- Submissions

Full Text
Orthopedic Research Online Journal
Neurogenic Heterotopic Ossification of the Hip: A Surgical Management
Chopra RK*, Simarjot Singh Sodhi, Surya Vijay Singh, Pritam Samanta, Gyanendra Puri, Deepanshu Mittal and Nitin Kumar
Senior Resident, Guru Gobind Singh University, India
*Corresponding author: Chopra RK, Senior Resident, Guru Gobind Singh University, India
Submission: July 14, 2022;Published: July 26, 2022

ISSN: 2576-8875 Volume9 Issue5
Abstract
Neurogenic Heterotopic Ossifications (NHO) is a condition in which unregulated spontaneous formation of bone tissue in between the muscles occurs especially around periarticular areas of large joints. Our aim of the study is to evaluate the clinical, functional and complication of the surgical management of Neurogenic Heterotopic Ossification of the hip joints.
Method and material: Medical records of 3 patients who had undergone surgical resection for NHO were reviewed in retrospect from 2018 to 2020. All 3 patients had suffered from road traffic accidents with traumatic brain injury. Preoperative x rays and CT scans were done to assess the location and size of ossification. Anterior approach was used to operate the NHO.
Results: The mean age of the patients was 36.67 years. The mean age of the patients in our study was 36.67 years (28-43 years). All 3 patients were males with history of RTA. All 3 had involvement of the right hip. The mean duration from accident to presentation in our institute was 9.33 months. All patients had preoperative ambulatory score of 4. The mean postoperative ambulatory score at end of follow up period was 2.33. The mean duration of surgery was 168.33 minutes. The mean intraoperative blood loss was 1066.67cc. The average drain volume was 450cc of blood. One patient developed paraesthesia and tingling sensation on an anterolateral aspect of thigh which resolved in 3 months with medication.
Background
Myositis ossificans is a benign condition of new bone formation in muscles. It is non- neoplastic [1]. Trauma is the most common cause of development of myositis ossificans. Non traumatic MO is a rare entity [2]. Trauma leads to formation of intermuscular hematoma which leads to the start of multiple events that lead to bone formation in muscles [3]. Neurogenic Heterotopic Ossifications (NHO) is a condition in which unregulated spontaneous formation of bone tissue in between the muscles occurs especially around periarticular areas of large joints. Neurogenic Heterotopic ossification occurs after traumatic brain injury or after traumatic spinal cord injury with or without association with localized trauma [4]. It occurs mostly in polytrauma patients who need some sort of critical or intensive care [5]. Other risk factors that are associated with heterotopic ossification is localised massage of the involved area and prolonged immobilization [4].
NHO’s mostly affect the area around hip [6]. NHO’s occuring after traumatic brain injury affect the anteromedial side of the hip whereas those occurring after spinal cord injury affect the anterior portion of Hip [7]. The other areas commonly involved are medial, lateral and posterior side of Hip. Posterior NHO’s frequently involve sciatic nerve. The ossification process is periarticular but never involves joints. The capsule can be thinned out but conserved. If the joint space is maintained, arthrotomy need not to be performed. Muscle planes are involved but tendons remained conserved.
Arteries are not invaded, however surrounded whereas veins are compressed [8]. In case of minor ossifications, conservative treatment is preferred which includes joint physiotherapy, use of NSAIDs, shockwave therapy and radiotherapy. However, when the area involved is large and it leads to limitation of daily activities or neurovascular compromise, surgical resection is planned [9]. To the best of my knowledge, very few case reports of NMO of the hip joint requiring surgical resection have been reported in India. Our aim of the study is to evaluate the clinical and radiological outcomes and also assess the challenges in surgical resection of NMO of the hip joint.
Study Population
Medical records of 3 patients who had undergone surgical resection for NMO were reviewed in retrospect from 2018 to 2020. All 3 patients had suffered from road traffic accidents with traumatic brain injury. Two patients had a history of dislocation of the hip which was reduced immediately. The mean age of the patients was 36.67 years. The patients presented to our institute with the chief complaints of hip pain, unable to walk and restriction of hip movements. The mean duration between accident and presentation to our hospital was 6 months. The mean follows up period was 9.33 months. The indication for surgery was severe periarticular heterotopic ossification limiting functional activity and range of motion of hip. All the patients faced difficulty in sitting, walking without support and getting up from sitting position. Surgical resection was planned when evidence of maturity of NHO was confirmed on radiological basis as well as when serum alkaline phosphatase values were normal for at least 6 months. Mean GMFCS (Gross Motor Function Classification System) Score was 4.
Preoperative Evaluation and Preparation
Preoperative general physical examination, higher mental function, local examination of involved hip, range of motion and neurovascular status was assessed. GMFCS score was noted. Preoperative x rays and CT scans were done to assess the location and size of ossification, borders, and changes in the hip joint, its relationship to the joint capsule. Angiography studies were performed to assess the relationship with vessels. Preoperative investigations including haemoglobin, serum electrolytes, random blood sugar, blood urea, serum creatinine, total bilirubin, ECG, urine routine and microscopic examination and chest x-ray was done as part of pre-anaesthetic evaluation.
Surgical Treatment and Postoperative Care
The procedure was performed with patient lying in supine position with a bolster under the ipsilateral hip. Patient was anaesthetized using appropriate anaesthesia. Prophylactic antibiotics (3rd generation cephalosporins) were given 15 minutes prior to surgery and repeated after every 4 hours. 1g of injection tranexamic acid was given preoperatively. The surgical site was draped exposing the iliac crest, ASIS (anterior superior iliac spine), Pubic tubercle till mid thigh. All bony prominences, neurovascular structures and surgical sites were marked. 8cm incision along the anterior half of the iliac crest to ASIS and from there it curved downwards vertically for another 8cm heading towards the lateral side of patella. Skin, subcutaneous tissue were cut and retracted. Soft tissue dissection was done with utmost care and muscle planes were identified. Cauterization and ligation of small bleeding vessels were performed when needed. Superficial plane was made between the sartorius and tensor fascia lata. Lateral cutaneous nerve of thigh was identified and retracted medially along with sartorius. Tensor fascia lata was detached from iliac crest and sartorius from ASIS. Deep plane was made between rectus femoris and gluteus medius. Both heads of Rectus femoris were detached from their origin and gluteus medius retracted laterally to expose the capsule of the hip joint. As the joint was not involved, Capsulotomy was not done. The exposure was done till the lesser trochanter. The mass seen was osseous in nature and extended superiorly from the lateral border of iliopsoas along the supra acetabular area over the capsule of hip joint till 5cm below the lesser trochanter. Moreover an osseous bridge was being formed from supra acetabular area to lesser trochanter which was limiting the motion of the hip joint. The mass was removed surgically from the intermuscular planes as well as around the hip joint piece by piece using osteotome and hammer taking into account the adjoining neurovascular structures. Osseous bleeding was controlled by application of bone wax.
After resection of the mass, hip motion was checked intraoperatively to assess range of motion and impingement, if any. Drain was put and closure was done in layers. 1g of tranexamic acid injection given at the time of closure and 6hrs after surgery. Standard antibiotics, analgesics were given in the postoperative period. Tablet indomethacin 150mg OD (sustained release tablets) were given for 2 months. Physiotherapy was started and followed. Drain was removed after 3 days. Patients were mobilized with walker from day 2 and without walker after day 7. Sutures were removed after 21 days and post operative visits were scheduled at 2nd week, 4th week, 3rd month and 6th month and GMFCS and ROM (range of motion) was noted with each visit.
Results
Medical records of 3 patients who had undergone surgical resection of NMO were reviewed and following data was collected: Age, sex, date and type of accident, site of injury, duration from injury to presentation to our hospital, preoperative and postoperative ambulatory function, preoperative and postoperative ROM, duration of surgery, intraoperative blood loss, post operative drain volume, units of blood transfused and complications.
We are presenting Categorical variables in number and percentage (%) and continuous variables as mean ± SD and median. Normality of data was tested by Kolmogorov-Smirnov test. If the normality was rejected, then a non parametric test was used. Quantitative variables were compared using Wilcoxon signed rank Test (as the data sets were not normally distributed) between pre and post. A p-value of <0.05 was considered statistically significant. The data was entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
The mean age of the patients in our study was 36.67 years (28- 43 years). All 3 patients were males with history of RTA. All 3 had involvement of the right hip. The mean duration from accident to presentation in our institute was 9.33 months. All patients had preoperative ambulatory score of 4. The mean post op ambulatory score at end of follow up period was 2.33. The mean ROM is described in the Table 1 below.
Table 1:

The mean duration of surgery was 168.33 minutes. The mean intraoperative blood loss was 1066.67cc. The average drain volume was 450cc of blood. An average of 3 units of whole blood was transfused in intraoperative and immediate post-op period. One patient developed paraesthesia and tingling sensation on anterolateral aspect of thigh for which patient was started on oral methyl cobalamin for 3 months after which symptoms were resolved. One patient had no improvement in adduction and the same patient had serous discharge from the suture site which resolved spontaneously after 1 week. However, no patients developed deep infection, severe hematoma and deep vein thrombosis. No recurrence was noted in the said period.
Medical records of three patients who had undergone surgical resection of NMO were reviewed and following data was collected: Age, sex, date and sort of accident, site of injury, duration from injury to presentation to our hospital, preoperative and postoperative ambulatory function, preoperative and postoperative ROM, duration of surgery, intraoperative blood loss, post operative drain volume, units of blood transfused and complications.
We are presenting Categorical variables in number and percentage (%) and continuous variables as mean ± SD and median. Normality of knowledge was tested by Kolmogorov-Smirnov test. If the normality was rejected, then a non parametric test was used. Quantitative variables were compared using Wilcoxon signed rank Test (as the info sets weren’t normally distributed) between pre and post. A p-value of <0.05 was considered statistically significant. the info was entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
The mean age of the patients in our study was 36.67 years (28- 43 years). All 3 patients were males with history of RTA. All 3 had involvement of the proper hip. The mean duration from accident to presentation in our institute was 9.33 months. All patients had preoperative ambulatory score of 4. The mean post op ambulatory score at end of follow up period was 2.33. The mean ROM is described within the table below.
Discussion
Neurogenic Heterotopic Ossification is usually developed after Traumatic Brain Injury which stimulates the body to produce and release various cytokines that generate osteogenic effects. Brain injury also damages the blood brain barrier to release the several osteogenic factors (BMP, Thrombin, TGF-b1, VEGF), neuropeptides and hormones like CGRP (calcitonin gene related peptides), Substance- P, Leptin and Melatonin into the blood stream. Trauma is the most common cause of development of myositis ossificans. Non traumatic Heterotopic Ossification is a rare entity2. In our study all patients had a history of having RTA associated with traumatic brain injury.
NHO develops in the connective tissue between the muscle planes, usually not involved in muscle [10]. Quadriceps femoris and iliopsoas were found to be most affected [11]. In our study it was found that iliopsoas was most commonly affected. There is no involvement of the femoral neurovascular bundle in our patients intraoperatively.
The use of NSAIDS (nonsteroidal anti-inflammatory drugs) has shown to decrease the incidence of recurrence of NHO and has been used in the prophyllaxis [12]. Another option is low-dose radiation therapy but in our study, we used NSAIDS and no recurrence was noted [13].
In study of Stover et al. [14] observed narrowing of the joint surface with severe osteoarthritic change and atrophy of muscles suggested that prolonged immobilization stimulates fibro-fatty proliferation and fibrous ankylosis [14]. In our study there were no severe osteoarthritic changes seen but muscles atrophy was noted in all 3 pateints.
In a study by Yoon BH et al. [9] Average ROM of the hip improved from 24.3° (flexion and extension) to 98.5° (flexion and extension) after surgery, and this was maintained even after the last follow-up. There were no common complications like deep infection, severe hematoma, deep vein thrombosis occurred in any patient [9]. In our study, mean ROM improved flexion (46.67 to 105), extension (0 to -10). There is no involvement of the femoral neurovascular bundle in our patients intraoperatively (Figures 1-12).
Figure 1: Preoperative photograph of patient showing attitude of the limb.

Figure 2:Preoperative photograph of patient showing attitude of the limb.
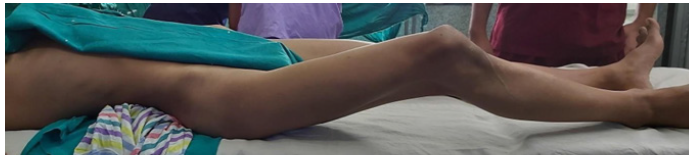
Figure 3: Preoperative radiograph of patient showing ossification over anteromedial surface of hip.
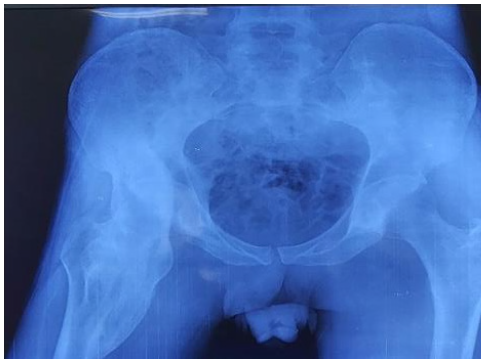
Figure 4:Preoperative coronal CT image of the patient.
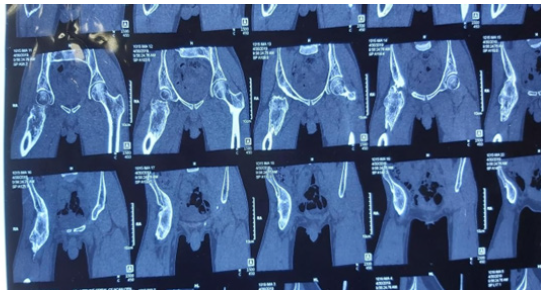
Figure 5:Preoperative coronal CT image of the patient.
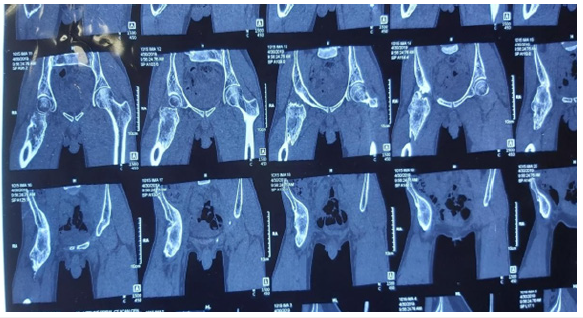
Figure 6: Axial CT images of hip.
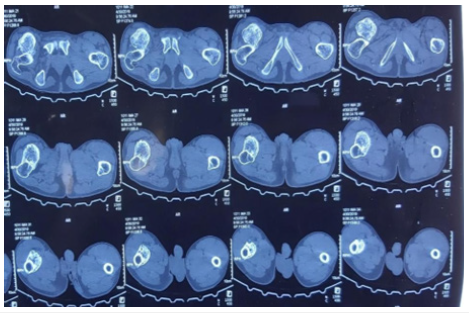
Figure 7: Incision and exposure via smith peterson approach.
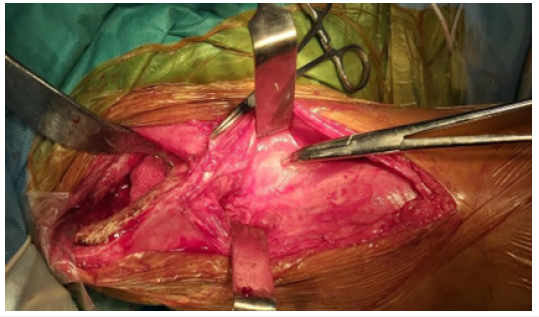
Figure 8: Deep Exposure showing bony tissue around hip.
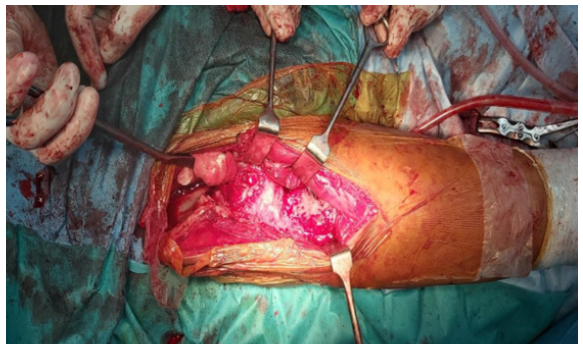
Figure 9: Cut out bony mass.

Figure 10: Post operative Radiograph.

Figure 11: At 6 months follow up, patient can in squatting position

Figure 12: At 6 months follow up, patient can in cross legged position.

Limitations
The limitations of our study were a retrospective study with a small number of patients. Ambulatory scores and range of motion was noted and other parameters were not evaluated. The functional outcomes of early and delayed surgery were not noted.
Conclusion
Surgical resection is an appropriate treatment in the management of heterotopic ossification if performed with appropriate indications. There was significant improvement in Range of motion of hip and ambulatory scores improved significantly. NSAIDS are an important pharmacological prophylactic agent in preventing recurrence.
References
- Folpe L, Inwards CY (2010) Osteocartilaginous tumors. In Bone and Soft Tissue Pathology, O’Connell JX (Ed.), A Volume in the Foundations in Diagnostic Pathology Series, Saunders-Elsevier, Philadelphia, Pa, USA, pp. 239-254.
- Yazici M, Etensel B, Gursoy MH, Aydo A, Erkus M (2022) Nontraumatic myositis ossificans with an unusual location: case report. Journal of Pediatric Surgery 37(11): 1621-1622.
- Goyal K, Pettis CR, Bancroft AE, Wasyliw CW, Scherer KF (2015) Myositis ossificans in the thigh of a lacrosse Orthopedics 38: 515-518.
- Sakellariou VI, Grigoriou E, Mavrogenis AF, Soucacos PN, Papagelopoulos PJ (2012) Heterotopic ossification following traumatic brain injury and spinal cord injury: insight into the etiology and pathophysiology. J Musculoskelet Neuronal Interact 12(4): 230-240.
- Garland DE, Orwin JF (1989) Resection of heterotopic ossification in patients with spinal cord injuries. Clin Orthop Relat Res (242): 169-176.
- Garland DE (1988) Clinical observations on fractures and heterotopic ossification in the spinal cord and traumatic brain injured populations. Clin Orthop Relat Res (233): 86-101.
- Ebinger T, Roesch M, Kiefer H, Kinzl L, Schulte M (2000) Influence of etiology in heterotopic bone formation of the hip. J Trauma 48(6): 1058-1062.
- de l'Escalopier N, Salga M, Gatin L, Genêt F, Denormandie P (2019) Resection of heterotopic ossification around the hip after trauma. EFORT Open Rev 4(6): 263-268.
- Yoon BH, Park IK, Sung YB (2018) Ankylosing neurogenic myositis ossificans of the hip: A case series and review of literature. Hip Pelvis 30(2): 86-
- Vanden Bossche L, Vanderstraeten G (2005) Heterotopic ossification: a J Rehabil Med 37(3): 129-136.
- Wick L, Berger M, Knecht H, Glücker T, Ledermann HP (2005) Magnetic resonance signal alterations in the acute onset of heterotopic ossification in patients with spinal cord injury. Eur Radiol 15(9): 1867-1875.
- Banovac K, Williams JM, Patrick LD, Levi A (2004) Prevention of heterotopic ossification after spinal cord injury withCOX-2 selective inhibitor (rofecoxib). Spinal Cord 42: 707-710.
- Huang H, Cheng WX, Hu YP, Chen JH, Zheng ZT, et al. (2017) Relationship between heterotopic ossification and traumatic brain injury: Why severe traumatic brain injury increases the risk of heterotopic ossification. J Orthop Translat 12: 16-25.
- Stover SL, Niemann KM, Tulloss JR (1991) Experience with surgical resection of heterotopic bone in spinal cord injury patients. Clin Orthop Relat Res (263): 71-77.
© 2022 Chopra RK. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






