- Submissions

Full Text
Orthopedic Research Online Journal
How to Manage the Avulsion of a Permanent Tooth : About a Case
Zidane Fatima Ezzahra1* and El Alloussi Mustapha2
1International University of Rabat, College of Health Sciences, International Faculty of Dental Medicine, BioMed Unit Technopolis Parc, Rocade of Rabat-Salé, Sala-Al Jadida, 11100, Morocco
2Professor of Higher Education in Pediatric Dentistry, International University of Rabat, College of Health Sciences, International Faculty of Dental Medicine, Morocco
*Corresponding author: Zidane Fatima Ezzahra, International University of Rabat, College of Health Sciences, International Faculty of Dental Medicine, BioMed Unit Technopolis Parc, Rocade of Rabat-Salé, Sala-Al Jadida, 11100, Morocco
Submission: March 22, 2022;Published: March 31, 2022

ISSN: 2576-8875 Volume9 Issue3
Introduction
Traumatic avulsion of permanent teeth is the most severe form of traumatic dislocation and represents an absolute clinical emergency. Only prompt and adequate treatment can achieve the best possible prognosis. The practitioner must give the appropriate advice: reimplantation or conservation of the tooth in an adequate conservation solution in order to avoid apoptosis of the pulp and periodontal cells [1-3].
This work aimed to describe the management of a case of traumatic avulsion based on the latest recommendations of the IADT (International Association of Dental Traumatology) of 2020 (1).
Case Presentation
A 10-year-old boy in good general health presented to the dental office for expulsion of the 11 as a reason for consultation, dating for more than 12 hours (Figures 1-11).
Figure 1: Absence of 11 + luxation of 21, 22.

Figure 2: Tooth stored in physiological saline.
Figure 3: X-ray showing the empty dental socket.

Figure 4: Reimplantation of 11.

Figure 5: Repositioning of the 21, 22 + splint 13 -23.

Figure 6: Sutures.

Figure 7: Postoperative X-ray.

Figure 8: Control after 2 weeks.
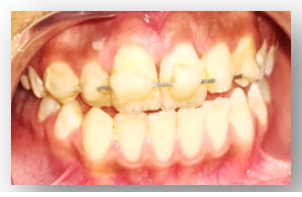
Figure 9: Ca(oh) 2 for 2 weeks.
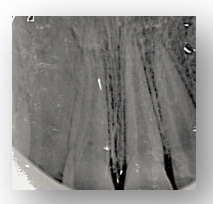
Figure 10: Canal obturation of 11 with gutta percha.

Figure 11: Removal of the splint after 2 weeks.

Discussion
The choice of treatments and the prognosis of the avuled tooth largely depends on the viability of the periodontal ligaments and the maturity of the root, in our case the expulsion was more than 12 hours old on a mature tooth. Thus, our trauma management according to IADT was as follows [4-6]:
A. Remove visible debris by agitating the tooth in physiological storage medium or with saline-soaked gauze.
B. Administer local anesthesia, preferably without a vasoconstrictor.
C. Irrigate the socket with sterile saline
D. Examine the socket cavity. Remove the blood clot if necessary.
E. Reimplant the tooth slowly with light finger pressure.
F. Check the correct position of the reimplanted tooth clinically and radiologically
G. Passive and flexible splint with a wire 0.016 or 0.4mm diameter for 2 weeks (2)
H. Keep the composite and the adhesive system away from the gum and proximal areas
I. Begin root canal treatment within 2 weeks of reimplantation
J. Suture gingival lacerations
K. Administer systemic antibiotics (4,5)
L. Check tetanus status (6)
M. Provide postoperative instructions
a) Avoid participation in contact sports.
b) Maintain a soft diet for up to 2 weeks, according to the tolerance of the patient.
c) Brush their teeth with a soft toothbrush after each meal.
d) Use a chlorhexidine (0.12%) mouth rinse twice a day for 2 weeks
N. Clinical and radiological follow-up at 2 weeks, 4 weeks, 3 months, 6 months, 1 year and every 5 years (7, 8, 9, 10) [7-10]
Conclusion
The treatment philosophy for traumatic avulsion is based on reimplantation as soon as possible in order to prevent complications, and to restore, at least temporarily, esthetics and function by maintaining the contour of the alveolar bone. Therefore, re-implanting a permanent tooth is almost always the right decision even if the extra-oral duration is more than 60 minutes.
References
- Cecilia B, Aristidis A, Asgeir S, Nikolaos K (2022) Dentoalveolar trauma of children and adolescents. Pediatric Dentistry pp. 363-413.
- Kwan SC, Johnson JD, Cohenca N (2012) The effect of splint material and thickness on tooth mobility after extraction and replantation using a human cadaveric model. Dent Traumatol 28(4): 277- 281.
- Ben Hassan MW, Andersson L, Lucas PW (2016) Stiffness characteristics of splints for fixation of traumatized teeth. Dent Traumatol 32(2): 140-145.
- Hammarstrom L, Blomlof L, Feiglin B, Andersson L, Lindskog S (1986) Replantation of teeth and antibiotic treatment. Endod Dent Traumatol 2(2): 51-57.
- Sae-Lim V, Wang CY, Choi GW, Trope M (1998) The effect of systemic tetracycline on resorption of dried replanted dogs' teeth. Endod Dent Traumatol 14(3): 127-132.
- Rhee P, Nunley MK, Demetriades D, Velmahos G, Doucet JJ (2005) Tetanus and trauma: a review and recommendations. J Trauma 58(5): 1082-1088.
- Andreasen JO, Andreasen FM, Avulsions TG Andreasen (2019) In: Andreasen JO, Andreasen FM, Andersson L (Ed.), Textbook and color atlas of traumatic injuries to the teeth. Wiley Blackwell, USA, pp. 486- 520.
- Andreasen JO, Borum MK, Andreasen FM (1995) Replantation of 400 avulsed permanent incisors. 3. Factors related to root growth. Endod Dent Traumatol 11(2): 69-75.
- Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM (1995) Replantation of 400 avulsed permanent incisors. 1. Diagnosis of healing complications. Endod Dent Traumatol 11(2): 51-58.
- Al-Sane M, Bourisly N, Almulla T, Andersson L (2011) Laypeoples' preferred sources of health information on the emergency management of tooth avulsion. Dent Traumatol 27(6): 432-437.
© 2022 Zidane Fatima Ezzahra. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






