- Submissions

Full Text
Orthopedic Research Online Journal
Isolated Fracture of the Lesser Tuberosity, A Case Report and Literature Review
Alex N Karanja*, Andrew P McBride and Michael J Thomas
Department of Orthopaedic Surgery, Hand and Upper Limb Unit, Gold Coast University Hospital, Australia
*Corresponding author: Alex Ngatia Karanja, Department of Orthopaedic Surgery, Hand and Upper Limb Unit, Gold Coast University Hospital, 1 Hospital Blvd, Southport, 4215, Queensland, Australia.
Submission: July 08, 2022;Published: July 20, 2022

ISSN: 2576-8875 Volume9 Issue5
Abstract
Background: Isolated fracture of the lesser tuberosity of the humerus is a rare injury that is commonly missed at initial presentation with a third of known cases having a delayed diagnosis. The purpose of this article is to report a case of an isolated lesser tuberosity fracture that was initially misdiagnosed in the emergency department of a metropolitan hospital and then surgically fixed with a novel technique. We also present a review of the literature and propose a new diagnostic algorithm for the initial assessment and management of this injury.
Case presentation: A 35-year-old male, left-hand-dominant carpentry student, presented to the emergency department of a metropolitan hospital with left shoulder pain after a fall off a skateboard. He was misdiagnosed with a soft tissue injury and discharged with a sling and simple analgesia after an anteroposterior (AP) radiograph failed to demonstrate the fracture. He represented two days later when orthopaedic examination revealed a positive Napoleon sign, further imaging including a lateral radiograph and subsequent CT and MRI imaging demonstrated a lesser tuberosity avulsion fracture. His fracture was fixed with four bioabsorbable suture anchors with a double row suture bridge technique. At 6 months post-operative he achieved a constant shoulder score of 70, a range of motion including 145 degrees abduction, 150 degrees flexion and internal rotation to T12. He had no limitations to his daily activities.
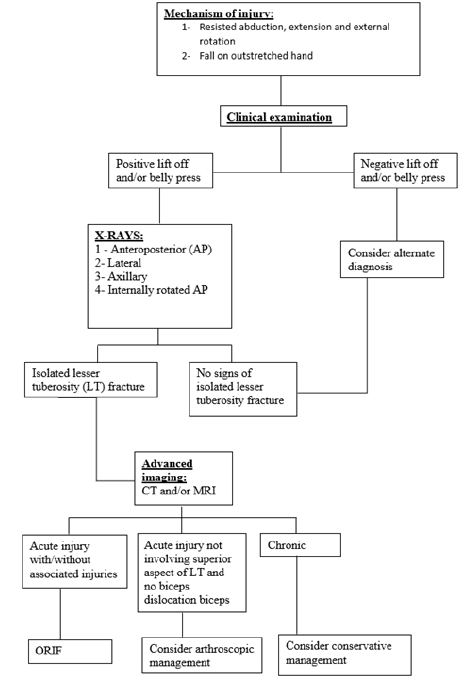
Conclusion: Our case, in addition to a literature review, reveals that a high clinical index of suspicion in patients presenting with shoulder pain after specific mechanisms of injury and a positive belly press sign on examination combined with special x-ray views and axial imaging can reduce the incidence of missed isolated lesser tuberosity fractures. The literature suggests that acute cases in younger patients should be managed operatively while a trial of econservative treatment in chronic cases is appropriate. These findings are summarised in our newly proposed diagnostic and management algorithm.
Keywords:Shoulder surgery; Isolated fracture; Lesser tuberosity
Abbreviations: AP: Anteroposterior; LT: Lesser Tuberosity; MRI: Magnetic Resonance Imaging; CT: Computed Tomography; T12: Twelfth Thoracic Vertebra
Background
Isolated fracture of the lesser tuberosity of the humerus is a rare injury occurring in only 0.46 persons per 100,000 [1]. Two-thirds occur in adults and one-third in paediatric age groups [2]. The primary mechanism of injury is forced abduction, extension and external rotation to the shoulder. With the arm in this position, there is a strong eccentric contraction of the subscapularis muscle that causes avulsion of the lesser tuberosity [3]. The diagnosis is commonly missed at initial presentation with a third of known cases having a delayed diagnosis [4]. The incidence of cases reported has increased in the past three decades [5]. This is likely due to the increased awareness of the injury along with improved use of clinical and radiographic examination by clinicians. The purpose of this article is to report a case of isolated avulsion of the lesser tuberosity that was initially misdiagnosed in the emergency department of a metropolitan hospital and surgically fixed with a novel technique. We also present a review of the literature and propose a new diagnostic algorithm for the initial assessment and management of this injury.
Case Presentation
A 35-year-old left hand dominant carpentry student presented to the emergency department of a metropolitan hospital complaining of left shoulder pain following a fall off a skateboard. The patient was reviewed by a resident medical officer who examined the patient, ordered an antero-posterior (AP) (Figure 1) and lateral radiograph of the shoulder. The patient was misdiagnosed with a soft tissue injury of the shoulder and discharged with a sling, analgesia and advised to see his general practitioner for follow up.
Figure 1: Left anteroposterior and lateral shoulder radiograph.

The patient re-presented to the same institution two days later complaining of severe shoulder pain. He described falling off his skateboard landing on his left arm in a position of abduction, extension and external rotation. On examination there was extensive bruising over the anterior and medial aspect of his left arm and on the palmar surface of his left hand. There was tenderness on palpation over the anterior shoulder. The patient was unable to abduct, flex or extend the left arm. Assessment of muscle power showed grade 2 abduction, grade 3 external rotation and grade 2 internal rotation. The patient had a positive belly press test (Napoleon sign). Sensation testing of the upper limb was unremarkable. A repeat lateral radiograph of the shoulder showed a large displaced bone fragment adjacent to the inferomedial aspect of the glenoid (Figure 2).
Figure 2: Left lateral shoulder radiograph.

A CT (computed tomography) scan of the shoulder demonstrated a comminuted fracture through the lesser tuberosity with >1cm of displacement (Figure 3 & 4). A subsequent MRI (magnetic resonance imaging) Scan of the shoulder showed a comminuted fracture of the lesser tuberosity of the humerus with complete avulsion of the subscapularis muscle (Figure 5). Multiple small interstitial tears of the supraspinatus tendon and a partial thickness tear of teres minor were also reported.
Figure 3: Left shoulder CT scan coronal view.
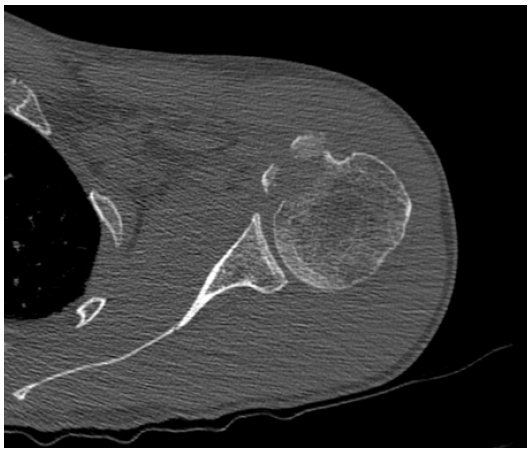
Figure 4: Left shoulder CT scan reconstruction.

Figure 5:Left shoulder coronal MRI scan.

The risks and benefits of operative versus conservative management were discussed. Given the degree of displacement of the fracture fragment, manual occupation and young age of the patient, a decision was made to proceed to operative management with the patients informed consent. His operation was performed eleven days from his injury.
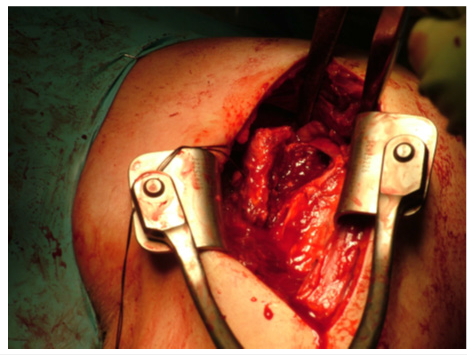
A left shoulder arthroscopy was performed which identified no significant supraspinatus, infraspinatus or labral tear. The biceps anchor was intact. An open deltopectoral approach was then utilised. The lesser tuberosity fracture was identified with the avulsed anterior compartment (Figure 6). The bicipital groove was intact. The rotator interval was incised. A separate isolated bony fragment was removed and prepared as bone graft.
Figure 6:Deltopectoral approach showing fracture fragment.
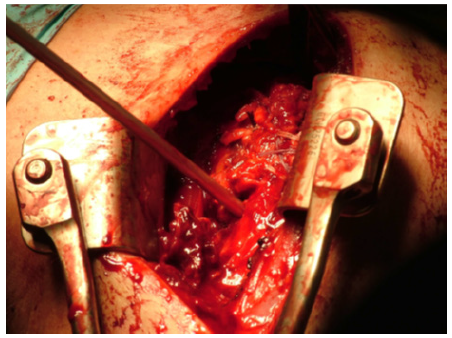
The lesser tuberosity was reattached in two rows with four bioabsorbable suture anchors, (swive lock from Arthrex®), using a suture bridge technique (Figure 7). Good reduction was achieved with adequate range of motion of passive external rotation to 30 degrees, without displacing the repair. The rotator interval was repaired using a side-to-side stitch and the shoulder was closed in layers with vicryl and nylon.
Figure 7:Deltopectoral approach showing fracture fragment.
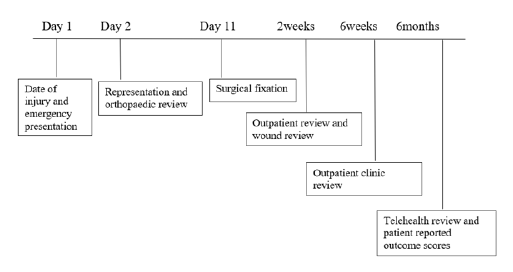
The patient was immobilised in a sling for six weeks postoperatively and followed up in our specialist outpatient clinic. Passive range of motion exercises were commenced from postoperative day two with external rotation movement restricted to neutral for three weeks. Active assisted range of motion exercises and scapular strengthening was commenced from three weeks. His wound was completely healed, and sutures removed at two weeks after the operation. At six weeks, the patient had regained 60 degrees of active flexion and abduction. The patient returned to France and was followed up by email at six months post-operative. Through a questionnaire and photographs we were able to approximate a constant score of 70. The patient was able to achieve 145 abduction, 150 degrees flexion and internal rotation to T12 (Figure 8.1 & 8.2)(Figure 9).
Figure 8:Range of movement at six months post operative.

Figure 9:Case presentation timeline.
Discussion and Conclusion
The first case of fracture through the lesser tuberosity of the humerus was described by Hartigan in 1895 in a boy who fell from a roof [6]. In 1997, a review of the literature conducted by Ogawa presented the largest known case series of 10 cases and identified a further 60 reported cases [4]. We have been able to identify a further 28 cases since Ogawa’s report in 1997 taking the total number of known case reports to 98 [2,7-29].
Isolated fracture of the lesser tuberosity of the humerus has previously been reported as a rare event [1]. A review of humeral tuberosity fractures by Gruson estimated that isolated lesser tuberosity fractures account for 2% of all proximal humeral fractures. In contrast, the incidence of isolated greater tuberosity fractures was estimated to be 20% of all proximal humeral fractures [9]. The true incidence and misdiagnosis rates of isolated lesser tuberosity fractures may remain hidden as many injuries managed non operatively have satisfactory outcomes [5]. The high proportion of chronic cases reported in the literature suggest that they are often overlooked at the time of injury [4]. Furthermore, a number of authors experienced in the diagnosis and management of this injury have reported series of cases over relatively short time periods [4,17,30].
Fractures of the lesser tuberosity occur mostly in men under the age of 50. Of the 98 cases identified 80 have occurred in an individual under the age of 50 with 28 of these occurring in adolescents under the age of 20. 66 of the 98 cases occurred in men, 21 in women and in the remainder the gender is not known to this author.
Two main mechanisms have been described. A mechanism that involves resisted abduction, external rotation and extension of the shoulder has been commonly reported [4,14,15,19,22,28,29,31,32]. It is postulated that the subscapularis eccentrically contracts protectively causing a traction force through the lesser tuberosity resulting in avulsion [3,4]. A second mechanism of a fall on an outstretched hand has been reported [4,11,12,15,24,30,32,33]. It is thought that during such a fall, the forces resulting from an axial load on the humerus cause superior migration of the humeral head and increased tension in the subscapularis muscle and the superior glenohumeral ligament [4,34]. Other mechanisms described include electroconvulsive therapy [6], electrocution [25] and epileptic seizures [18,27]. The lesser tuberosity is protected from direct injury due to its small size and location medial to the head of the humerus [9]. In many cases the exact mechanism remains unknown [4,17,18,20,26,35-37].
In acute and chronic cases, patients report anterior shoulder pain and a reduced range of motion about the shoulder [2,4,11,12,14,15,17-22,24,25,27,31,32,34,36-40]. Other examination findings include severe pain with passive external rotation [12,14,36], weakness of internal rotation [2,11,19,20,21- 23,25-29,31,32,40] and positive apprehension and relocation tests [2,4,40]. These findings are not specific to the diagnosis of lesser tuberosity avulsion. To specifically test the function of the subscapularis complex, the lift off test or belly press test must be performed [14]. The lift off test involves the patient placing the affected hand behind the back and pushing outwards into the examiners hand [14]. A positive test occurs when the patient is unable to push into the examiners hand [18]. The belly press test should be performed when the lift off cannot be due to pain or limited range of motion. The patient places the hand of the affected side on the belly and attempts to push down as the elbow is moved forwards. The test is positive if the patient cannot press against the belly while trying to internally rotate the shoulder. Several authors report a positive lift off or belly press test in lesser tuberosity avulsion [8,11,14,15,21,26,31,36]. The lift off and belly press tests may be positive due to subscapularis muscle injury. Proving the existence of a bone fragment radiologically is therefore necessary for the diagnosis of lesser tuberosity avulsion [4].
Many cases of lesser tuberosity avulsion are missed on initial plain radiograph [12,14,18,20,22,28,29,30,32,35]. Ross, Ogawa and Rajani found that an anteroposterior radiograph in internal rotation clearly demonstrated fracture fragments in cases where anteroposterior radiographs in neutral did not [4,28,32]. The axillary view is the most sensitive radiograph view clearly identifying the fracture fragment when performed [2,4,11,12,15,1 8,19,21,26,29,30,32,33,37].
CT scan of the shoulder is helpful in characterising the displacement of the fracture as well as identifying the extent of involvement of the lesser tuberosity [4,11,18,19,20,21,22,24,25 ,28,33,34]. Fractures involving the superior aspect of the lesser tuberosity are associated with medial dislocation of the biceps [14,30,31]. MRI scans help characterise the fracture and identify associated injuries [8,15,17,24,26-29,36]. In cases where MRI is not available ultrasound scan has been used to identify associated biceps dislocation and injury to the rotator cuff [40].
Almost all authors that performed surgery utilised an open procedure for repair via a deltopectoral approach. Two reported cases have been managed arthroscopically with a good outcome [15,26].
Satisfactory outcomes have been achieved with both conservative and surgical management. Ogawa compared the outcomes of three acute cases treated surgically with three patients who refused surgical treatment and were treated nonoperatively. The long-term outcomes obtained by open reduction via a deltopectoral approach were superior to those obtained by conservative treatment [4]. Of the 28 cases we have identified since Ogawa’s 10, 25 were managed operatively and 3 non-operatively. All cases had a good outcome with pain free range of motion and return to premorbid function at long term follow up.
Similar outcomes are achieved in chronic case presentations with conservative and surgical management with the outcomes generally being good [4,14,20,26,29,31,32,35,37,38,41].
However, most authors suggest that in acute cases where displacement of the lesser tuberosity is greater than five millimetres surgery should be considered particularly in young patients. Two systematic reviews by Vavken and Spek have confirmed better outcomes of surgical treatment compared to nonoperative treatment in paediatric patients with displaced fractures. For this reason, clinicians should strongly consider surgery for paediatric patients with fractures displaced more than 5mm [5,42].
Robinson and Cottias advocated for surgical treatment over nonoperative treatment in patients with displaced fractures and demonstrated better outcomes [1,43]. Moreover, Cottias pointed out that almost one-third of the initial nonoperatively treated patients had to undergo surgery due to secondary fragment displacement [43].
Spek’s systematic review found that there was no significant difference between the outcomes of acute and delayed treatment (>6 weeks) in paediatric and adult patients [5]. Many authors however, advocate a trial of conservative management in chronic case presentations [7,11,18,39,41,44,45].
We conclude that isolated lesser tuberosity fractures are perhaps more common than once thought. They occur predominantly in young males due to a mechanism that involves forceful contraction of the subscapularis. Symptoms and signs are variable at presentation. All patients should undergo a lift off or belly press test to assess the integrity of the subscapularis. Imaging is necessary to obtain the diagnosis and axillary radiograph is the most sensitive view for detecting the fracture. Where MRI is available, it is helpful in characterising the displacement of the fracture and associated injuries [46]. Where it is not available, CT scan and Ultrasound scan should be performed. In acute cases where there is fracture displacement surgical management is indicated and proven to achieve better patient outcomes. In chronic cases conservative management is a reasonable option however a low threshold for surgical management should be considered for young healthy patients. Arthroscopic surgical management has been found to be successful in isolated lesser tuberosity fractures where there is no biceps displacement or other associated injury and remains an option for the future. Figure 10 summarizes our management algorithm based on the above findings.
Figure 10:Diagnostic algorithm for lesser tuberosity avulsion fractures.
References
- Robinson CM, Teoh KH, Baker A, Bell L (2009) Fractures of the lesser tuberosity of the humerus. J Bone Joint Surg Am 91(3): 512-520.
- Levine B, Pereira D, Rosen J (2005) Avulsion fractures of the lesser tuberosity of the humerus in adolescents: review of the literature and case report. J Orthop Trauma 19(5): 349-352.
- Van Laarhoven HA, te Slaa RL, van Laarhoven EW (1995) Isolated avulsion fracture of the lesser tuberosity of the humerus. J Trauma 39(5): 997-999.
- Ogawa K, Takahashi M (1997) Long-term outcome of isolated lesser tuberosity fractures of the humerus. Journal of Trauma - Injury, Infection and Critical Care 42(5): 955-999.
- Spek R, Schoolmeesters B, den Haan C, Jaarsma RL, Doornberg JN, et al. (2021) What are the patient-reported outcomes, functional limitations, and complications after lesser tuberosity fractures? a systematic review of 172 patients. JSES Int 5(4): 754-764.
- Hartigan JW (1895) Separation of the lesser tuberosity of the head of the humerus. NY Med J 61: 276.
- Biedert RM, Maitre T (200) Conservative treatment of isolated fractures of the lesser tuberosity of the humerus. Swiss journal for Sports Medicine and Sports Traumatology 48(4): 158-160.
- Dhawan A, Kirk K, Dowd T, Doukas W (2008) Isolated avulsion fracture of the lesser tuberosity of the humerus in an adult: case report and literature review. Am J Orthop (Belle Mead NJ) 37(12): 627-630.
- Gruson KI, Ruchelsman DE, Tejwani NC (2008) Isolated tuberosity fractures of the proximal humerus: Current concepts. Injury 39(3): 284-298.
- Kanso I, Bricout JM (1998) Isolated avulsion fracture of the lesser tuberosity of the humerus: A case report. Journal of Orthopedic and Restorative Surgery of the Motor Apparatus 84(6): 554-557.
- Kumar V, Candal-Couto J, Rangan A (2006) Isolated avulsion fracture of the lesser tuberosity of the humerus associated with delayed axillary nerve neuropraxia. Injury Extra 37(1): 31-33.
- Maris SG, Papanicolaou A (2006) Isolated avulsion fracture of the lesser humeral tuberosity: A case report. Journal of the Hellenic Association of Orthopaedic and Traumatology 57(2).
- Ollat D, Mathieu L, Bouchard A, Marchaland JP, Versier G (2008) Isolated fracture-avulsion of the minor tubercle of the humerus: About a case and review of the literature. Journal of Sports Traumatology 25(2): 102-106.
- Provance AJ, Polousky JD (2010) Isolated avulsion fracture of the subscapularis tendon with medial dislocation and tear of biceps tendon in a skeletally immature athlete: a case report. Curr Opin Pediatr 22(3): 366-368.
- Scheibel M, Martinek V, Imhoff AB (2005) Arthroscopic reconstruction of an isolated avulsion fracture of the lesser tuberosity. Arthroscopy 21(4): 487-494.
- Shah NN, Agarwal A, Turner R, Hatrick C (2006) Avulsion of the lesser tuberosity with a Salter-Harris type II injury of the proximal humerus: A case report. Journal of Shoulder and Elbow Surgery 15(5): e16-e8.
- Steinbach L, Nardo L, Ma B (2011) Lesser tuberosity avulsions in adolescents. Pediatric Radiology. Conference: International Congress of Pediatric Radiology, IPR 2011 London United Kingdom. Conference Start: 20110528 Conference E.
- Tosun B, Kesemenli CC (2011) Isolated avulsion fracture of lesser tuberosity of the humerus: Review of the literature and report of two cases. Int J Shoulder Surg 5(2): 50-53.
- Lik-Hang Hung, Kwong-Yin Chung, Ning Tang, Kwok-Sui Leung (2012) Isolated avulsion fracture of the lesser tuberosity of the humerus: Case report and literature review. Journal of Orthopaedics, Trauma and Rehabilitation 16(2): 78-81.
- Bao M, Barquet A (2021) Nonunion of lesser tuberosity fracture in A 16-year-old teenager. Front Med Case Rep 2(4): 1-6.
- Ohzono H, Gotoh M, Mitsui Y, Kanesaki K, Okawa T, et al. (2011) Isolated fracture of the lesser tuberosity of the humerus: a case report. Kurume Med J 58(4): 131-133.
- Oburu E, John J (2014) Isolated displaced fracture of the lesser tuberosity. The Annals of African Surgery 11(2): 52-53.
- Gen-Bin Wu, Shu-Qing Wang, Si-Wan Wen, Guang-Rong Yu (2014) Isolated avulsion fractures of lesser tuberosity humerus: a case report and review of the literature. Int J Clin Exp Med 7(3): 780-784.
- Nikolaou VS, Chytas D, Tyrpenou E, Babis GC (2014) Two-level reconstruction of isolated fracture of the lesser tuberosity of the humerus. World J Clinical Cases 2(6): 219-223.
- Seeli DR, Sasapu SR, Dhavala BS, Vaddiraju VS (2014) Isolated lesser tuberosity avulsion with rupture of long head of biceps. J Orthop Traumatol Rehabil 7: 172-175.
- Alexandre Tadeu do NascimentoI, Gustavo Kogake ClaudioI, Pedro Bellei RochaI (2018) Arthroscopic treatment for a chronic isolated avulsion fracture of the lesser tuberosity of the humerus: a case report. MOJ Sports Med 2(1): 24-26.
- Jaya TS, Hadizie D, Muzaffar TMS (2019) Isolated avulsion fracture lesser tuberosity of the humerus, a rare presentation post seizure. Trauma Cases Rev 5: 078.
- Amyn M Rajani, Urvil A Shah, Meenakshi S Punamiya (2021) Lesser tuberosity avulsion fracture: A rare case report. Journal of Orthopaedic Case Reports 11(12): 11-14.
- Ryan Cheng, Jay Moran, Samantha Smith, Don Li, Christopher A, et al. (2021) Lesser tuberosity avulsion fracture in an 11-year-old baseball player due to batting. Case Reports in Orthopedics.
- te Slaa RL, van Laarhoven HAJ, van Laarhoven EW (1996) Isolated avulsion fracture of the lesser tuberosity of the humerus. A report of six cases. Journal of Shoulder and Elbow Surgery 5(2, Part 2): S21.
- Paschal SO, Hutton KS, Weatherall PT (1995) Isolated avulsion fracture of the lesser tuberosity of the humerus in adolescents. A report of two cases. J Bone Joint Surg Am 77(9): 1427-1430.
- Ross GJ, Love MB (1989) Isolated avulsion fracture of the lesser tuberosity of the humerus: report of two cases. Radiology 172(3): 833-834.
- Kuroda T, Go G, Ojima S, Nishi S, Mizuno K (1993) Isolated avulsion fracture of the lesser tuberosity of the humerus: A case report. Journal of Shoulder and Elbow Surgery 2(4): 221-224.
- Shibuya S, Ogawa K (1986) Isolated avulsion fracture of the lesser tuberosity of the humerus. A case report. Clin Orthop Relat Res (211): 215-218.
- Earwaker J (1990) Isolated avulsion fracture of the lesser tuberosity of the humerus. Skeletal Radiol 19(2): 121-125.
- Klasson SC, Vander Schilden JL, Park JP (1993) Late effect of isolated avulsion fractures of the lesser tubercle of the humerus in children. Report of two cases. Journal of Bone and Joint Surgery - Series A 75(11): 1691-1694.
- LaBriola JH, Mohaghegh HA (1975) Isolated avulsion fracture of the lesser tuberosity of the humerus. A case report and review of the literature. J Bone Joint Surg Am 57(7): 1011.
- Caniggia M, Maniscalco P, Picinotti A (1996) Isolated avulsion fracture of the lesser tuberosity of the humerus. Report of two cases. Panminerva Med 38(1): 56-60.
- McGuinness JP (1939) Isolated avulsion fracture of the lesser tuberosity of the humerus. The Lancet 233(6027): 508.
- Thielemann FW, Kley U, Holz U (1992) Isolated injury of the subscapular muscle tendon. Sports Injury Sports Damage 6(1): 26-28.
- Kunkel SS, Monesmith EA (1993) Isolated avulsion fracture of the lesser tuberosity of the humerus: A case report. Journal of Shoulder and Elbow Surgery 2(1): 43-46.
- Vavken P, Bae DS, Waters PM, Flutie B, Kramer DE (2016) Treating subscapularis and lesser tuberosity avulsion injuries in skeletally immature patients: A Systematic Review. Arthroscopy 32: 919-928.
- Cottias P (1998) Fractures of the lesser tuberosity of the humerus. Rev Chir Orthop Reparatrice Appar Mot 84: 137-139.
- Berbig R, Keller H, Metzger U. Isolated fracture of the lesser tuberosity of the humerus: case reports and review of the literature. Journal for Trauma Surgery and Insurance Medicine: Official Organ of the Swiss Society.
- Kanso I, Bricout JM (1998) Isolated avulsion fracture of the lesser tuberosity of the humerus: A case report. Journal of Orthopedic and Restorative Surgery of the Motor Apparatus 84(6): 554-557.
- Zanlungo U, Manetti G, La Cavera F (1994) Isolated avulsion fracture of the lesser tuberosity of the humerus. A case report. Minerva Ortopedica e Traumatologica 45(3): 97-99.
© 2022 Alex N Karanja. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






