- Submissions

Full Text
Orthopedic Research Online Journal
Day Hospital Facility, An Inpatient Alternative for Pediatric Spinal Cord Injury Care
Juan M Talavera-Mosquera1, Irene García Camacha2, Raúl M Martín2, Melchor Álvarez de Mon-Soto3 and Elisa López-Dolado4*
1Staff Physiatrist, Rehabilitation Department, Hospital Nacional de Parapléjicos of Toledo, Spain
2Tenured Professor, Department of Mathematics, Toledo School, Universidad de Castilla-La Mancha, Spain
3Head of Internal Medicine Department, Hospital Universitario Príncipe de Asturias de Alcalá de Henares, Spain
4Chief Clinician of the Rehabilitation Department, Hospital Nacional de Parapléjicos de Toledo, Spain
*Corresponding author: Elisa López-Dolado, Pediatric Spinal Cord Injury Unit, Hospital Nacional de Parapléjicos of Toledo, Associate Professor, Department of Medicine and Medical Specialties, School of Medicine, Universidad de Alcalá de Henares, Spain
Submission: May 13, 2022;Published: May 23, 2022

ISSN: 2576-8875 Volume9 Issue4
Abstract
Study design: Observational retrospective study.
Background: The present work was aimed to determine if the founding of a day patient facility (DPT) was able to optimize inpatient (IP) effectiveness measures and if there were differences in the patient’s clinical profile depending on the modality of care. Setting: Pediatric Unit of the Hospital Nacional de Parapléjicos of Toledo (Spain).
Methods:All the children attended, both IP and outpatient, were analyzed throughout two different years: 2006, the year immediately prior to the start-up of the DPT facility, and 2015, ten years after its foundation. A descriptive and inferential statistical analysis was performed for the study purpose.
Results: In 2006, there were different 75 inpatient children treated. From the 156 patients attended in 2015, 16.7% reported receiving IP regime, 61.5% DPT regime, and 21.8% in combined modality (CM). The average age of DPT was significantly lower than IP (P<0.01). Almost half of IPs processes exhibited AIS A SCI in both years (46.7% in 2006, and 46.2% in 2015), while a 67.7% of DPT patients showed AIS C or D in 2015. With respect of the hospitalization activity monitoring, we found that the presence of a DPT involved an increase in the IP average length of stay (from 20.83 to 39.78 days) and bed occupancy (from 27.72% to 42.04%) with a decrease in the bed turnover (from 4.86 to 3.86).
Conclusion:A DPT facility is able to improve the healthcare of pediatric SCI children by optimizing the use of IP resources.
Introduction
Despite having a relatively low incidence, pediatric spinal cord injury (PedSCI) is a very significant central nervous system disability, with enormous health and emotional costs, not only for patients but also for both their families and community. The incidence of PedSCI varies between regions and countries [1]. Mechanisms, patterns, and injury severity have shown to be different not just with age or race but with the access to medical care, depending on the type of the health care system [2]. The most cost-effective solution to minimize sequelae and optimize final functional level is the integrated management within a specialized unit [3]. Inpatient regime (IP) that includes rehabilitation facilities is the gold standard therapeutic modality, both for the acute and subacute stages or even for some of the chronic forward complications. During the last decade, a constant increase in the number and complexity of the PedSCI cases has been reported, which together with a decrease in mortality rates shows clear improvements in medical management to this very vulnerable population [4,5]. IP, although costly, is usually seen as the best care alternative, in spite of requiring a team of expert professionals, a good amount of material resources, a huge investment of emotional and physical effort and a great deal of time on the part of the child’s family. Common secondary complications after a PedSCI included spinal, hip and feet deformities, bone fractures, urinary tract infections, bowel problems, spasticity and pain, addressing the greater rates of contacts with the healthcare system and the need of multiple rehospitalization through the patient’s lifetime [6]. To make sustainable all these expensive health attentions, both from the patient’s well-being point of view and from the hidden costs that their attention generates, a few alternatives to IP have been proposed [7]. In the last decade, some evidence-based IP alternative programs providing acute hospital-equivalent care to adult patients with acute/subacute SCI in the comfort of their home had been implemented and had been successful to demonstrate a decreasing in the length of stay, improvements in patient access, and an increasing in-patient satisfaction [8]. Among adult SCI population, these home-hospitalization programs help to deal with the common discharge barriers at the end of the rehabilitation period, whose consequence is additional unnecessary days in hospital, and represent a great improvement opportunity for the health care systems [9].
' 'Very few studies focused on the hospitalization alternatives in PedSCI population have been carried out. Socioeconomic disparities for trauma-related outcomes have been described in this population, so the more impoverished the child, the higher the injury incidence, severity, mortality and poor functional outcome rates [10]. But no evidence of higher medical costs per inpatient of lower household income has been addressed among children with severe Traumatic Brain Injury (TBI) and Spinal Cord Injury (SCI) disability [11]. Although these last data must be carefully interpreted, they do reflect the different role played by socioeconomic factors, family and community support in pediatric population compared to adults, and therefore, the need to specifically design pediatric hospitalization-alternative modalities.
Day patient treatment (DPT) is a less expensive health care modality that has shown efficient in other pathologies as anorexia nervosa for avoiding problems of relapse and readmission by easing the transition from hospital to home [12]. However, the effectiveness of different regimes of heath care without hospital admission to correctly manage mental health diseases among young patients remains controversial [13]. Although it makes sense to propose that, the DPT as an alternative to the IP, could provide great benefits for PedSCI population, to our knowledge it has not yet been addressed. On the other hand, while there are several indicators that measure hospitalization adequacy (since they have shown to be useful for the monitoring of the health care activity over time and also allow comparisons with other units and / or centers [14,15]), no such metrics have been yet designed to evaluate the new hospitalization-alternative modalities neither for children nor for adults, at least in the Spanish health system.
The present work was aimed to determine if the establishment of a pediatric DPT in a Spanish SCI monographic hospital was able to optimize the pediatric hospitalization effectiveness measures. It was also analyzed if there were differences in the patient’s clinical profile depending on the modality of care.
Methods
Study design and participants
We carried out an observational retrospective analysis of all the PedSCI children attended throughout two different years in a 212-bed national SCI monographic hospital in Spain: 2006, the year immediately prior to the start-up of the DPT facility, and 2015, ten years after its foundation and with the DPT area at full capacity. The study obtained approval from the local Clinical Research Ethics Committee. During the years studied, the workers template assigned to the Unit under study remained unchanged: 1 physician, 12 nurses, 3 physiotherapists and 2 occupational therapists, all of them full-time plus 1 secretary and 1 social worker, both of them part-time.
In order to accurately stratify the patients sample, three models of care attention were defined depending on the area where the clinical care processes was carried out: 1) IP regime, in which all the clinical processes were put into effect only in the hospitalization area; 2) DPT regime, in which all the processes were effectuated in the DPT area exclusively, and finally 3) combined modality (CM), in which the patients were treated both in IP or in DPT facility, depending of the nature of the process attended.
Inclusion/exclusion criteria
All patients between 0 and 18 years old, with acute or chronic spinal cord injury, assessed during 2006 and/or 2015 in the National Paraplegics Pediatric Unit of Toledo (Spain) were included in the present study. A total of 75 different children were attended in IP regime in the year 2006, that generated a total of 102 clinical processes, compared to the 156 ones attended in 2015, 26 of them in IP regime and the other 130 in DPT or CM regime, that generated a total of 81 clinical processes in IP and CM related to hospitalization, and 413 in DPT or CM regimes involving DPT facility.
Those patients in whom SCI was ruled out and/or those over 18 years old at the start of the study were excluded (meaning, 2 patients attended in IP regime in 2006 and 60 patients in 2015, only 3 of them attended in the hospitalization area).
Sources
Two different types of information sources were handled: the official healthcare activity data provided by the National Paraplegic Hospital Admission Service [16,17] and the whole clinical reports of discharge issued along the 2006 and 2015. In order to avoid biases and ensure the patients’ clinical data confidentiality, all documents were handled after removing their filiation data. All participants provided their informed consent.
Demographics
The following demographic variables were recorded for each process, both in IP as in DPT regimes or in combined modality: age, sex, place of origin and etiology, level and severity of SCI, these last two variables according to the international standards for neurological classification of spinal cord injury [18].
Health care activity monitoring
To analyze IP regime in the two selected years, the total number of health care processes per patient and year and the total number of days of admission per patient and year were collected. As hospitalization effectiveness measures, three indicators were chosen and registered: the average length of stay (the total sum of stays in a particular period, divided by the total number of admissions in the same period), the bed occupancy (the average proportion in a period of time in which the beds have actually been occupied by a patient, with respect to their maximum occupancy capacity) and the bed turnover (the number of admissions per bed in a given period of time) [17]. These indicators have shown to be useful for the monitoring of the care activity over time and also allow comparison with other units and / or centers [15,19,20].
To analyze the activity in the DPT facility, the total number of processes per patient and year was recorded for both the DPT and the CM regimes.
Statistical Analysis
Statistical analysis was performed by using the Statistical Package for the Social Sciences software IBM SPSS Statistics 24. A descriptive analysis of the hospital effectiveness indicators and sociodemographic variables was carried out. Multivariate and univariate analysis of variance (MANOVA and ANOVA respectively) were conducted to determine if there were differences in study variables between groups of care attention models. Subsequent pairwise comparisons were performed using Games-Howell post hoc test. To detect associations between therapeutic modalities and categorical demographic variables, Chi-squared tests were conducted. The significance level was defined as P<0.05 in all statistical evaluations.
Results
In 2006, there were 75 inpatients treated at pediatric unit of the National Paraplegic Hospital Admission Service. From the 156 patients attended in 2015, 16.7% reported receiving IP regime, 61.5% DPT regime, and 21.8% in CM regime. Patient’s demographics for these time periods are represented in Table 1. Univariate analysis of variance showed significant differences between the averages of age of the patients treated at the different therapeutic modalities (P<0.01). A post-hoc analysis let us to explore the pairs of care attention modalities whose averages of age resulted to be statistically different. The average of age was significantly lower in DPT (9.89±5.13 years) than IP regime in 2015 (13.77±4.34 years). Figure 1(A) graphically supports this result. Consequently, the frequency distribution between the age groups was statistically different depending on the received attention regime (P<0.05). The ages of DPT group were lower (39.5% from 0 to 8 years old) from than IP group in both years (26.7% from 0 to 8 years old in 2006 and 15.3% from 0 to 8 years old in 2015). No significant differences were found regarding gender. Another key issue to show the effect of the DPT facility is the geographical origin of the patients. Three categories were created for this purpose: 1) patients coming from the same region, 2) patients coming from neighboring regions (according to Spanish territorial organization), and 3) patients coming from distant regions. Significant statistical differences in the provenance were found concerning the model of care attention: 41.7% of the DPTs came from the same region, whereas the 21.3%, 15.4% of the IPs in 2006 and 2015 respectively, and 20.6% of the CMs came from the same region. In addition, the existence of the DPT facility increased the number of inpatients coming from distant regions (from 12% in 2006 to 26.9% in 2015).
Table 1: Demographic data for the different therapeutic modalities in 2006 and 2015.
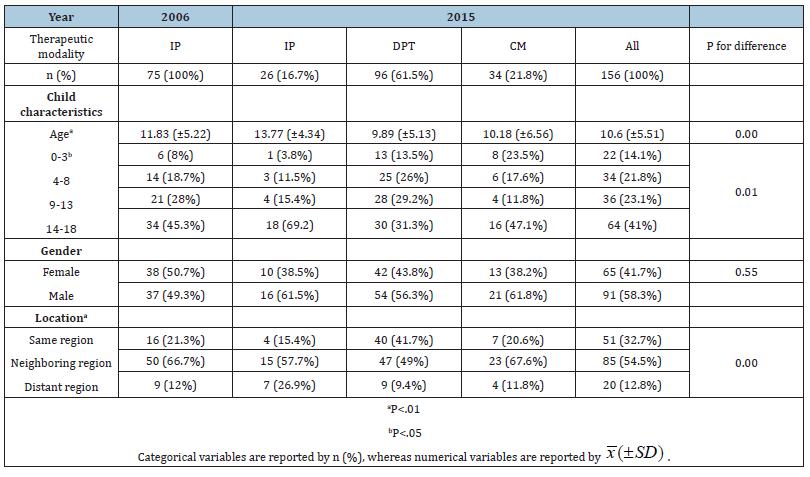
Figure 1:A) Box plot of the age distribution of the patients treated at the different therapeutic modalities in 2006 and 2015. B) Bar char of the frequency distribution (given in percentage) of ASIA levels for each model of care attention in 2006 and 2015.
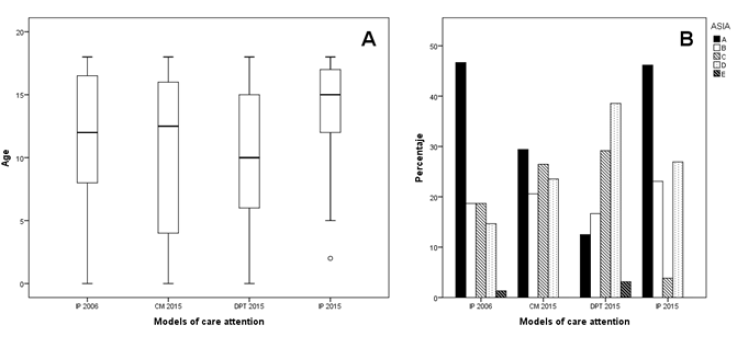
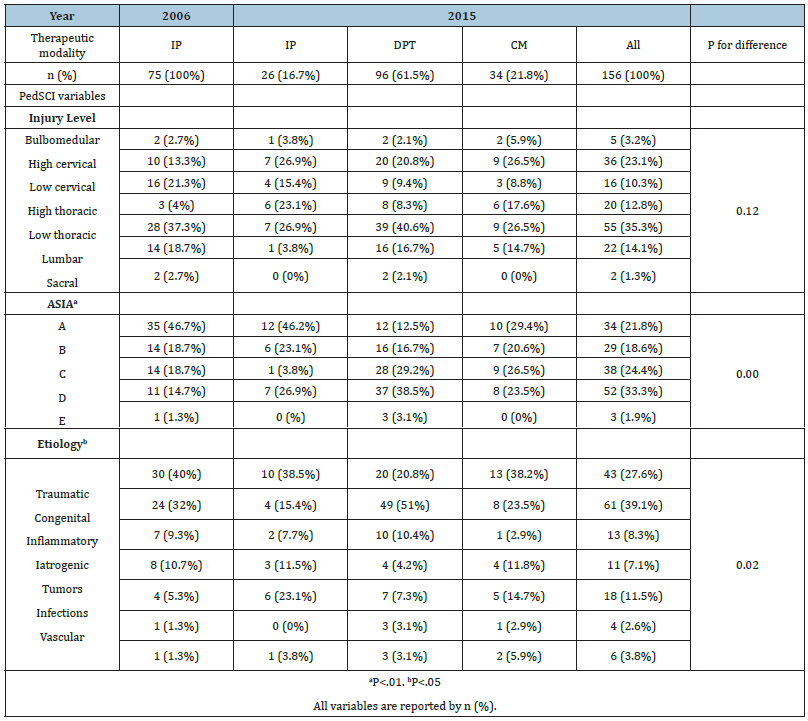
Despite observing slight variations in the patient distribution depending on injury level (Table 2), there were no statistically significant differences between therapeutic modalities. Regarding the SCI severity, almost half of IPs in both years 2006 and 2015 exhibited AIS A lesions (46.7% and 46.2% respectively), while a 67.7% of DPTs showed AIS C or D ones. Patients receiving CM were distributed in a balanced way from AIS A to D SCI severities (29.4%, 20.6%, 26.5% and 23.5% from AIS A to D, respectively). Therefore, DPT and CM regimes significantly received patients with more incomplete PedSCI than IP regime (P<0.01). Figure 1(B) illustrates this result. It may also be noticed that a few numbers of patients were gathered in some categories. Regarding SCI etiology, significant differences were found between the studied care attention modalities (P=0.02). Most patients attended in IP (40% in 2006 and 38.5% in 2015) and CM (38.2% of the patients) suffered traumatic injuries, whereas a 51% of those patients receiving DPT facility reported congenital injuries, mostly spina bifida.
Table 2: PedSCI characteristics of the patients treated at different therapeutic modalities in 2006 and 2015.
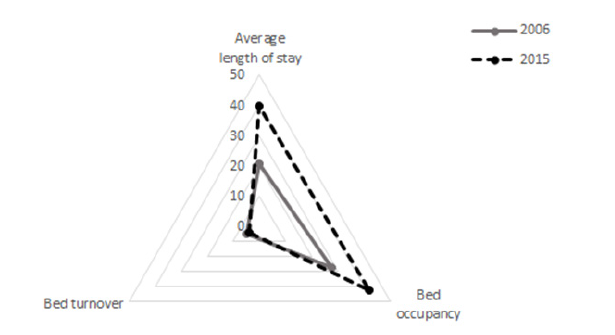
As it was mentioned before, the average length of stay, the bed occupancy and the bed turnover index are the most widely used indicators in Spain to measure the hospitalization effectiveness. A comparative of the obtained indicators in both years, 2006 and 2015, is depicted in Figure 2. The existence of a DPT facility involved a substantial increase in the average length of stay (from 20.83 days in 2006 to 39.78 days in 2015) and the bed occupancy (from 27.72% in 2006 to 42.04% in 2015) and consequently, a slight decrease in the bed turnover was observed (from 4.86 in 2006 to 3.86 in 2015).
Figure 2:Indicators of hospitalization effectiveness in 2006 and 2015.
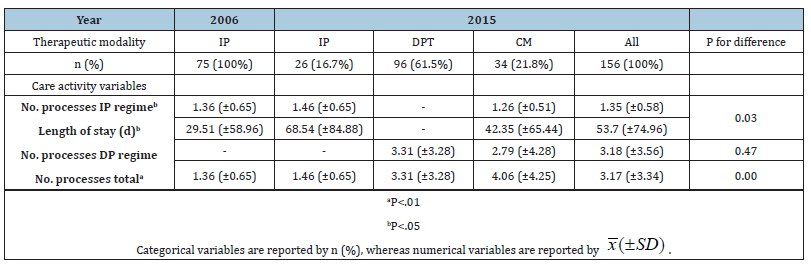
In order to statistically infer the previous results regarding heath care activity, variables involved in the previous indicators as well as other care activity variables were analyzed (Table 3). Multivariate analysis of variance (MANOVA) reported significant differences in the average number of processes and the average length of stay between groups of patients receiving IP regimen in 2006, IP regime in 2015 and CM regimen in 2015 (P=0.03). Patients requiring only hospitalization in 2006 compared with those of 2015 had a lower average length of stay (from 29.51±58.96 days in 2006 to 68.54±84.88 days in 2015), while patients attending CM regime remained hospitalized an average of 42.35±65.44 days. The same trend was observed regarding the average number of processes, although the differences between values became were less pronounced (1.36±0.65 processes and 1.46±0.65 processes in patients attending IP regimen in 2006 and 2015 respectively; and 1.26±0.51 processes for CM regime patients). As far as the authors know, there is not an indicator of the care activity for DPT as a standard, at least in Spanish health care system. Therefore, care activity of DPT and IP may be only fairly compared in terms of number of processes. A new variable, total number of processes, was created reporting the total sum of processes registered by the patient either IP or DPT areas. Univariate analysis of variance (ANOVA) revealed significant differences between the average total number of processes depending on the received therapeutic modality (P<0.01). Post hoc analysis showed that the average total number of processes was significantly higher in DPT and CM regimes (3.31±3.28 and 4.06±4.25 processes respectively) than IP regime in both years 2006 and 2015 (1.36±0.65 and 1.46±0.65 processes respectively).
Table 3: Indicator variables of the care activity for the different therapeutic modalities in 2006 and 2015.
Discussion
In this work, the organizational consequences and changes in the pediatric population profile in a monographic unit of PedSCI after the creation of a DPT facility has been analyzed.
Thanks to the DPT regime, it was possible to significantly increase healthcare activity, mostly “capturing” in the DPT a new group of younger patients, with more incomplete SCI and, consequently, better functional prognosis. The total number of processes attended was around almost five times higher in 2015 than in 2006 (494 vs 102) with the same workforce, which necessarily implies an optimization of the resources directly due to organizational changes.
Interestingly, the predominant etiology among those “new” patients was non-traumatic, particularly congenital, thus being the course of their disability more insidious and therefore, less urgent the rehabilitative interventions in a monographic unit like ours, but not less necessary. Another interesting point is the fact that the IP regime patients’ profile has remained unchanged in both studied years, attending mostly complete traumatic SCIs in elder children and adolescents. As no statistically significant differences were found in the level of the SCI between DPT ó CM with respect to IP, it could not directly be assumed that the more severe the lesion, the more complex the management and the more likely the need for hospitalization. A clear increase in the average length stays and the bed occupancy with a slight decrease in the bed turnover (Figure 2) could be easily interpreted as a worsen in the IP effectiveness indicators. But if they are analyzed in the context of the abovementioned data, they indicate a better use of the hospitalization resources, since all those short hospital stays that in 2006 were necessary to carry out, for example, invasive diagnostic procedures, were performed in 2015 in the DPT facility. The lack of new therapeutic paradigms in the SCI field that could substantially modify the PedSCI outcome and prognosis in the past decade, together with the absence in the scientific literature of data that suggest a relevant increase in the PedSCI incidence [1,2] supports the fact that all the changes described in this work are related to a greater or lesser extent to the existence of the DPT facility and the organizational changes it brought about.
To the authors knowledge, no other published works had proposed to manage PedSCI in a DPT regime as an alternative to IP, so comparisons are not feasible. Nevertheless, a DPT facility have shown to be able to adequately control non-chronic anorexia nervosa in the adolescent patients, what makes it a safe and costeffective alternative to IP [12].
A clear limitation of this work is that it has not analyzed the potential clinical impact, be it good or bad, over the development of chronic complications of the SCI, as the main goal of the periodic follow-up throughout the growth and development period is to prevent and to treat them precociously. Another issue that must be explored after the present work is the development of reliable effective indicators to accurately measure DPT regimes healthcare activity. It is our desire to continue working in that research line.
In conclusion, a DPT facility inside of a monographic PedSCI unit has improved healthcare activity, not only by increasing the number of patients attended but also by handling a widespread range of etiologies, severities and ages, thus optimizing the use of IP resources. DPT and CM regimes are useful conventional hospitalization alternatives and their creation may be promoted.
References
- GBD 2016 Traumatic brain injury and spinal cord injury collaborators (2019). Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 18(1): 56-87.
- Joseph H Piatt (2015) Pediatric spinal injury in the US: epidemiology and disparities. J Neurosurg Pediatr. 16: 463-471.
- Illis LS (2004) The case for specialist units. Spinal Cord 42: 443-446.
- Gregory W Poorman, Frank A Segreto, Bryan M Beaubrun, Cyrus M Jalai, Samantha R Horn, et al. (2019) Traumatic fracture of the pediatric cervical spine: Etiology, epidemiology, concurrent injuries, and an analysis of perioperative outcomes using the kids’ inpatient database. International Journal of Spine Surgery. 13(1): 68-78.
- Ocete Hita E (2011) Towards the future in pediatric intensive care. Med Intensiva 35(6): 328-330.
- Munce Sep, Perrier L, Tricco AC, Straus SE, Fehlings MG, et al. (2013) Impact of quality improvement strategies on the quality of life and well-being of individuals with spinal cord injury: a systematic review protocol. Systematic Reviews. 2: 14.
- Ogilvie D (2013) Hospital based alternatives to acute paediatric admission: a systematic review. Arch Dis Child 90: 138-142.
- Madaris LL, Onyebueke M, Liebman J, Martin A (2016) SCI hospital in home program: Bringing hospital care home for veterans with spinal cord injury. Nurs Adm Q 40(2): 109-114.
- New PW (2015) Prospective study of barriers to discharge from a spinal cord injury rehabilitation unit. Spinal Cord 53(5): 358-362.
- Cassidy LD, Lambropoulos D, Enters J, Gourlay D, Farahzad M, Lal DR (2013) Health disparities analysis of critically ill pediatric trauma patients in Milwaukee, Wisconsin. J Am Coll Surg 217: 233-239.
- Zonfrillo MR, Zaniletti I, Hall M, Fieldston ES, Colvin JD, et al. (2016) Socioeconomic status and hospitalization costs for children with brain and spinal cord injury. J Pediatr 169: 250-255.
- Herpertz-Dahlmann B, Schwarte R, Krei M, Egberts K, Warnke A, et al. (2014) Day-patient treatment after short inpatient care versus continued inpatient treatment in adolescents with anorexia nervosa (ANDI): a multicentre, randomized, open-label, non-inferiority trial. Lancet 383: 1222-1229.
- Shepperd S, Doll H, Gowers S, James A, Fazel M, et al. (2009) Alternatives to inpatient mental health care for children and young people. Cochrane Database Syst Rev 2009 (2): CD006410.
- Hussey PS, De Vries H, Romley J, Wang MC, Chen SS, et al. (2009) A systematic review of health care Efficiency measures. Health Serv Res 44(3): 784-805.
- Bernal-Delgado E, García-Armesto S, Oliva J, Sánchez Martínez FI, Repullo JR, et al. (2018) Spain: health system review. Health Systems in Transition 20(2): 1-179.
- http://hnparaplejicos.sescam.castillalamancha.es/es/quienessomos/memorias-anuales
- https://www.slideshare.net/rogufe/memoria-del-servicio-de-salud-de-castillala-mancha-sescam-2006
- Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, et al. (2011) Reference for the 2011 revision of the international standards for neurological classification of spinal cord injury. The Journal of Spinal Cord Medicine 34(6): 547-554.
- Cabo SJ (2011) Indicadores de actividad y casuística. Madrid: Escuela Nacional de Sanidad.
- Rahimi H, Khammar-Nia M, Kavosi Z, Eslahi M (2014) Indicators of hospital performance evaluation: A systematic review. International Journal of Hospital Research 3(4): 199-208.
© 2022 Elisa López-Dolado. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






