- Submissions

Full Text
Orthopedic Research Online Journal
Radiological and Functional Outcome of Dorsolumbar Burst Fractures Treated with Short Transpedicular Screw Fixation and Facetal Fusion
Muhammad Naeem Shah*
Consultant Orthopedic Surgeon, Khyber Medical University, Pakistan
*Corresponding author: Muhammad Naeem Shah, Consultant Orthopedic Surgeon, Khyber Medical University, Pakistan
Submission: March 23, 2022;Published: April 28, 2022

ISSN: 2576-8875 Volume9 Issue4
Abstract
Objectives: To analyse the radiological and functional outcome in patients with dorsolumbar burst fractures treated with short dorsal instrumentation and facetal fusion.
Material and Methods:51 patients (40 males and 11 female) admitted in Hayatabad medical complex hospital and DHQ hospital Timergara, with dorsolumbar burst fracture. All the patients were treated with transpedicular screw fixation plus facet involve were fused. Posterior decompression performed if neurological deficit present. Patients were followed up and assessed for functional outcome with denis pain pain scale and denis work scale, neurological outcome by ASIA scale and radiological outcome by anterior wedge angle, anterior height, posterior height, kyphotic angle.
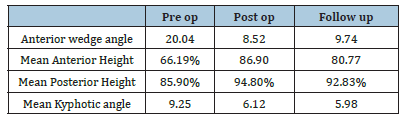
Results: 51 patients (40 males, 11 female) with history of fall from height (89%) and RTA (11%)with (unstable burst fractures). 58.1% of patients were 20-40 years old. On follow up 8 patients improved from ASIA B to ASIA C and 4 patients from ASIA C to ASIA D. among 51 cases, mean Anterior Wedge Angle (AWA) was 20.04° preoperatively which was corrected to 8.52° and on follow up, mean AWA was 9.74°. Mean Anterior Height (AH) was 66.19% preoperatively which was improved to 86.56% and on follow up, mean Anterior Height was 80.77%. Mean Posterior Height (PH) was 85.90% preoperatively which was improved to 94.80% and on follow up, mean Posterior Height was 92.83%. Mean Kyphotic angle was 9.25° preoperatively which was corrected to 6.12° and on follow up, mean Kyphotic angle was 5.98°.
Conclusion: Burst fractures treated with dorsal instrumentation and transpedicular bone grafting facilitate early mobilisation of patients and achieving stable, pain free spinal column and preventing the late vertebral collapse.
Keywords:Burst fractures; Transpedicular screw fixation; Thoracolumbar fracture
Introduction
Doubts still exist about the optimal management strategy for thoracolumbar/lumbar burst fracture [1]. Patients with neurologic deficits or in those with severe instability are generally dealt with surgical treatment. Commonly used procedure is posterior short segment pedicle screw for the treatment of unstable thoracolumbar/lumbar burst fracture. Posterior instrumentation can be divided into long-segment fixation ( two upper and two lower adjacent levels), short-segment fixation (one level above and one below the fractured vertabra) and mono-segment fixation. A large number of biomechanical studies suggest that reinforcement with a fracture-level screw combination can help to improve the biomechanical stability [2] . Short-segment fixation offers the advantage of saving motion segments when compared with longer instrumentations.
Aim of Treatment for thoracolumbar burst fractures include achievement of stability and alignment, deformity correction and decompression of the spinal canal. Posterior short segment pedicle screw fixation with pedicle screw at the fractured vertebra was used . Although the early clinical data from surgery is satisfactory but progressive kyphosis and a high failure rate of the pedicle screws remain a question of this procedure. Anterior column support by anterior approach has its own risks and complications. Transpedicular bone grafting has been used to overcome this failure and in means of biological support in addition to fractured vertebra fixation in preventing loss of kyphosis correction [3,4].
Materials and Method
51 patients (40 males and 11 female) admitted in Hayatabad medical complex hospital and DHQ hospital Timergara, with dorsolumbar burst fracture. ATLS protocol was used to examine the patients, then detailed history of injury, the mode of injury, a thorough clinical and neurological examination.
Rest of skeletal system was examined to rule out any associated injuries. The patient’s spine was examined for any swelling, contusion, tenderness, haematoma, gibbus or step off. Neurological examination (sensation, motor, anal tone) was performed and documented. Spinal column was given immediate protection. Neurological examination was repeated daily . level and severity of neurological injury were noted and Frankel’s Classification was applied if neurological injury present. Under the effect of general anaesthesia, patients were positioned on the fracture table and antero-posterior & lateral X rays were obtained to determine the exact course of pedicles, end plates , disc spaces and the level of injury.
All the patients were treated with transpedicular screw fixation plus facet involve were fused through posterior approach. If neurological deficit present, decompression performed. Patients were followed and assessed for functional outcome with denis pain pain scale and denis work scale, neurological outcome by ASIA scale and radiological outcome by anterior wedge angle, anterior height, posterior height, kyphotic angle.
Results
In our study of 51 patients [78.43% males and 11 female (21.5%)] with a mean age of 32 years with highest number of patients were seen in 20-40 years (57.1%). Among 51 patients, D11 level involved in 6 (11.6%) patient, D12 level in 12 (12.12%) patients, L1 level in 18(35.2%) patients, L2 level in 10 (19.6%) patients and L3 in 4 (7.8%) patients.
In our study, 16 patients (76.1%) had score of 5, one patient (4.7%) had score 6, two patients(9.6%) had score of 7 and two patients (9.6%) had score of 8.Among 51 patients, 38 patients (76%) had history of fall from height and 12 patients (24%) had history of road traffic accident. In our study, 48 patients (85.7%) had Denis pain scale of P 1 and three patients (14.3%) had Denis pain scale of P 2.
Among the 51 patients, 18 patients (35.29%) had neurological deficit of which six case ASIA C grade, 10 cases ASIA B grade and two case ASIA A grade and 33 patients (64.70%) presents without neurological deficit. nine patients improved from ASIA B grade to ASIA C grade, six patients improved from ASIA C grade to ASIA D grade on assessment at 3rd month. None of the patients had detoriation or new onset of neurological deficit.
In our study , among 51 cases, mean Anterior Wegde Angle was 20.04° preoperatively which was corrected to 8.52° and on follow up, mean AWA was 9.74°. Mean Anterior Height (AH) was 66.19% preoperatively which was improved to 86.56% and on follow up, mean Anterior Height was 80.77%. Mean Posterior Height (PH) was 85.90% preoperatively which was improved to 94.80% and on follow up, mean Posterior Height was 92.83%. Mean Kyphotic angle was 9.25° preoperatively which was corrected to 6.12° and on follow up, mean Kyphotic angle was 5.98° as shown in Table 1.
Table 1:
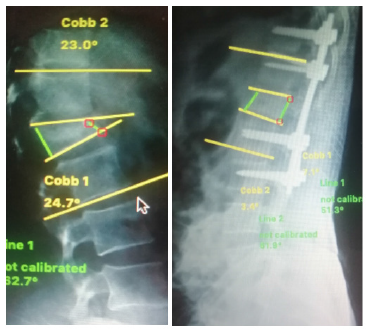
In our study, two patient (4.7%) had superficial wound infection which was treated with antibiotics and dressing. Among the patients with neurological deficit, no patient had bed sore. 49 patients (96.07%) had no complications (Figure 1).
Figure 1: Pre op and post op x-rays.
Discussion
The transitional anatomy of the dorsolumbar spine put it at risk of injury to high-energy deceleration trauma associated with falls and motor-vehicle accidents. The main objectives of initial evaluation include identification of any neurological deficit and avoidance of any exaggeration of cord injury. The aims of the treatment are to achieve pain free stable spine and restoration of maximum function.
The thoracolumbar junction (T11–L2) is the transitional zone between the stiff thoracic and the mobile lumbar spine; therefore, burst fractures in this region are usually very unstable and aggravation of kyphotic deformity after conservative managements is a frequently observed [3,5]. Selection of the surgical approach and method, such as corpectomy and reconstruction via an anterior approach, posterior instrumentation, or combined with an anterior and posterior approach, remains controversial [4,6]. Currently, Posterior Short Segment Pedicle Screw Fixation is a popular procedure for treating unstable thoracolumbar/lumbar burst fracture. But progressive kyphosis and a high rate of hardware failure because of lack of the anterior column support remains a concern. The efficacy of different methods remains debatable and each technique has its advantages and disadvantages [7].
The management of traumatic fractures of the thoracic and lumbar spine remains controversial. A large number of publications, describing various surgical techniques for the reduction and fixation of spinal fractures, followed by discussions among the authors has not led to a general consensus on the optimal treatment [2,5]. Various methods of posterior fixation e.g., hook and Harrington rods have evolved over the past few decades. However, pedicle screw instrumentation has revolutionized spine.
Mentioned that short segment instrumentation has the benefit of incorporating fewer motion segments and biomechanical studies have shown that transpedicular screws are more rigid than posterior distraction instrumentations like Harrington rods [8].
In our series all patients underwent posterior short segment fixation and transpedicular bone grafting using autograft. Ligamentotaxis done in all burst fractures with intact neurology in 51 cases utilizing the partially intact Posterior Ligamentous Complex (PLC). Patients with neurological deficit posterior decompression was done. In our study we have not encountered loss of kyphosis correction for any of our cases and vertebral body height was maintained post operatively even after 18 months of follow up what was achieved on table.
Leferink et al. [9] in his study mentioned that preoperatively the mean Anterior Wedge Angle (AWA) was 16.2° that was corrected to 7.2° and on follow up, mean AWA was 8.5°. Wang et al. [7] in his study observed that mean AWA was corrected to 6.4° and maintained on follow up9. In our study, among 21 cases, mean Anterior Wedge Angle (AWA) was 18.04° preoperatively which was corrected to 9.42° and on follow up mean AWA was 10.14° [9].
Mean Anterior Height (AH) was 68.09% preoperatively which was improved to 83.66% and on follow up, mean Anterior Height was 78.57%. Mean Posterior Height (PH) was 83.90% preoperatively which was improved to 93.80% and on follow up, mean Posterior Height was 92.33%.
Herck et al. [10] in his study noted that mean kyphotic Angle preoperatively was 7° which was corrected to 5° and on 2 years follow up, mean kyphotic angle lost by 1° [10]. In our study mean Kyphotic angle was 8.85° preoperatively which was corrected to 5.42° and on follow up lost by 1° (mean 0.96°).
Conclusion
In conclusion, follow-up results suggest an excellent outcome for short-segment instrumentation. By performing the transpedicular screw fixation with short segment fixation in cases of traumatic thoracolumbar fractures of an unstable nature, a stable fracture fixation can be achieved. Allowing early mobilization ,rapid return to work and costs effective rehabilitation.
References
- Cahueque M , Cobar A , Zuñiga C , Caldera G (2016) Management of burst fractures in the thoracolumbar spine. J Orthop 13(4): 278-281
- Wutte C, Klein B, Becker J, March O, Panzer S, et al. (2019) Early decompression results in better neurological and functional outcome after thoracolumbar spinal cord injury. Jounal of Neurotauma 36: 12.
- Aebi M (2010) Classification of thoracolumbar fractures and dislocations. Eur Spine J 19(suppl.1): 2-7.
- Kim YM, Kim DS, Choi ES, Shon HC, Park KL, et al. (2010) Nonfusion method in thoracolumbar and lumbar spinal fractures. Spine 36(2): 170-176.
- Saglam N, Dogan S, Ozcan C, Turkmen I (2019) Comparison of four different posterior screw fixation techniques for the treatment of thoracolumbar junction fractures. World Neurosurg 123: e773-e780.
- Aly TA (2017) Short segment versus long segment pedicle screws fixation in management of thoracolumbar burst fractures: Meta-analysis. Asian Spine J 11(1): 150-160.
- Cheng LM, Wang JJ, Zeng ZL, Zhu R, Yu Y, et al. (2013) Pedicle screw fixation for traumatic fractures of the thoracic and lumbar spine. Cochrane Database Syst Rev 5: CD009073.
- Jang TA, Kim YE, Moon KY (2013) Comparison of the biomechanical effect of pedicle-based dynamic stabilization: a study using finite element analysis. Spine J (13): 85-94.
- Leferink VJ, Keizer HJ, Oosterhuis JK, van der Sluis CK, et al. (2003) Functional outcome in patients with thoracolumbar burst fractures treated with dorsal instrumentation and transpedicular cancellous bone grafting. Eur Spine J 12: 261-267.
- Bert Van Herck (2009) Transpedicular bone grating as a supplement to posterior pedicle screw instrumentation in thoracolumbar burst fractures. Acta Orthop Belg 75: 815-821.
© 2022 Muhammad Naeem Shah. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






