- Submissions

Full Text
Orthopedic Research Online Journal
Comparison of Posterior Vs Double Approach in the Treatment of Adult Degenerative Scoliosis
Reyes Sánchez Alejandro, García Villaseñor Axel, Galicia Palacios Henar, Domínguez Soto Alejandro, Alpízar Aguirre Armando, Zárate Kalfópulos Barón, Rosales Olivarez Luis Miguel and García Ramos Carla Lisette*
Spine Surgery, National Institute of Rehabilitation, Luis Guillermo Ibarra Ibarra (INR LGII), Secretary of Health (S.S.), Mexico
*Corresponding author: García Ramos Carla Lisette, Spine Surgery, National Institute of Rehabilitation, Luis Guillermo Ibarra Ibarra (INR LGII), Secretary of Health (S.S.), Mexico
Submission: March 02, 2022;Published: April 14, 2022

ISSN: 2576-8875 Volume9 Issue3
Abstract
Background: The prevalence of adult degenerative scoliosis increases with age and can appear in a previously aligned column. Its prevalence is from 2 to 32% in people over 50 years of age.
Material and Methods: a prospective, longitudinal, comparative controlled study with two-year follow-up, in adult degenerative scoliosis, divided into two groups Group I treated with posterior approach and Group 2 treated with the double approach. 43 patients with an average age of 63.2 years, 30 women (69.76%), with curves with magnitude from 10 to 42°. 35 were subjected to a posterior approach, while 8 were treated with a double approach (ALPA Anterior-Lateral-Transpsoas-Approach + posterior approach).
Results: the Roland-Morris scale in group 1 was 13.17 (0-22) and at 2 years 9.75 (0-22) for group 2 with a preoperative mean of 14.71 (8-20) and 7.28 (0-14) at 2 years. No statistical significance between groups (p=0.356). The Oswestry in preoperative group 2 patients was 49.71 (26-74); 2 years in 21.85 (2-44). For group 1 in 54.27 (18-82), and 35.51 (2-82) in 2 years. pelvic parameters have no difference and only correction of scoliosis and sagittal balance was better in the double-approach group.
Conclusion: The meta-analysis revealed that CR MB and PS MB could achieve similar clinical outcomes, whereas the rate of complications and revision was significantly increased in CR MB. Based on the outcomes of this meta-analysis, the choice of the CR MB does not appear to be justified, and further studies of high methodological quality with long-term follow-up are required to confirm our conclusion.
Keywords: Degenerative scoliosis; Double lumbar approach; Posterior lumbar approach
Introduction
World literature has identified that the prevalence of scoliosis increases with age and those anomalous curvatures may appear in a previously aligned spine [1-3], unlike idiopathic scoliosis in young people, it presents with pain and disability in adults [4].
Currently, the prevalence in the population is about 2 to 32% reported in those over 50 years of age and up to 60% in those over 60 years of age [5,6]. Given that its main symptom is pain, this condition has an impact on the quality of life of those who suffer it, limiting their personal and work activities, becoming disabling. It is most frequently observed in adult patients of productive age, progressing with disability [7].
Previous studies have shown that scoliotic curvature correction is over 70% with a double approach vs. 44% with a posterior approach [8]. Controversy exists regarding lordosis, complications, pseudoarthrosis, and complication rate [9-15].
This research proposes to carry out a comparative study between the clinical, radiological, and functional results of two surgical techniques and their variants, as well as to establish if there is correspondence between the radiographic changes and the clinical situation of the patient.
The number of studies comparing the posterior approach with a dual approach for the management of adult degenerative scoliosis is minimal. When searching with the terms: “surgery” + “treatment” + “degenerative scoliosis” + “double approach” search in PubMed, Google Scholar, Ovid, Cochrane we obtained a total of 11 articles [16-27], however, when we searched the Mexican literature, we did not find any reference to the subject. Therefore, we conclude that there is no precedent where the results of double surgical treatment in patients with this disease are analyzed in our country.
The hypothesis is that the dual approach (ALPA Anterior-Lateral- Transpsoas-Approach [22] + posterior) has better radiographic, clinical, and functional results than a posterior approach in the treatment of adult degenerative scoliosis. This study was done to compare the clinical, radiographic, and functional results between patients who underwent double approach vs. patients who underwent posterior approach in the treatment of adult degenerative scoliosis. The specific objectives were to describe the distribution and demographic profile of patients with adult degenerative scoliosis managed in the spine surgery service of our institution, to establish the functional status and pain perception in the two groups of patients before, after, and two years after surgery. Using the SF-36, Roland-Morris scales, the Oswestry disability index, and the Visual Analog Scale, analyze the measurements of pelvic parameters preoperatively, postoperatively, and at the end of follow-up in both groups, compare the correction values of scoliosis and lordosis deformity in the two groups of patients, and contrast the immediate and mediate transoperative and postoperative complications of the patients in both groups.
Materials and Method
It is a prospective study, longitudinal and deliberate intervention, controlled comparative, by direct assignment unblinded beforeand- after panel study with two-year follow-up.
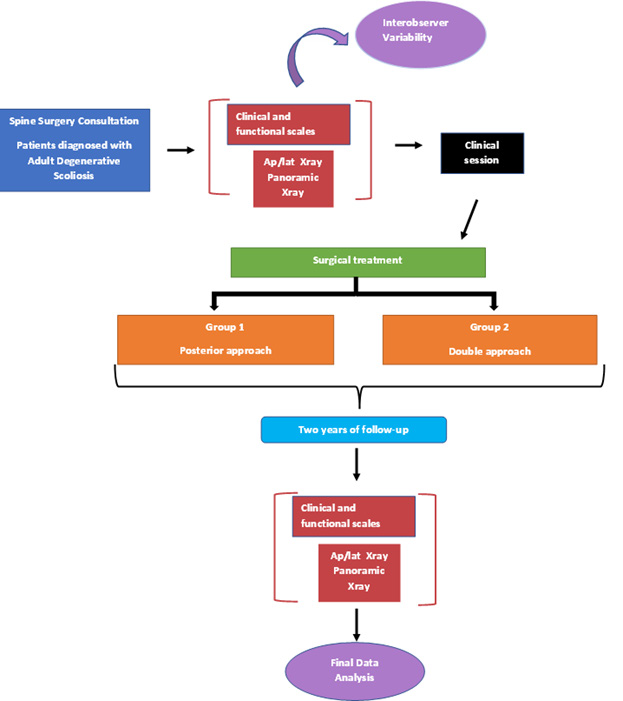
In patients with a diagnosis of adult degenerative scoliosis, with ICD 10 diagnoses of scoliosis, degenerative scoliosis, and adult degenerative scoliosis (the database was obtained from the National Rehabilitation Institute (INR) technological development department), who were treated by conservative management for three months, and subsequently in the INR spine surgery service, by surgical management, posterior approach and double approach, with BMI less than 30, without immune diseases. The included patients were assigned treatment according to the algorithm shown in Figure 1.
Figure 1: The process of patient selection through the clinical session is shown. Description of intervention maneuvers and analysis of results.
The posterior approach consisted of positioning the patient in the prone position, incising the skin in the midline. The posterior bony elements (spinous processes, laminae, pedicles, and transverse processes) are dissected subperiosteally at the levels to be treated. Once exposed, decompression of the roots, osteotomies, transforaminal inter somatic fixation for recovery of the space between the vertebral bodies, and/or posterior fixation with transpedicular screws and rods can be performed, depending on the objective to be achieved with the surgery. Finally, a drain is placed, and the fascia, subcutaneous cellular tissue, and skin are sutured.
To perform the combined ALPA (Antero Lateral transPsoas Approach) plus posterior approach, the patient is placed in right lateral decubitus. A lateral oblique approach is performed. Below the skin and abdominal fasciae are the external and internal oblique muscles and the transverse abdominis muscle, which are bluntly dissected. The transverse fascia is the deepest layer before reaching the retroperitoneum. Digital dissection is performed through this space until the psoas is visualized. The contents of the abdomen and retroperitoneum are protected with an abdominal retractor. The psoas is incised and under fluoroscopic control, the disc to be treated is marked with a needle. The psoas is dissected, and access is gained through it. Lateral resection of the annulus fibrosus is performed and partial discectomy is performed, the inferior platform of the superior vertebra and the superior platform of the inferior vertebra are prepared using dilators, shavers, curettes, and gouges. The contralateral annulus fibrosus is released with a Cobb elevator, avoiding reaching the contralateral psoas.
Subsequently, boxes are placed in the inter somatic spaces where balance is to be restored. The muscles, fascia, and skin are sutured. After this, either in the same surgical time or in a second intervention, a posterior approach is performed, as previously described for decompression and fixation of the treated levels.
Clinical and demographic data are described with summary measures, (mean and median) for quantitative data and dispersion (standard deviation, maxima, and minima). The kappa coefficient was used to measure interobserver agreement.
The normality of the data was analyzed with the Shapiro-Wilk test. Kruskal-Wallis was applied to compare quantitative variables between groups. Pearson’s χ2 test was used to compare qualitative variables.
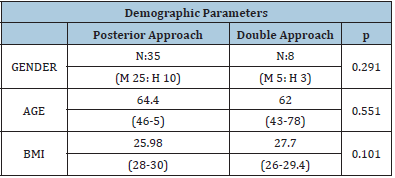
The SPSS V21 statistical package was used, and a significant difference was considered with an α=0.05. Sixty-four patients with adult degenerative scoliosis, operated from 1995 to 2015, by 4 different surgeons were analyzed. However, 5 patients died, 15 refused to participate in the research, 1 patient presented idiopathic scoliosis. Therefore, 43 patients met the inclusion criteria, 30 women (69.76%) and 13 men (30.23%), with an age of 43-78 years (mean 63.2 years) and with curves with magnitude from 10 to 42°, (mean 22.45°). 35 underwent a posterior approach, while 8 were treated with a double approach (ALPA + posterior), the groups being homogeneous (p=0.291). The posterior approach group was composed of 25 women and 10 men, while the combined approach group was composed of 5 women and 3 men. The mean age was 64.4 years (46-75) and 62.0 years (43-78) for the posterior and combined approach, respectively (p=0.551). The mean body mass index in the first group was 25.98 (18-30), in the second group 27.7 (26-29.4) (p=0.101) (Table 1).
Table 1: Demographic variables in both surgical approaches.
Results
It was found that the mean preoperative low back pain, measured according to VAS, in the group treated with a single approach was 7.62 (1-10), while the pain in the extremities was 6.55 (0-10). Postoperatively, low back pain for this group decreased to 2.34 (0- 9) and at 2 years it was 3.37 (0-9), while pain in the extremities decreased postoperatively to 2.72 (0-7) and at 2 years it was 3.44 (0-8). In the double approach group, the mean preoperative pain was 7.42 (6-8) and 6.28 (2-9) for low back pain and radicular pain, respectively. Postoperatively the VAS for low back pain decreased to 1.0 (0-3) and at 2 years was 2.85 (0-6), while the VAS reported for radicular pain postoperatively was 2.28 (0-7) and at 2 years was 2.71 (0-7). The difference in terms of improvement in low back pain and radicular pain, between the two groups, postoperatively and at 2 years, was not statistically significant. (p=0.118, p=0.613), (p=0.591, p=0.495).
Regarding the Roland-Morris low back pain scale, the mean preoperative value for the group treated with posterior approach was 13.17 (0-22), and at 2 years postoperatively it was 9.75 (0- 22). In the group treated with the double approach this was 14.71 (8-20) preoperatively and 7.28 (0-14) at 2 years. At 2 years after surgery, there was no statistical significance between the groups (p=0.356).
The mean Oswestry Disability Index in patients treated with a single approach was 54.27 (18-82), decreasing to 35.51 (2-82) at 2 years post-surgery. In those treated with a double approach the preoperative ODI was 49.71 (26-74); 2 years after surgery it was reported at 21.85(2-44). The improvement in ODI was not statistically significant (p=0.074) (Table 2).
Taking into consideration the SF-36 questionnaire, the items of physical and mental health (PCS and MCS) were analyzed separately. In the group treated with a single approach, the mean preoperative PCS and MCS were 19.41 (13.8-28.7) and 40.56 (25.9- 52.2) respectively. At 2 years a slight increase in their values was found, 31.08(17.2-47) for PCS and 45.13(22.1-69.8) for MCS. On the other hand, in the dual approach group, preoperative PCS and MCS mean values were 22.7 (17.8-31.3) and 41.25(30.1-50.9). In the following 2 years, their values were 37.25(26-52.3) and 54.98(42.5- 65.4), respectively. There was no significant difference between the two approaches if we refer to the PCS (p=0.120); however, it is found that there is statistical significance in the postoperative MCS between the two groups (p=0.050).
Table 2: Comparison between clinical parameters referring to VAS and clinical scales in the preoperative, postoperative, and 2-year follow-up periods.

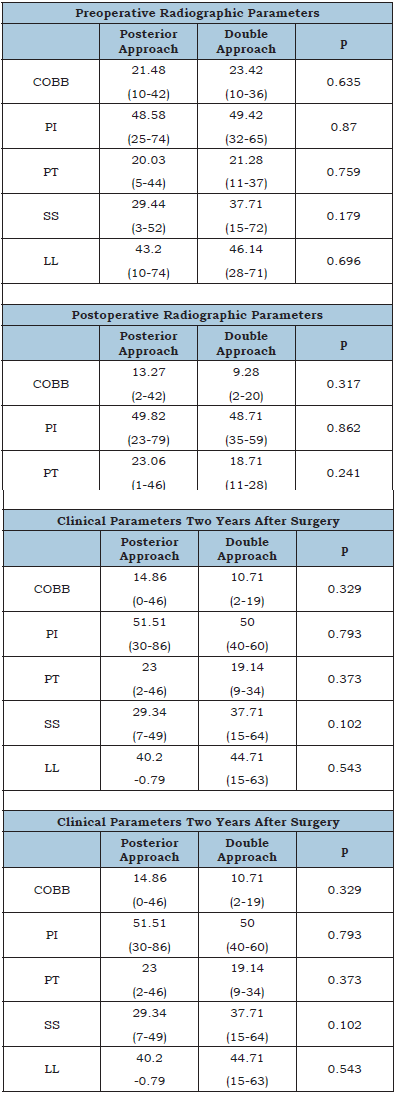
We found the preoperative curve magnitude in patients who underwent posterior approach to average 21.48° (10-42), which decreased postoperatively to 13.27° (2-42), and at 2 years remained at 14.86° (0-46). Meanwhile, in patients treated with ALPA + posterior, the average magnitude of the curve was 23.42° (10-36), which improved to 9.28° (2-20) and slightly increased at 2 years to 10.71° (2-19). The improvement in curve magnitude was not significant postoperatively (p=0.317), nor at 2-year follow-up (p=.329), between groups.
In the individuals in whom the posterior approach was performed, the average preoperative lumbar lordosis was 43.2° (10-74). Postoperatively it was 39.00° (5-69), and at 2 years of follow-up 40.2° (0-79). In those who underwent the double approach, the mean preoperative lumbar lordosis was 46.14° (28- 71), while postoperatively and at 2 years after surgery, it was 43.0° (28-61) and 44.71° (15-63), respectively. There was no statistical significance in the correction of lumbar lordosis between the two approaches postoperatively (p=0.531), or at 2 years postoperatively (p=0.543).
Analyzing the pelvic parameters in both groups, posterior and ALPA + posterior; we found that the pelvic incidence in the first group had an average of 48.58° (25-74) preoperatively, remained at 49.82° (23-79) postoperatively, and increased at 2 years after surgery to 51.51° (30-86). In the second group, the preoperative average was 49.42° (32-65), 48.71° (35-59) and at 2 years it was 50.0° (40-60). The pelvic angle in the first group had a mean of 20.03° (5-44) preoperatively, after surgery it was 23.06° (1-46), remaining at 2 years at 23.0° (2-46). In the combined approach the preoperative mean in this parameter was 21.28° (11-37), after surgery it was 18.71° (11-28) and during the 2-year follow-up, it was 19.14° (9-34). Finally, the sacral slope before surgery, for the first group, was on average 29.44° (3-52), postoperatively 27.68° (3-49), and 2 years after surgery 29.34° (7-49). Meanwhile, in the second group the preoperative sacral slope averaged 37.7° (15-72), postoperatively 37.28° (17-57), and 37.71° (15-64) in the subsequent 2 years. There was no evidence of significance between PI (p=0.862 and p=0.793), PT (p=0.241 and p=0.373), or SS (p=0.084 and p=0.102) postoperatively or at 2-year follow-up, among patients treated with the different approaches (Table 3).
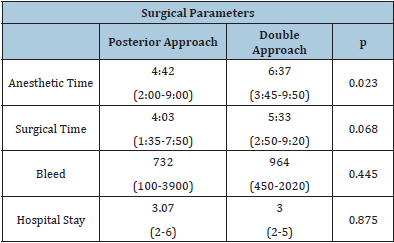
The average time in which the posterior approach was performed was 4:03 hours (1:35-7:50). Compared to the time used for ALPA + posterior, which was 5:33 hours (2:50-9:20), we observed that there is a difference between the two, however, it is not statistically significant (p=0.068).
The anesthetic time in the single approach group averaged 4:42 hours (2:00-9:00). In contrast, in the combined approach group it was 6:37 hours (3:45-9:50), the statistical difference being significant (p=0.023).
The mean bleeding rate of patients who underwent a single approach was 732ml (100-3900); whereas in patients treated with a double approach, it was 964ml (450-2020) (p=0.445).
3.07 days (2-6) was the average hospital stay for those treated with a single approach, an item that did not differ from the group treated with a double approach, whose hospital stay was 3.0 days (2-5) (p=0.871) (Table 4).
Table 3: Comparison between radiographic parameters at preoperative, postoperative, and 2-year follow-up.
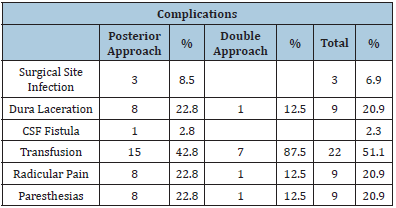
In the isolated posterior approach group, there were 8 patients with lacerations of the dura mater (22.8%), which were repaired on the spot. One of the patients in this group developed a cerebrospinal fluid fistula (2.8%), which required reoperation to close the defect in the dura. 15 patients had excessive bleeding requiring transfusion (42.8%). 3 patients (8.5%) suffered an infection in the instrumentation, so the fixation material had to be removed, one of them during the first month after surgery, so it was managed with a bandage for 1 year until consolidation was achieved. In one of the patients who was treated with a posterior approach, the procedure was performed 2 surgical times, with a space of 5 months between one and the other. This was due to a layer hemorrhage during the first surgical time. The patient was transfused, discharged, and rescheduled for a second surgical time, to complete the instrumentation. 8 patients (22.8%) suffered radicular pain and numbness of the extremities.
Table 4: Comparison between surgical parameters and hospitalization time.
In contrast, in the group treated with a double approach, one patient presented a laceration of the dura mater (12.5%), which was repaired at the time. Seven patients (87.5%) presented excessive bleeding and required transfusion. There were no reports of infections among the dual approach group. One patient (12.5%) continued with radicular pain and numbness of the extremities.
Discussion
The mean age of presentation of degenerative scoliosis in our population is 63.2±9.6 years and the gender distribution is 69.7% in women and 30.23% in men. This is similar to that described by Anwar et al. [28] who reported age of 63.25±15.3 years and that 70.3% were women, and Pérennou et al. [2] who reported a mean age of 62.1±12 years and that 72% were female, with a female-tomale ratio of 2/1.
The perception of preoperative low back pain using VAS was 7.62±1.76, decreasing to 2.34±2.1 postoperatively and 3.37±2.27 at 2 years in the patients treated with a posterior approach and was 7.42±0.78 in the group treated with a combined approach, decreasing to 1±1.29 postoperatively and 2.85±2.84 at 2 years. In his study, Tormenti [25] documented a preoperative VAS of 9.5 and postoperative VAS of 4 in patients treated with a posterior approach versus 8.8 in preoperative VAS and 3.5 in postoperative VAS in the double approach, without finding a significant difference between the two groups, which is similar to our results. Something similar was found by Hsieh et al. [16], in a retrospective study with 110 patients, made a comparison between a posterior approach (54 patients) and a double approach (ALIF + posterior) (56 patients, 18 at one time and 38 at two surgical times). They established a mean preoperative VAS in the posterior approach of 9.0 and 2.3 2 years after surgery; in the dual approach, the mean preoperative VAS was 8.2, decreasing to 2.1 at 2 years of follow-up. There was no statistical significance preoperatively (p=0.54) or postoperatively (p=0.23).
Regarding the perception of lower extremity pain, we found that preoperatively the VAS was 6.55±2.82, 2.72±1.88 postoperatively, and 2.63±2.01 at 2 years in patients treated with a posterior approach, while in those treated with a combined approach it was 6.28±2.69 preoperatively, 2.28±2.62 postoperatively and 2.71±2.56 at 2 years. In the study performed by Hsieh et al. [16], a mean preoperative VAS in the posterior approach was found to be 6.5. Two years after surgery the VAS was 0.5. In the combined approach the mean preoperative VAS was 5.5, improving to 0.9 at the end of follow-up. In our study, there was no statistical significance between groups pre-and postoperatively (p=0.45 and p=0.22, respectively). We found patients in whom lumbar pain was present without reporting any type of pain in the lower extremities, so we agree with what has been described in terms of degenerative scoliosis is not accompanied by stenosis in all cases [9].
Using the Roland-Morris scale for low back pain perception we found that in patients treated with a posterior approach preoperatively the score was 13.47±7.06 and at 2 years 9.75±6.24, while in patients treated with a combined approach it was 14.71±4.07 preoperatively and 7.28±6.42. We did not find any report on the use of the Roland-Morris scale comparing the posterior approach vs. the double approach; however, Faldini [29] conducted a retrospective study, where he analyzed 81 patients with degenerative scoliosis, with an average age of 61 years (range 44-73) undergoing a posterior approach and compared the results of a short fusion (<3 levels) (57 patients) vs a long fusion (≥ 4 levels) (24 patients), and finds in these patients a score on this preoperative scale of 15 points (range 12-19) in the short fusion group and 16 points (range 13-21) in patients undergoing long fusion, decreasing to 4 points (range 2-5) in both groups, at the last follow-up (2-5 years postoperatively); which exceeds that reported for our two groups.
The Oswestry Disability Scale (ODI) in patients treated with a posterior approach was 54.27±16.65 and 35.51±18.23 preoperatively and at 2 years, respectively, with a difference of 18.76 between the two figures. The combined approach group was 49.71±15.8 preoperatively and 22.42±15.25 at 2 years, with a difference of 27.29. Similar to this, Hsieh et al16 found reported in their study a preoperative ODI in the posterior approach group of 29.1, with improvement to 6.2 at 2-year follow-up, with a difference of 22.9. The ODI in the double approach was 28.8, at 2 years after surgery it was 6.4, with a difference of 22.4. There was no significant difference in the ODI between groups. Our study differs from that reported by Good & Lenke [30], who is a retrospective study compared 24 patients treated with posterior approach versus 24 patients treated with double approach (anterior + posterior) and with a follow-up at 2 years. In this study, the pre-surgical ODI in patients who underwent the posterior approach was 32.4, decreasing to 19.7 at 2 years, with a difference in the mean of 13.7 (p=0.002). On the other hand, in patients who underwent double approach, we found a pre-surgical ODI of 33.7, which at 2 years was 21.1, with a change of 12.5 (p=0.017). The comparison between one treatment and the other was not significant preoperatively (p=0.80) or postoperatively (p=0.70). It is worth mentioning that in this study the treated patients did not have degenerative scoliosis “de novo”, they were patients with idiopathic scoliosis, kyphoscoliosis, and congenital scoliosis, which progressed in adulthood.
Table 5: Summary of complications between the two study groups.
In our patients, we found that the SF-36 in the physical health item preoperatively and at 2 years in the postoperative approach group was 19.41±3.91 and 31.08±9.19 respectively, in patients with a combined approach it was 22.7±4.67 before surgery and at 2 years 37.25±9.18. Regarding mental health, we found that in the posterior approach before surgery it was 40.56±6.6 and at 2 years it was 45.13±12.12. In the combined approach we reported that before surgery it was 41.25±7.25 and at 2 years it was 54.98±7.84. We found no studies reporting SF-36 in comparison between approaches. Zimmerman et al. [31] performed a prospective study with 35 patients, older than 40 years, with adult degenerative scoliosis, treated surgically and with a minimum follow-up of 2 years, without previous surgeries. They did not make the comparison between approaches, but involved patients treated with only posterior approach (16 patients), anterior + posterior on the same day (5 patients), anterior + posterior in 2 stages (14 patients). They evaluated clinical outcomes using the SF-36 preoperatively and postoperatively, reporting mean preoperative PCS of 53.1±22.8 and postoperative PCS of 75.6±27.1, with a mean improvement of 20.6±16.7. The mean preoperative MCS was 75.4±19.7 and the postoperative MCS was 81.3±23.8, with a mean increase of 3.1±9.1, which is not comparable with our results (Table 5).
The magnitude of the curve in the group treated with the posterior approach was 21.48±9.6°, with a correction at 2 years to 14.86±10.52°, giving a mean correction of 37.89% with this approach, while in the group treated with the combined approach the magnitude of the curve was 23.42±9.8°, with a correction at the end of the follow-up to 10.71±6.7°, with a mean correction of 51.47%. This correction is below that mentioned by Tormenti [25] who reports a curvature correction in patients treated with a combined approach from a mean of 38.5° to a mean of 10°, with a mean percentage correction of 70.2%, and in patients treated with a posterior approach reports a curve correction from a mean of 19° preoperatively to 11° postoperatively, with a mean percentage correction of 44.7%. Our results do not compare with those of Hsieh et al16, who documented a curve correction of 38.5° to 21.4° (44%) in patients treated with a posterior approach and a correction of 48.3° to 9.3° (78%) in patients with a double approach, with no significant preoperative difference (p=0.48), but with a significant postoperative difference (p=0.02) between both groups. Similarly, they contrast with the results of Pateder [26] who reports a scoliotic curve correction of 54% (mean 47.2° preoperatively to 25.5° postoperatively) with a posterior approach versus 46% (mean 54.9° preoperatively to 25.7° postoperatively) with a combined anterior + posterior approach. Good & Lenke [30] report a mean scoliotic curvature in patients with thoracolumbar/ lumbar curvature of 58° and 60°, in 2 groups treated with a posterior and a combined approach, achieving a correction of 55% and 43%, respectively, which was significant in their study (p=0.03). Khan27 in a study of 14 patients treated with a double approach reports a correction of the curve with a mean of 46° preoperatively to 6° at the end of follow-up but does not make a comparison with other approaches.
Lumbar lordosis and pelvic parameters were generally not affected by treatment in either group. LL in the posterior approach treated group was 43.2±17.95 preoperatively and at 2 years was 40.20±17.84, while in the dual approach group preoperatively was 46.14±16.25 and post 2 years it was 44.71±15.37. Tormenti [25] reports something similar, finding no changes in lumbar lordosis between patients submitted to a posterior approach and a double approach (LL 47.3±28.7° pre and post 40.4±2.8°, in the combined approach vs. 30±10.5° pre and post 37.7±3.5°, in the posterior approach), thus preserving the LL and its hypo- or hyperlordotic curves. The results of Hsieh16 record an LL correction of 6° to 15.8° in the posterior approach group and 3.1° to 35.7° in the double approach group, which leads us to believe that most or all patients have hypo- or hyperlordotic spines. The magnitude of the correction is statistically significant between groups (p=0.009). Pateder26 reports a correction of lumbar lordosis in patients undergoing a posterior approach of 10.2° (27° pre to 37.2° post) and 8.5° (25.4° pre to 33.9° post) in the combined approach, which turns out not to be significant. In his study, Khan [27] reports an increase in lumbar lordosis in patients treated with a double approach, with a mean of 35° preoperatively and a mean of 55° at the end of follow-up (mean 21 months postoperative).
No studies were found where the pre and postoperative pelvic parameters were analyzed in comparisons of the results of surgical approaches in the treatment of adult scoliosis. Surgical times averaged 4:03±1:43 hours and the time from induction of anesthesia to patient recovery inside the operating room was 4:42±1:45 hours for the posterior approach, versus 5:33±2:28 hours of surgical time and 6:37±2:29 hours of anesthetic time for the double approach. Reported bleeding was 732.75±748.60ml for the posterior approach and 964.28±505.36ml for the combined approach. Hospital stay for the posterior approach was 3±0.99 days versus 3±1 days for the dual approach.
The results of other studies [32,33], in this aspect, are twice as long as ours, for example, Good & Lenke [30] reported that the surgical time was 11.6 hours for the double approach group, while it was 6.9 hours for the posterior approach group, which was significant (p<0.0001). Estimated bleeding was 1330ml for the first group, versus 980ml for the second group, also being statistically significant (p=0.04). Hospital stay was 11.9 and 8.3 days for the combined and posterior approaches, respectively (p=0.03). Hsieh et al16 documented that the mean operative times were 172.5 minutes for ALIF and 262.5 minutes for posterior instrumentation in the dual approach group, compared to 350.5 minutes for the posterior approach group. The mean estimated bleeding was 250ml in the ALIF and 1650ml in the posterior instrumentation in the double approach group. In the posterior approach, the mean was 3250ml. Hospital stay was 16 days and 10 days for the combined and posterior approaches, respectively. Although it is not within the objectives of our study to analyze the number of instrumented levels, we can establish that the difference in surgical times, bleeding, and days of hospital stay is due to the extent of the instrumentations.
Complications in the surgical treatment of scoliosis are reported to be 20-40% [6,19]. In our study no major systemic complications such as myocardial infarction, ileus, pneumonia, deep vein thrombosis, pulmonary thromboembolism, urinary tract infections, mesenteric artery syndrome, or blindness were found. No surgical site infection was reported in patients treated with a double approach. The percentage of dura tears was 12.5%. The percentage of patients with persistent radicular pain was 12.5%, which is similar to the 12% reported by Ailon T [34], 12.5% by Tormenti [25], and 10.7% by Hsieh [16]. Among the complications in patients treated only with the posterior approach, 3 surgical site infections were found (8.5%), which is above the infection rate reported by Smith et al. [35], the rate is 3.5%; Tambe [10], who refers that the rate ranges from 3 to 5% [11] and Bradford [14], who argues that it ranges from 1 to 8%. The dura mater tears in this group were 22.8%, in agreement with the literature [4].
Conclusion
The ALPA + posterior approaches, compared to the posterior approach alone, have an advantage in reducing the magnitude of scoliosis and restoring sagittal balance. Both approaches were shown to be equally effective in terms of quality of life and pain perception. It was observed that the hospitalization time in the two approaches is similar. The limitations of this study are that the sample of patients treated with a dual approach is small. In addition, the number of levels involved in instrumentation is not taken into account in the analysis.
References
- Robin GC, Span Y, Steinberg R, Makin M, Menczel J (1982) Scoliosis in the elderly: a follow-up study. Spine 7: 355-359.
- Perennou D, Marcelli C, Herisson C, Simon L (1994) Adult lumbar scoliosis. Epidemiologic aspects in a low-back pain population. Spine 19: 123-128.
- Li G, Passias P, Kozanek M, Fu E, Wang S, et al. (2009) Adult scoliosis in patients over 65 years of age. Spine 34(20): 2165-2170.
- Smith JS, Shaffrey CI, Berven S, Glassman S, Hamill C, et al. (2009) Operative versus nonoperative treatment of leg pain in adults with scoliosis. A retrospective review of a prospective multicenter database with two-year follow-up. Spine 34(16): 1693-1698.
- Youssef JA, Orndorff DO, Patty CA, Scott MA, Price HL, et al. (2013) Current status of adult spinal deformity. Global Spine J 3: 51-62.
- Kotwal S, Pumberger M, Hughes A, Girardi F (2011) Degenerative scoliosis: A review. HSS J 7: 257-264.
- Ploumis A, Transfledt EE, Denis F (2007) Degenerative lumbar scoliosis associated with spinal stenosis. Spine J 7(4): 428-436.
- Kuklo TR (2006) Principles for selecting fusion levels in adult spinal deformity with particular attention to lumbar curves and double major curves. Spine 31(S19): 132-138.
- Le Huec JC, Cogniet A, Mazas S, Faundez A (2016) Lumbar scoliosis associated with spinal stenosis in idiopathic and degenerative cases. Eur J Orthop Surg Traumatol 26(7): 705-712.
- Tambe AD (2011) Adult degenerative scoliosis. Orthop Trauma 25(6): 413-424.
- Aebi M (2005) The adult scoliosis. Eur Spine J 14: 925-948.
- Silva FE, Lenke LG (2010) Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 28(3): 1-10.
- Dakwar E, Cardona RF, Smith DA, Uribe JS (2010) Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus 28(3): E8.
- Bradford DS, Tay BK, Hu SS (1999) Adult scoliosis: surgical indications, operative management, complications, and outcomes. Spine 24(24): 2617-2629.
- Caputo AM, Michael KW, Chapman TM, Massey GM, Howes CR, et al. (2012) Clinical outcomes of extreme lateral interbody fusion in the treatment of adult degenerative scoliosis. Scientific World Journal 2012: 1-5.
- Hsieh MK, Chen LH, Niu CC, Fu TS, Lai PL, et al. (2015) Combined anterior lumbar interbody fusion and instrumented posterolateral fusion for degenerative lumbar scoliosis: indication and surgical outcomes. BMC Surg 15(26): 1-7.
- Fu KM, Rhagavan P, Shaffrey CI, Chernavvsky DR, Smith JS (2011) Prevalence, severity, and impact of foraminal and canal stenosis among adults with degenerative scoliosis. Neurosurgery 69: 1181-1187.
- Voin V, Kirkpatrick C, Alonso F, Rustagi T, Sanders FH, et al. (2017) Lateral transpsoas approach to the lumbar spine and relationship of the ureter: anatomic study with application to minimizing complications. World Neurosurg 104: 674-678.
- Dwyer AF, Newton NC, Sherwood AA (1969) An anterior approach to scoliosis. a preliminary report. Clin Orthop Relat Res 62: 192-202.
- Bhalla A, Fayssoux R, Radcliff KE (2015) Approach options in adult spinal deformity surgery. Semin Spine Surg 27: 163-168.
- Bergey DL, Villavicencio AT, Goldstein T, Regan JJ (2004) Endoscopic lateral transpsoas approach to the lumbar spine. Spine 29(15): 1681-1688.
- Dahdaleh NS, Snyder LA, Smith ZA, Fessler RG, Graham RB, et al. (2014) Lateral transpsoas lumbar interbody fusion: Outcomes and deformity correction. Neurosurg Clin N Am 25: 353-360.
- Graham RB, Liu JC, Wong AP (2014) Minimally invasive lateral transpsoas approach to the lumbar spine: pitfalls and complication avoidance. Neurosurg Clin N Am 25: 219-231.
- Dorward IG, Lenke LG (2010) Osteotomies in the posterior-only treatment of complex adult spinal deformity: a comparative review. Neurosurg Focus 28(3): E4.
- Tormenti MJ, Maserati MB, Bonfield CM, Okonkwo DO, Kanter AM (2010) Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation. Neurosurg Focus 28(3): E7.
- Pateder DB, Kebaish KM, Cascio BM, Neubaeur P, Matusz DM, et al. (2007) Posterior only versus combined anterior and posterior approaches to lumbar scoliosis in adults a radiographic analysis. Spine 32(14): 1551-1554.
- Khan SN, Hofer MA, Gupta MC (2009) Lumbar degenerative scoliosis: outcomes of combined anterior and posterior pelvis surgery with minimum 2-year follow-up. Orthopedics 32(4).
- Anwar Z, Zan E, Gujar SK, Sciubba DM, Riley III LH, et al. (2010) Adult lumbar scoliosis: underreported on lumbar MR scans. Am J Neuroradiol 31: 832-837.
- Faldini C, Di Martino A, Borghi R, Perna F, Toscano A, et al. (2015) Long vs. short fusions for adult lumbar degenerative scoliosis: does balance matters? Eur Spine J 24(S7): S887-S892.
- Good CR, Lenke LG, Bridwell KH, O’Leary PT, Pichelmann MA, et al. (2010) Can posterior-only surgery provide similar radiographic and clinical results as combined anterior (Thoracotomy/Thoracoabdominal)/ posterior approaches for adult scoliosis? Spine 35(2): 210-218.
- Zimmerman RM, Mohamed AS, Skolasky RL, Robinson MD, Kebaish KM (2010) Functional outcomes and complications after primary spinal surgery for scoliosis in adults aged forty years or older. a prospective study with minimum two-year follow-up. Spine 35(20): 1861-1866.
- Cho KJ, Kim YT, Shin S, Suk SI (2014) Surgical treatment of adult degenerative scoliosis. Asian Spine J 8(3): 371-381.
- Tribus CB (2003) Degenerative lumbar scoliosis: Evaluation and management. J Am Acad Orthop Surg 11: 174-183.
- Ailon T, Smith JS, Shaffrey CI, Lenke LG, Harrop JS, et al. (2015) Degenerative spinal deformity. Neurosurgery 77: 75-79.
- Smith JS, Shaffrey CI, Sansur CA, Scoliosis Research Society Morbidity and Mortality Committee, et al. (2011) Rates of infection after spine surgery based on 108,419 procedures: a report from the scoliosis research society morbidity and mortality committee. Spine 36: 556-563.
© 2022 García Ramos Carla Lisette. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






