenter study. Orthopaedic Journal of Sports Medicine 4(7): 1-8.
- Cook JB, Shaha JS, Rowles DJ, Bottoni CR, Shaha SH, et al. (2012) Early failures with single clavicular transosseous coracoclavicular ligament reconstruction. Journal of Shoulder and Elbow Surgery 21(12): 1746-1752.
- Shin SJ, Kim NK (2015) Complications after arthroscopic coracoclavicular reconstruction using a single adjustable-loop-length suspensory fixation device in acute acromioclavicular joint dislocation. Arthroscopy 31(5): 816-824.
- Cook JB, Tokish JM (2014) Surgical management of acromioclavicular dislocations. Clinics in Sports Medicine 33(4): 721-737.
- Glanzmann MC, Buchmann S, Audigé L, Kolling C, Flury M (2013) Clinical and radiographical results after double flip button stabilization of acute grade III and IV acromioclavicular joint separations. Archives of Orthopaedic and Trauma Surgery 133(12): 1699-1707.
- Jensen G, Katthagen JC, Alvarado L, Lill H, Voigt C (2013) Arthroscopically assisted stabilization of chronic AC-joint instabilities in GraftRopeTM technique with an additive horizontal tendon augmentation. Archives of Orthopaedic and Trauma Surgery 133(6): 841-851.
- Eisenstein ED, Lanzi JT, Waterman BR, Bader JM, Pallis MP (2016) Medialized clavicular bone tunnel position predicts failure after anatomic coracoclavicular ligament reconstruction in young, active male patients. American Journal of Sports Medicine 44(10): 2682-2689.
- Jordan RW, Malik S, Bentick K, Saithna A (2019) Acromioclavicular joint augmentation at the time of coracoclavicular ligament reconstruction fails to improve functional outcomes despite significantly improved horizontal stability. Knee Surgery Sports Traumatology Arthroscopy 27(12): 3747-3763.
- Cohen G, Boyer P, Pujol N, Ferjani BH, Massin P, et al. (2011) Endoscopically assisted reconstruction of acute acromioclavicular joint dislocation using a synthetic ligament: Outcomes at 12 months. Orthopaedics and Traumatology Surgery and Research 97(2): 145-151.
- Shin SJ, Yun YH, Yoo JD (2009) Coracoclavicular ligament reconstruction for acromioclavicular dislocation using 2 suture anchors and coracoacromial ligament transfer. American Journal of Sports Medicine 37(2): 346-351.
- Mazzocca AD, Arciero RA, Bicos J (2007) Evaluation and treatment of acromioclavicular joint injuries. American Journal of Sports Medicine 35(2): 316-329.
- Scheibel M, Dröschel S, Gerhardt C, Kraus N (2011) Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. American Journal of Sports Medicine 39(7): 1507-1516.
- Hann C, Kraus N, Minkus M, Maziak N, Scheibel M (2018) Combined arthroscopically assisted coraco- and acromioclavicular stabilization of acute high-grade acromioclavicular joint separations. Knee Surgery Sports Traumatology Arthroscopy 26(1): 212-220.
- Maziak N, Audige L, Hann C, Minkus M, Scheibel M (2019) Factors predicting the outcome after arthroscopically assisted stabilization of acute high-grade acromioclavicular joint dislocations. American Journal of Sports Medicine 47(11): 2670-2677.
- Minkus M, Hann C, Scheibel M, Kraus N (2017) Quantification of dynamic posterior translation in modified bilateral Alexander views and correlation with clinical and radiological parameters in patients with acute acromioclavicular joint instability. Archives of Orthopaedic and Trauma Surgery 137(6): 845-852.
- Blazar PE, Iannotti JP, Williams GR (1998) Anteroposterior instability of the distal clavicle after distal clavicle resection. Clinical Orthopaedics and Related Research (348): 114-120.
- Debski RE, Parsons IV IM, Woo SLY, Fu FH (2001) Effect of capsular injury on acromioclavicular joint mechanics. J Bone Joint Surg Am 83(9): 1344-1351.
- Sahara W, Sugamoto K, Murai M, Tanaka H, Yoshikawa H (2006) 3D kinematic analysis of the acromioclavicular joint during arm abduction using vertically open MRI. Journal of Orthopaedic Research 24(9): 1823-1831.
- Testut L, Jacob O (1921) Treatise on topographic anatomy with medico-surgical applications. In: Doin O, Doin G (Eds.), (4th edn), Paris, France, pp. 756-774.
- Xue C, Song LJ, Zhang M, Zheng TS, Fang JH, et al. (2013) Coracoclavicular ligament attachment regions of the Chinese population: A quantitative anatomic study. Anatomical Science International 88(4): 189-194.
- Harris RI, Vu DH, Sonnabend DH, Goldberg JA, Walsh WR (2001) Anatomic variance of the coracoclavicular ligaments. Journal of Shoulder and Elbow Surgery 10(6): 585-588.
- Takase K (2010) The coracoclavicular ligaments: An anatomic study. Surgical and Radiologic 32(7): 683-688.
- Hislop P, Sakata K, Ackland DC, Gotmaker R, Evans MC (2019) Acromioclavicular joint stabilization: A biomechanical study of bidirectional stability and strength. Orthopaedic Journal of Sports Medicine 7(4): 1-7.
- Coale RM, Hollister SJ, Dines JS, Allen AA, Bedi A (2013) Anatomic considerations of transclavicular-transcoracoid drilling for coracoclavicular ligament reconstruction. Journal of Shoulder and Elbow Surgery 22(1): 137-144.
- Banffy MB, Uquillas C, Neumann JA, ElAttrache NS (2018) Biomechanical evaluation of a single-versus double-tunnel coracoclavicular ligament reconstruction with acromioclavicular stabilization for acromioclavicular joint injuries. American Journal of Sports Medicine 46(5): 1070-1076.
- Dumont GD, Russell RD, Knight JR, Hotchkiss WR, Pierce WA, et al. (2013) Impact of tunnels and tenodesis screws on clavicle fracture: A biomechanical study of varying coracoclavicular ligament reconstruction techniques. Arthroscopy 29(10): 1604-1607.
- Milewski MD, Tompkins M, Giugale JM, Carson EW, Miller MD, et al. (2012) Complications related to anatomic reconstruction of the coracoclavicular ligaments. American Journal of Sports Medicine 40(7): 1628-1634.
- Martetschläger F, Horan MP, Warth RJ, Millett PJ (2013) Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. American Journal of Sports Medicine 41(12): 2896-2903.
- Wylie JD, Beckmann JT, Granger E, Tashjian RZ (2014) Functional outcomes assessment in shoulder surgery. World Journal of Orthopedics 5(5): 623-633.
- Angst F, Schwyzer HK, Aeschlimann A, Simmen BR, Goldhahn J (2011) Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) society standardized shoulder assessment form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI). Arthritis Care and Res (Hoboken) 63(Suppl 11): S174-S188.
- Dijkers M (2010) Comparing quantification of pain severity by verbal rating and numeric rating scales. J Spinal Cord Med 33(3): 232-242.
- Voutilainen A, Pitkäaho T, Kvist T, Vehviläinen-Julkunen K (2016) How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. Journal of Advanced Nursing 72(4): 946-957.
- Murena L, Vulcano E, Ratti C, Cecconello L, Rolla PR, et al. (2009) Arthroscopic treatment of acute acromioclavicular joint dislocation with double flip button. Knee Surgery, Sports Traumatology, Arthroscopy 17(12): 1511-1515.
© 2022 Philippe Vial. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






