- Submissions

Full Text
Orthopedic Research Online Journal
Extensor Pollicis Longus Tendon Delayed Rupture Following a Minimally Displaced Distal Radius Fracture in Adolescence
Awdhah A Al-Samhan1*, Ali N AL-Khayat2 and Ali A Jarragh3
1Department of Orthopedic Surgery, Al-Razi Orthopedic Hospital, Kuwait
2Department of General Surgery, Mubarak Hospital, Kuwait
3Department of Surgery, Faculty of Medicine, Kuwait university, Kuwait
*Corresponding author: Awdhah A Al-Samhan, Department of Orthopedic Surgery, Al-Razi Orthopedic Hospital, Kuwait
Submission: June 10, 2022;Published: June 20, 2022

ISSN: 2576-8875 Volume9 Issue4
Abstract
Extensor Pollicis Longus tendon (EPL) delayed rupture following a minimally displaced distal radius fracture is considered a rare complication. Up to our knowledge cases are even less frequent in the adolescence and there is limited literature on this subject. We present a case of delayed rupture of EPL tendon post minimally displaced distal radius fracture in a 16-year-old male, that was managed surgically. The best preventive measure is high index of clinical suspicion for this type of injury.
Keywords:Extensor tendon Rupture; Interphalangeal joint; Tendon rupture; Extensor pollicis longus distal radius fracture
Introduction
Extensor Pollicis Longus (EPL) muscle, which is located in the third extensor compartment, is part of the deep group of dorsal forearm muscles originating from the posterior surface of the middle third ulna and interosseous membrane. The muscle runs laterally, and it passes through the forearm, passes over Lister’s tubercle and inserts in the posterior aspect of base of distal phalanx of the thumb, as it crosses the wrist, the muscle becomes a tendon which forms the medial border of the anatomical snuff box. The EPL tendon main blood supply comes from the Anterior interosseous artery which supplies the first part of the EPL tendon prior to the synovial sheath, the second blood supply is the radial artery which supplies the tendon after the synovial sheath. The tendon main function is extension of the thumb at the terminal phalanx and adduct the thumb at metacarpophalangeal (MCP) and interphalangeal (IP) joints [1,2].
EPL ruptures in literature was first reported by Duplay in 1876 [3] the most common etiologies were found to be associated with underlying systemic diseases such as rheumatoid arthritis, history of use of systemic or local steroids, trauma in the form of repetitive excessive abnormal motion of the wrist joint or displaced distal radius fracture. In a study conducted in 2018 the incidence of EPL rupture and distal radius fracture in adult found to be ranging between 0.4% to 5% [4], but the literature on this subject regarding the incidence in adolescence population is limited and study groups are usually small. In a 2014 a study review mentioned that there are only nine cases in the English literature regarding delayed EPL tendon rupture in young population, five of which were not reported in detail [5].
Multiple vascular and mechanical theories to support and describe the delayed presentation of tendon rupture were mentioned, the classic 1979 study by Engkvist and lunborg [4] described the vascular theory which state that poor vascularity around the lister tubercle make the area more prone to ischemic changes after any insult also hemorrhage after a trauma into an intact tendon sheath may leads to increased pressure within the closed sheath resulting in decreasing blood supply that may weaken the tendon and lead to ischemic atrophy . The mechanical theory can explain the EPL delayed as a result of callus friction against the EPL tendon which is held intact in its extensor retinaculum sheath in non-displaced fractures.
In this case report we present a case of spontaneous delayed rupture of EPL tendon after distal radius minimally displaced fracture in a sixteen-year-old male, the aim of addressing the case is that earlier recognition for this unusual presentation will provide surgeons with high index of clinical suspicion for this type of injury which might provide earlier surgical management that may eventually improve the outcome of patients.
Case Presentation
A 16-year-old male previously healthy with no known medical history, rheumatologically disease systemic or local steroid use, was brought to the hospital by ambulance to the emergency room after fall from height (third floor) due to a suicidal attempt with multiple body fractures.
Bilateral distal end radius fracture: right side was managed with open reduction and internal fixation by volar plate (Figure1). Left side minimally displaced fracture managed conservatively with splint immobilization (Figure 2). Left Pilon fracture, for which he had open reduction and internal fixation. Bilateral calcaneal fracture and right subtalar dislocation managed with open reduction and internal fixation. Right nondisplaced transverse acetabular fracture managed conservatively. High transverse S1 fracture dislocation (limbo-pelvic dissociation) causing cauda equina at presentation with stool and urine incontinence. This injury was managed with neurological decompression (laminectomy of the sacral vertebrae 1-4) and tension band plating of the comminuted sacral fracture.
Figure 1:Plain radiograph showed anteroposterior and lateral view of the right distal radius managed with open reduction and internal fixation by volar plate: (A) anteroposterior view (B) lateral view.
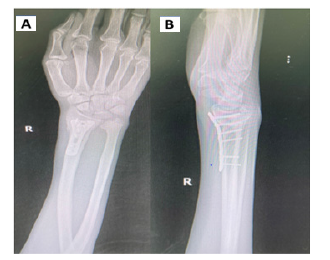
Figure 2:Plain radiograph showed anteroposterior and lateral view of the left. minimally displaced fracture managed conservatively with splint immobilization: (A) anteroposterior view (B) lateral view.
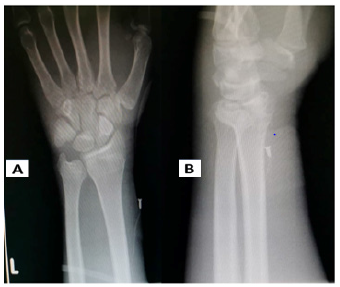
During daily rounds post trauma day 15, the patient complained of a sudden inability to extend his left thumb; this incident was painless. No swelling or discoloration was noticed in the hand. The examination revealed the inability to extend the left thumb at interphalangeal joint, the sensory nerve examination was intact, patient was able to extend his ring and little finger without any difficulty. The complete blood cell count, erythrocyte sedimentation rate, and C-reactive protein were within normal range. The rheumatoid factor as well as Anti-CCP were negative. A study of the plain radiographs revealed minimally displaced distal radius fracture with no other associated injuries.
Rupture of the EPL tendon was confirmed by ultrasound and by clinical due to inability to do MRI because of the presence of incompatible MRI implants from previous surgeries. Radiographs of the left hand and wrist demonstrated a healing minimally displaced extra-articular distal radius fracture.
The patient was consented for a possible reconstructive procedure “Extensor Indicis Proprius (EIP) to EPL transfer” to restore his thumb function in addition to Kirschner(K)-wire fixation of the minimally displaced distal radius fracture in the same operation setting. In our patient, the EPL tendon repair was first approached through a dorsal incision, the distal stump of the EPL found to be divided at the level of the dorsal tubercle of the radius, was found not in a condition that permit direct repair. The decision of EIP transfer was taken intraoperatively. There was no bony irregularity, no bony spicule and no prominent Lister’s tubercle evident at the time of the tendon transfer. Proper tensioning was achieved to maintain good tendon post-operative healing. The minimally displaced fracture of the left distal radius was approach next by K-wire fixation under radiographic guidance (Figure 3). Our post-operative protocol involved immobilization using a short-arm cast, keeping the wrist in a neutral position and the thumb in ulnar deviation and extension, it was maintained for 6 weeks, through the 6 weeks’ patient was evaluated in the outpatient clinic, for wound evaluation and x-rays, rehabilitation exercises planned after cast and K-wire removal to restore function (Figure 4).
Figure 3:Plain radiograph showed anteroposterior and lateral view of the left minimally displaced fracture managed by K-wire fixation under radiographic guidance: (A) lateral view (B) anteroposterior view.
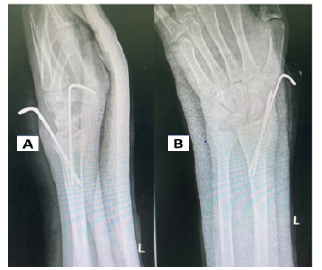
Figure 4:(A) A photo of the hand showing the k-wire fixation and post-operative scars. (B) A short- arm cast was used to keep the wrist in neutral position, and thumb in extension and ulnar deviation.

Discussion
EPL rupture is mostly reported in adult population with comorbidities, trauma or history of steroid use. The incidence of spontaneous EPL rupture following distal radius fracture has been found in literature between 0.3% to 5% [6]. It is mostly reported in adults with nondisplaced distal radius fractures. Delayed rupture of the EPL tendon in adolescent population after minimally displaced distal radius fracture is uncommon and to our best knowledge is rarely reported in the literature. In a 2014 a study review mentioned that there are only nine cases in the English literature regarding delayed EPL tendon rupture in young population, five of which were not reported in detail [5].
The theories of delayed presentation can be best explained with effusion or bleeding inside the intact synovial sheath that may affect the microvasculature around the tendon which may lead to tendon atrophy and delayed tendon rupture. Fracture callus can also decrease space for EPL tendon which can cause pressure and irritation to the tendon or can affect synovial fluid nutritional exchange, eventually resulting in necrosis, tendon atrophy and EPL tendon rupture.
Study conducted in 2015 [7,8] in adult population suggested that hematoma evacuation or needle aspiration after a nondisplaced fracture can reduce the incidence of EPL delay rupture, further studies are needed to confirm this theory specially in young population.
However, management of the rupture tendon depend on the tendon condition during surgical exploration and the management is similar between adults and young population. The management options are direct tendon repair, tendon transfer or tendon graft, most authors recommend tendon transfer and in our case EPI tendon transfer was performed. The reason why EPI tendon transfer is commonly performed because it has a similar amplitude and direction of pull to the EPL which will provides predictable good functional outcome after rehabilitation.
Early clinical evaluation and a high index of suspicion can allow early diagnosis, which will help in avoidance and decrease the incidence of reconstructive surgery and its associated rehabilitation and possible future complication.
Conclusion
The incidence of delay Rupture of the EPL tendon in adolescence is rare, few cases up to our knowledge were found to be reported in literature, the injury associated usually with highly displaced distal radius fracture, patient with co-morbidities, or history of steroid use. However, it is even more rare to be present in non-displaced or minimally displaced distal radius fractures. In our particular case of delayed presentation of rupture EPL tendon post minimally displaced distal radius fracture in a 16-year-old male, surgical intervention EPL tendon transfer and K-wire fixation were chosen to improve patient outcome and quality of life. Owing to rarity of the condition the best prevention measure is high index of clinical suspicion for this type of injury that will enable treating surgeons to provide earlier surgical management which may improve the outcome of patients. Further studies are needed to evaluate the incidence of presentation and treating methods thus facilitating the development of evidence-based therapy.
Declaration of Patient Consent
The authors declare that informed consent has been granted for this case from patient and parents for his images and clinical information to be reported in the journal. Patient and parents understand that his name and initials will not be published, effort will be made to conceal identity, but anonymity cannot be guaranteed
Competing interests
The authors declare that they have no competing interests.
Authors contributions
1-Dr. AA: Prepared the study design, collect the necessary data,
literature review of similar case, writhing the drafts, responsible for
roles allocation and keeping the team on schedule to timeframe.
2-Dr. AN: Literature review of similar case, collect images used
in report, responsible for patient counseling regarding the consent
3- Dr. AJ: The treating surgeon, presented the case a case of
interest for the report, revised the final draft of the manuscript.
All authors reviewed and accepted the final draft of the manuscript with the corresponding figures and are responsible for the content and similarity index of the manuscripts.
References
- Moore KL, Daley AF, Agur AMR (2014) Clinically Oriented Anatomy (7th edn), Philadelphia, Lippincott Williams & Wilkins, PA, USA, P. 758.
- (2014) Standring S, Gray's Anatomy (41st edn), Edinburgh: Elsevier Churchill Livingstone. Netter F, p. 880.
- (2016) Atlas of Human Anatomy (6th edn), Philadelphia, Saunders, PA, USA, 398: e113.
- Hove LM (1994) Delayed rupture of the thumb extensor tendo A 5-‐year study of 18 consecutive cases. Acta Orthop Scand 65(2): 199--203.
- Review Article Advances in Orthopedics and Sports Medicine AOASM-132 ISSN: 2641-6859.
- Brooker B, Harris PC, Donnan LT, Graham HK (2014) Rupture of the extensor pollicis longus tendon following dorsal entry flexible nailing of radial shaft fracture in children. Advances in Orthopedics and Sports Medicine J child Orthop 8: 3537.
- Eno JJT, Yao J (2017) Bilateral spontaneous delayed extensor pollicus longus ruptures following distal radius fractures: A case report and review of the literature. Ann Clin Case Rep 2:
- Gary M Lourie, Andrew Putman, Taylor Cates, Allan E Peljovich (2015) Extensor pollicis longus ruptures in distal radius fractures: Clinical and cadaveric studies with a new therapeutic intervention. Am J Orthop 44(4): 183-‐
© 2022 Awdhah A Al-Samhan. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






