- Submissions

Full Text
Orthopedic Research Online Journal
Fibrodysplasia Ossificans Progressiva: A Case Series and Literature Review
Muhammad Naeem Shah1, Muhammad Inam2*, Imran Khan2 and Muhammad Arif3
1Consultant Orthopedic Surgeon, Department of Orthopedic District Headquarter Hospital Temargara Lower Dir, Pakistan
2Department of Orthopedic and Taumatology, Medical Teaching Institute Lady Reading Hopsital Peshawar, Pakistan
3Incharge Orthopeadic unit, Hayatabad Medical Complex Peshawar, Pakistan
*Corresponding author: Muhammad Inam, Department of Orthopedic and Taumatology, Medical Teaching Institute Lady Reading Hopsital Peshawar, Pakistan
Submission: February 25, 2022;Published: March 09, 2022

ISSN: 2576-8875 Volume9 Issue3
Abstract
Fibrodysplasia Ossificans Progressiva(FOP) is a rare autosomal dominant disease, characterized by multiple bony swellings mostly in the axial musculature at shoulder. Diagnosis is based on findings of extra-skeletal ossification in the connective tissues and congenitally malformed big toe. Although the congenitally malformed big toe is present since birth, still its diagnosis is often missed. We report three cases of Fibrodysplasia Ossificans Progressiva. The patients were diagnosed one at 6 years of age, other at 10 years and other at 25 years of age. They had classical features of the disease, congenital hallux valgus deformity of foot and extra skeletal ossification. The objective of reporting these cases is to attract the researcher to do something for its prevention and treatment.
Keywords: Fibrodysplasia ossificans progressive; Hallus valgus; Ossification
Introduction
Fibrodysplasia Ossificans Progressiva is rare congenital disorder which occurs most commonly as result of new mutation [1-5]. It is inherited as autosomal dominant disease [1,2,6,7].This disease is manifested by extra skeletal bone formation in axial musculature, which start developing in first decade of life, apart from this bilateral hallux valgus deformity is present since birth. This disease occurs due to mutation in the FOP gene located on chromosome 4. These results increase in Bone morphogenic Protein 4 (BMP 4) [1,2,8]. This increase in BMP 4 leads to ossification in connective tissues of voluntary muscles, tendons and fascia. Usually, a soft tissue trauma triggers the ossification. Initially painful lumps develops which fades away in a few days but it leads to the formation of new bone at the site of initial trauma. With growing age, ribbons and sheaths of extra skeletal bone is formed which functionally lock the spine to skull, skull to jaw, and spine to limbs. Patient gradually lose mobility [1-4]. Patient become wheelchair bound by 20 years of age, bedridden by 30 years and usually leads to death by 40 years of age. The common mode of death being respiratory compromise [8]. This disease is most often misdiagnosed resulting in iatrogenic insult to the patient [6].
Case Report 1
We report a case of 6 years old female patient who was referred to department of Orthopaedics and spine surgery by the pediatric unit. They referred the patient to orthopaedic unit because they had noticed multiple bony swelling; they had obtained radiographs of the swellings and interpreted them as osteo-cartilaginous exostosis. We admitted the patient and obtained detailed history followed by clinical examination. The patient had bony swellings on the anterior and posterior aspect of her left shoulder and in the buttocks as well. The parents reported that swelling in her buttock appeared around 4 years of age after a ground level fall. They disappeared after a few weeks but were followed by appearance of bony swellings. Two years later the patient also developed similar phenomenon around her left shoulder (Figure 1). While examining the patient we found multiple stony hard irregular lumps in buttocks, left scapula, anterior fold of left axilla and in Para-spinal muscles. She had a kyphotic posture and the Para-spinal muscles had multiple swellings along the cervical, thoracic and lumbar vertebrae. Spine movements from cervical to lumbar region were absent. The left shoulder and both hip movements were also restricted. We also noted a bilateral hallux valgus deformity in her feet. She had no neurological abnormality. She was born of a consanguineous marriage to an unaffected 32 year old mother. It was an uneventful normal vaginal delivery. She had normal developmental milestones. Her family history was unremarkable. She had five siblings all of whom were normal (Figure 2).
Figure 1: A, Prominent bony swelling in scapula and along paraspinal muscle. B, bilateral hallux valgus deformity.

Figure 2: Chest and pelvic x ray showing heterotrophic ossification.
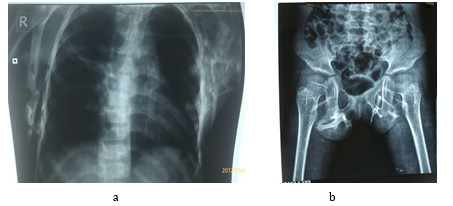
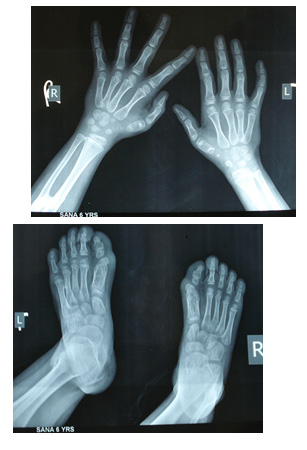
Her blood work and metabolic parameters including serum calcium and alkaline phosphatase were all normal. Her initial radiographs were suggestive of exostosis but based on the history and examination we were suspecting FOP (Fibrodysplasia Ossificans Progressiva). We obtained her foot and hand radiographs, which showed, first ray shortening (Figure 3). We did a 3-dimentional (3D) CT scan of the pelvis in order to confirm that the ossifications were extra-skeletal hence confirming our diagnosis of FOP (Figure 4). After confirming the diagnosis of FOP, the parents were counseled regarding prognosis of the disease. They were given instructions to avoid tissue trauma and intra-muscular injections. The patient was discharged on cox 2 (cyclo-oxygenase-2) inhibitors (25mg/day) and montelukast (10mg / day). We plan to do regular follow up.
Figure 3: 3D scan showing heterotrophic ossification near the pelvic bone.
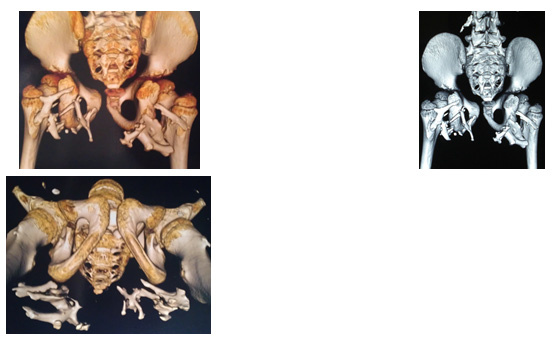
Figure 4: Short first metacarpal and metatarsal bones.
Case Report 2
We report another case of 10-year-old female patient who came to us as outdoor patient with complaint of multiple bony swellings and stiffness of spine and hip. The patient had gone through a number of investigations prior to our visit ,but no definite diagnosis had been met. We admitted the patient and obtained detailed history followed by clinical examination. The patient had hard bony swellings on the back .The parents observed the swelling at age of 3 year on back .Initially they were small and multiple, with time the swellings increased in number, they were extending in continuity from skull to buttocks.
While examining the patient we found swellings, which were like cords extending from skull in continuity to buttocks and spreading to both shoulder as well (Figure 5).The whole spine from occiput to pelvis was rigid, there was no movement possible at cervical, thoracic and lumber spine as well hip joints. She had a kyphotic posture. The shoulder movements on both sides were also restricted. We also noted a bilateral hallux valgus deformity in her feet. She had no neurological abnormality. She was born of a nonconsanguineous marriage to an unaffected 35-year-old mother.
It was an uneventful normal vaginal delivery. She had normal developmental milestones. Her family history was unremarkable. She had 2 siblings all of whom were normal.
Figure 5: Prominent bony swelling extending from skull to buttocks.

Figure 6: 3D scan showing heterotrophic ossification from skull to pelvic bone.

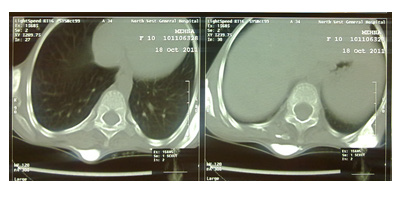
Her blood work and metabolic parameters including serum calcium and alkaline phosphatase were all normal . We did a 3-dimentional (3D) CT scan of the pelvis in order to confirm that the ossifications were extra-skeletal hence confirming our diagnosis of FOP (Figure 6). After confirming the diagnosis of FOP, the parents were counseled regarding prognosis of the disease. They were given instructions to avoid tissue trauma and intra-muscular injections. The patient was discharged on cox 2 (cyclo-oxygenase-2) inhibitors (25mg/day) and montelukast (10mg / day). We plan to do regular follow up (Figure 7).
Figure 7: Tranverse section showing heterotrophic ossification posterior to paraspinal muscles.
Case Report 3
We report another case of 25-year-old male patient who came to us as outdoor patient with complaint of multiple bony swellings and stiffness of spine and hip. The patient had gone through a number of investigations prior to our visit, but no definite diagnosis had been met. We admitted the patient and obtained detailed history followed by clinical examination. He was walking with help of cane in his hand with flexion attitude of left hip and knee and heel raised from ground. He had kyphotic posture , multiple bony swellings on the back. Multiple cords like structures non tender running from occiput to pelvis and arm to trunk were palpable (Figure 8). No movement was possible in cervical, thoracic and lumbar spine. Shoulder and hip movement were also grossly restricted. He had no neurological abnormality. He was born of a non-consanguineous marriage to an unaffected 35-year-old mother. It was an uneventful normal vaginal delivery. She had normal developmental milestones. Her family history was unremarkable.
Figure 8: A, Prominent bony swelling in scapula and along paraspinal muscle. B, flexion attitude at left hip and knee.

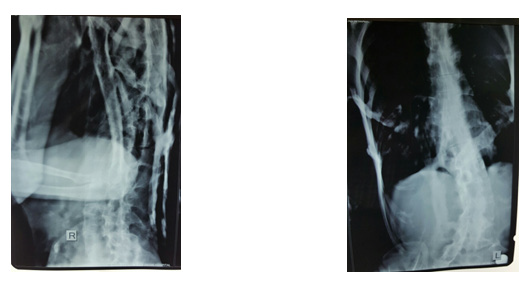
Her blood work and metabolic parameters including serum calcium and alkaline phosphatase were all normal. His x rays spine were obtained showed characteristic ossified band in soft tissues (Figure 9). After confirming the diagnosis of FOP, the parents were counseled regarding prognosis of the disease. They were given instructions to avoid tissue trauma and intra-muscular injections. The patient was discharged on cox 2 (cyclo-oxygenase-2) inhibitors (25mg/day) and montelukast (10mg / day). We plan to do regular follow up.
Figure 9: Chest AP and lateral x ray showing heterotrophic ossification.
Discussion
Fibrodysplasia Ossificans Progressiva (FOP) is a rare disease with incidence of 1 in 200,000 [9]. Only 700 cases have been reported so far throughout the world. The disease has a predilection towards female sex [1,5]. It occurs mostly sporadically but it has got an autosomal dominant inheritance. The disease is characterized by two clinical features, congenital hallus valgus and soft tissue ossifications [10]. This severely disabling disease usually starts around 3-6 years of age. Patients commonly present with an indurated swelling initially, the swelling subsides but leads to new bone formation in the underlying tissues. As the disease progresses, so does the soft tissue and muscle ossification. Ossifications first appear in axial musculature, mainly in the scapular region and in the buttocks. With passage of time the limbs are fixed to body by new bone formation. The Cardiac muscles, smooth muscles and laryngeal muscles are spared however. The disease is aggravated with trauma and viral infections and ultimately renders the patient wheelchair bound by the second decade and leads to death as a result of respiratory compromise by the fourth decade of life [1,8,11].
Approximately 90% of FOP patients worldwide are misdiagnosed, and 67% undergo dangerous and unnecessary diagnostic procedures that lead to permanent harm and lifelong disability in nearly half of all the affected individuals. Patients with FOP are commonly subjected to unnecessary procedures such as incisional/excisional biopsies and amputations. Such procedures inevitably exacerbate the progression of disease and can lead to permanent lifelong disability [12].
Routine biochemical evaluations do not contribute to making the diagnosis. Plain x-rays can substantiate more subtle great toe abnormalities, short first ray and the presence of heterotrophic ossification. Three dimensional (3D) CT scan helps a great deal in confirming the extra skeletal ossification [13]. Although the diagnosis of FOP can be made on the basis of the two classic clinical features (malformation of the great toes and progressive heterotrophic ossification) but identification of the recurrent single nucleotide mutation that causes FOP now provides a level of molecular certainty to the diagnosis at an early stage in the disease. However, this genetic testing is only available on research basis [1,7,14]. Biopsy is not recommended for diagnosis [3]. FOP is frequently confused with myosifying myositis, osteomas, sarcomas, exostosis, juvenile fibromatosis, desmiod tumours and congenital anomalies [2,15].
Although no curative treatment is yet possible, the avoidance of tissue trauma including intra-muscular injections, reduction of falls and modification of daily activities can lead to less aggressive ossification. Glucocorticoids can be used in new flare-ups affecting the function of major joints in the appendicular skeleton. Nonsteroidal anti-inflammatory medications such as cyclo-oxygenase-2 inhibitors, leukotriene inhibitors and mast cell stabilizers are useful anecdotally in managing chronic discomfort and ongoing flare-ups, but to date there is no proven efficacy with any therapy in altering the natural history of the disease [1,3,8,16,17].
Conclusion
Fibrodysplasia Ossificans progressive is a rare disease with no curative treatment but its recognition at an early stage is essential in order to reduce the iatrogenic triggers to progression of this disease, in the form of unnecessary biopsy and avoidance of further trauma and life style modification which can slow down progression of this disease. Further research is required to look for a curative treatment of this disease.
References
- Botman E, Netelenbos JC, Rustemeyer T, Schoonmade LJ, Nieuwenhuijzen JA, et al. (2020) Radiotherapy in fibrodysplasia ossificans progressiva: A case report and systematic review of the literature. Front Endocrinol (Lausanne) 11: 6.
- Pignolo RJ, Wang H, Kaplan FS (2020) Fibrodysplasia Ossificans Progressiva (FOP): A segmental progeroid syndrome. Front Endocrinol (Lausanne) 10: 908.
- Haga N, Nakashima Y, Kitoh H, Kamizono J, Katagiri T, et al. (2020) Fibrodysplasia ossificans progressiva: Review and research activities in Japan. Pediatr Int 62(1): 3-13.
- Matsuo K, Chavez RD, Barruet E, Hsiao EC (2019) Inflammation in fibrodysplasia ossificans progressiva and other forms of heterotopic ossification. Curr Osteoporos Rep 17(6): 387-394.
- Pacifici M (2018) Retinoid roles and action in skeletal development and growth provide the rationale for an ongoing heterotopic ossification prevention trial. Bone 109: 267-275.
- Gencer-Atalay K, Ozturk EC, Yagci I, Ata P, Delil K, et al. (2019) Challenges in the treatment of fibrodysplasia ossificans progressiva. Rheumatol Int 39(3): 569-576.
- Lees-Shepard JB, Goldhamer DJ (2018) Stem cells and heterotopic ossification: Lessons from animal models. Bone 109: 178-186.
- Hsiao EC, Di Rocco M, Cali A, Zasloff M, Al Mukaddam M, et al. (2019) Special considerations for clinical trials in fibrodysplasia ossificans progressiva (FOP). Br J Clin Pharmacol 85(6): 1199-1207.
- Alessi Wolken DM, Idone V, Hatsell SJ, Yu PB, Economides AN (2018) The obligatory role of Activin A in the formation of heterotopic bone in Fibrodysplasia Ossificans Progressiva. Bone 109: 210-217.
- Qi Z, Luan J, Zhou X, Cui Y, Han J (2017) Fibrodysplasia ossificans progressiva: Basic understanding and experimental models. Intractable Rare Dis Res 6(4): 242-248.
- Katagiri T (2016) Fibrodysplasia ossificans progressiva and osteoimmunology. Clin Calcium 26(5): 691-698.
- Kaplan FS, Pignolo RJ, Shore EM (2016) Granting immunity to FOP and catching heterotopic ossification in the Act. Semin Cell Dev Biol 49: 30-36.
- Hüning I, Gillessen-Kaesbach G (2014) Fibrodysplasia ossificans progressiva: clinical course, genetic mutations and genotype-phenotype correlation. Mol Syndromol 5(5): 201-211.
- Nakahara Y, Katagiri T, Ogata N, Haga N (2014) ACVR1 (587T>C) mutation in a variant form of fibrodysplasia ossificans progressiva: second report. Am J Med Genet A 164A(1): 220-224.
- Pignolo RJ, Shore EM, Kaplan FS (2013) Fibrodysplasia ossificans progressiva: diagnosis, management, and therapeutic horizons. Pediatr Endocrinol Rev 10 (Suppl 2): 437-448.
- Miao J, Zhang C, Wu S, Peng Z, Tania M (2012) Genetic abnormalities in fibrodysplasia ossificans progressiva. Genes Genet Syst 87(4): 213-219.
- Lin H, Shi F, Gao J, Hua P (2019) The role of Activin A in fibrodysplasia ossificans progressiva: a prominent mediator. Biosci Rep 39(8).
© 2022 Muhammad Inam. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






