- Submissions

Full Text
Orthopedic Research Online Journal
Clinical Outcomes of Transforaminal Percutaneous Endoscopic Lumbar Discectomy in Malaysia
Colin Komahen1, Ren Yi Kow2*, Naveen Vijayasingam1, Fatihah Mahmud3, Chooi Leng Low4 and Jayamalar Thurairajasingam1
1Department of Orthopaedic. Hospital Sultan Ismail, Johor Bahru, Malaysia
2Department of Orthopaedics, Traumatology & Rehabilitation, International Islamic University Malaysia, Malaysia
3Clinical Research Centre (CRC), Hospital Tengku Ampuan Afzan, Pahang, Malaysia
4Department of Radiology, International Islamic University Malaysia, Malaysia
*Corresponding author: Ren Yi Kow, Department of Orthopaedics, Traumatology & Rehabilitation, International Islamic University Malaysia, Malaysia
Submission: February 07, 2022;Published: February 14, 2022

ISSN: 2576-8875 Volume9 Issue2
Abstract
Background: Chronic low back pain secondary to lumbar disc herniation is common and debilitating to patients. Those patients who do not respond to conservative management are traditionally treated with open lumbar discectomy. With the advent of Minimally Invasive Spine Surgery (MISS) technique, Transforaminal Percutaneous Endoscopic Discectomy (TPED) has been practiced with much success. In contrast to open discectomy, TPED breaches only the skin and subcutaneous tissue from the lateral aspect, minimizing trauma to the soft tissue. Nevertheless, the documented clinical outcome of this new technique is scarce among the Malaysian population. We aim to present clinical outcomes of TPED among the Malaysian population.
Methods: All patients who had undergone treatment for prolapsed intervertebral discs at Hospital Sultan Ismail, Johor Bahru, from 1st of January 2019 to 1st of June 2020 were screened for suitability to be included in this retrospective study. Patients who had undergone TPED at this centre were recruited. Those who underwent open discectomy were excluded. Only patients with minimum 1-year follow-up were included in this study. Patient characteristics were presented descriptively. Analysis of the pre-operative and post-operative Visual Analogue Scale (VAS) and Oswestry Disability Index was done with SPSS V21.0 (IBM, Armonk, NY).
Results: A total of 30 patients were included in this study with a mean age of 40.7 years. Majority of patients (n=25; 83.3%) presented with radiculopathy only. The mean duration of symptoms was 6.5 months. Most patients had diseased discs at L4/L5 (n=15; 50%) and L5/S1 (n=8; 26.7%) with subarticular region as the most common location of disc protrusion (n=18; 60%). The patients’ mean Visual Analogue Scale (VAS) score significantly reduced from 6.3 to 2.2 at post-operative 1 month, 2.4 at post-operative 6 months and 2.0 at post-operative 1 year (p<0.001). The mean Oswestry Disability Index significantly improved from 45.1 to 22.0 after the surgery (p<0.001). More than three-quarter of patients had excellent (n=10; 33.3%) and good (n=11; 36.7%) outcomes based on the Macnab criteria. Only three patients had complications (nerve root injury, recurrence, and skin irritation). There was no association between Macnab outcomes and patients’ characteristics.
Conclusion: TPED is safe and effective in managing patients with prolapsed intervertebral discs among the Malaysian population. Improvement in terms of visual analogue score and Oswestry Disability Index is significant up to 1 year after TPED.
Background
Chronic back pain is a common symptom suffered by patients and up to 85% of the population experience it at least once during their lifetime [1-3]. Lumbar Disc Herniation (LDH) is a condition in which the intervertebral disc (nucleus pulposus or the annulus fibrosus or both) protrudes beyond the intervertebral space [4-6]. The herniated disc may cause compression of the spinal nerve root, thereby precipitating the low back pain and radiating pain to the lower limb [4-6]. Most of the patients will be treated conservatively, in the form of physical therapy, oral non-steroidal analgesic, and epidural steroid injection [7-9]. Nonetheless, up to 20% of the recalcitrant patients who do not respond to trial of nonoperative management or present with neurological deficit, require surgical intervention to alleviate the compression on spinal nerve roots [8-10].
Traditionally, Open Lumbar Discectomy (OLD) has been practised with success on patients with LDH [9-13]. OLD procedure involves a midline incision, retraction of paravertebral muscles, laminotomy and extraction of ligamentum flavum and disc material [5-13]. With the advent of Minimally Invasive Spine Surgery (MISS) technique, Transforaminal Percutaneous Endoscopic Discectomy (TPED) has been practiced with much success [13-16]. In contrast to OLD, TPED breaches only the skin and subcutaneous tissue from the lateral aspect, minimizing trauma to the soft tissue. Nevertheless, the documented clinical outcome of this new technique is scarce in the Malaysian population. We aim to present clinical outcomes of TPED among the Malaysian population.
Material and Methods
This retrospective study was performed at Hospital Sultan Ismail, Johor Bahru, a 704-bed tertiary center in the south of Peninsular Malaysia. All spinal surgeries were performed by three different spine surgeons. All patients with prolapsed intervertebral discs who had been treated at this center from 1st of January 2019 to 1st of June 2020 were screened for suitability to be included in this study. The inclusion criterias were:
A. Age more than 18 years
B. Undergone transforaminal percutaneous endoscopic discectomy (TPED) during the study period
C. Completed a minimum of 1-year follow-up
The exclusion criteria included:
A. Patients who underwent open discectomy
B. Incomplete data
C. Did not complete a minimum of 1-year follow-up
All patients undergone TPED under local anaesthesia. All surgeries lasted less than one hour. The patient was positioned in a prone position with proper padding. The disc locations were checked and marked under image intensifier in both anteroposterior (AP) and lateral positions. The entry point on the skin was generally located at 9-10cm lateral to the midline. After local anaesthetic injection, a skin incision was made slightly superior to the marked lateral line to facilitate a downward path to the centre of the disc. A needle was then inserted under image intensifier guidance until the tip of the needle was located just lateral to the medial pedicle line on the AP view and at the posterior annulus on the lateral view. Once the correct placement of needle was secured, the stylet of the needle was replaced by a guidewire and the needle was then removed, leaving only the guidewire. After sequential transforaminal passage of reamers of different sizes, the cannula and endoscope were carefully inserted. A grasper was used to remove the pathological fragments. The adequacy of removal was determined by: A) the fragment appeared red at the tip due to epidural vascular reaction; B) the center of disc appeared red due to oozing of epidural veins into the disc, and C) the patient inform the surgeon that the previously experienced pain was relieved. All patients were discharged on the next day after the surgery.
In this review, the following parameters were extracted from medical records: (i) age, (ii) gender, (iii) smoking status, (iv) co-morbidity, (v) duration of disease, (vi) level of disease, (vii) symptoms, (viii) side of disc, and (ix) location of disc.
Patients were assessed with the Visual Analogue Scale (VAS), Oswestry Disability Index (ODI), and Macnab criteria, both preoperatively and post-operatively. The VAS was assessed postoperatively at 1 month, 6 months and 1 year. The Oswestry Disability Index and Macnab criteria were assessed at 1-year post-operation. Presence of complication and whether the patient had undergone additional procedures post-operatively were also documented. All patients were assessed by the lead author and a consultant spine surgeon, both pre-operatively and post-operatively.
The collected data was processed using SPSS V21.0 (IBM, Armonk, NY). Patients’ demographic data and diseased disc characteristics were descriptively presented. The difference between pre-operative and post-operative VAS and Oswestry Disability Index was analysed using paired t-test. Univariate analysis was used to investigate the association between the patients’ satisfaction (Macnab criteria) and patients’ demographic data as well as disc characteristics. A p-value of <0.05 indicated a statistically significant difference.
Results
During the investigation period, 30 eligible patients met the inclusion criteria. The demographic data of these patients was summarized in Table 1. The mean age of patients was 40.7 years. There were 18 (60%) male patients and 12 (40%) female patients. Majority of patients were non-smokers (24 patients, 80%). Less than one-third of patients (9 patients, 30%) had co-morbidities at the time of treatment. The mean duration of disease prior to surgical intervention was 8.7 months.
Table 1: Demographic data of all recruited patients. n- frequency; SD- standard deviation.
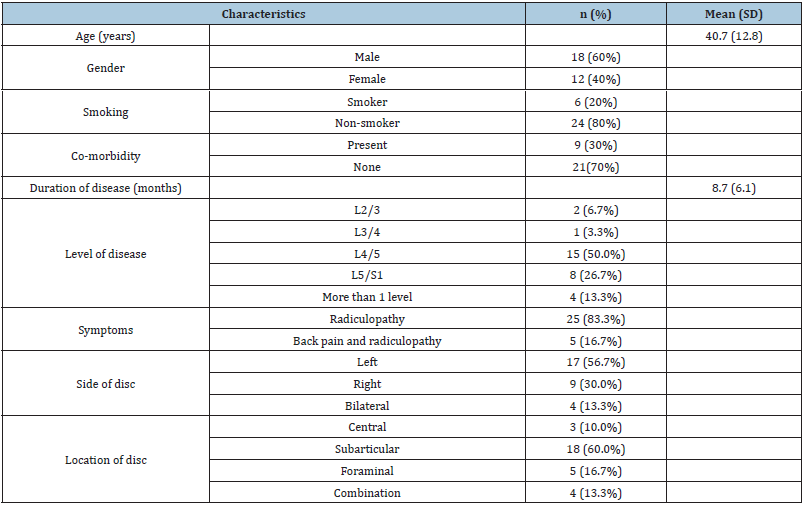
Half the patients (15 patients, 50%) presented with LDH at L4/ L5 level. This is followed by L5/S1 (8 patients, 26.7%), multilevel (4 patients, 13.3%), L2/L3 (2 patients, 6.7%) and L3/L4 (1 patient, 3.3%). Most of the patients presented with radiculopathic symptoms only (25 patients, 83.3%). There were only 5 patients (16.7%) presented with back pain and radiculopathy. More than half of the patients had protruded disc at the left side (17 patients, 56.7%). This is followed by right-sided disc protrusion (9 patients, 30%) and large disc protrusion involving bilateral compression (4 patients, 13.3%). Up to three-fifth of the protruded discs are located at the subarticular region (18 patients, 60%). This is followed by foraminal region (5 patients, 16.7%), combination (4 patients, 13.3%) and central region (3 patients, 10%).
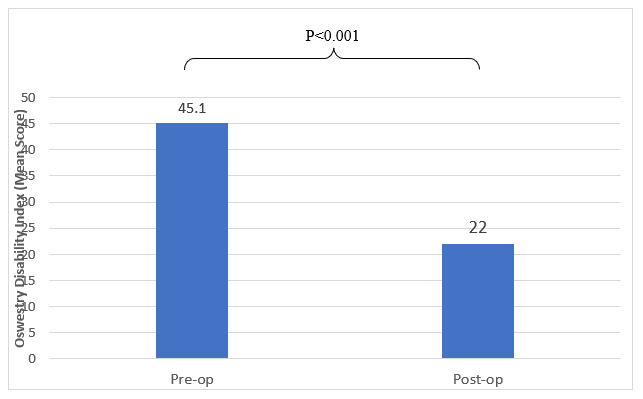
Clinical outcomes of patients who had undergone TPED were summarized in Table 2. The pre-operative mean score for Visual Analogue Scale (VAS) was 6.3. The VAS reduced to 2.2 at one-month post-operation, 2.4 at six-month post-operation and 2.0 at one-year post-operation. It was statistically significant in terms of VAS reduction (p<0.001) as highlighted in Figure 1. The Oswestry Disability Index also significantly improved from 45.1 pre-operatively to 22.0 post-operatively (p<0.001), as shown in Figure 2. Regarding Macnab criteria, two-third of patients reported excellent (10 patients, 33.3%) and good (11 patients, 36.7%) outcomes. Only 4 patients (13.3%) and 3 patients (10.0%) reported fair or poor outcomes respectively. Among these patients, 3 of them had problems, namely nerve root injury, recurrence, and pain at the portal scar. Six patients (20%) required additional procedures after TPED for facet joint arthropathy, in which two of them had radiofrequency ablation and four of them had facet joint steroid injections.
Table 2: Clinical outcomes of transforaminal percutaneous endoscopic discectomy.
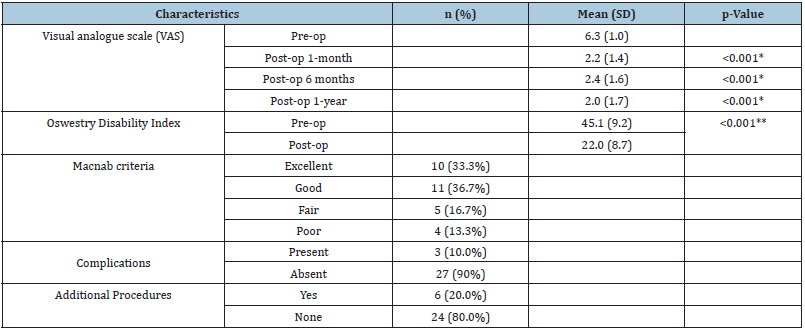
n- number; SD standard deviation
*paired t-test comparison with pre-operative VAS
**paired t-test comparison with pre-operative ODI
Figure 1: Comparison of pre-operative VAS and post-operative VAS.
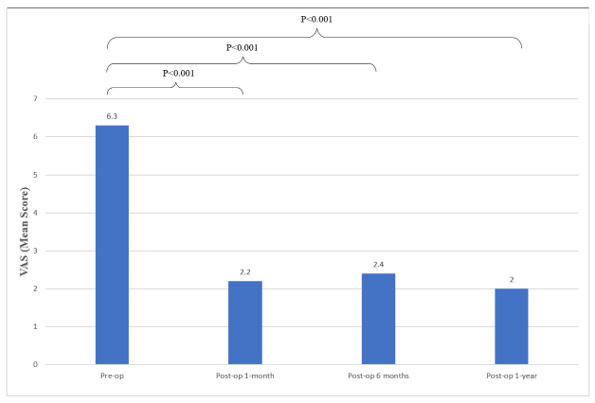
Figure 2: Comparison of pre-operative ODI and post-operative ODI.
Univariate analysis was performed to determine the association between Macnab criteria and patients’ characteristics as outlined in Table 3. There was no association between Macnab criteria and patients’ characteristics except for location of the disc (p<0.05). All three patients with central disc protrusion reported poor or fair outcomes while majority of patients with other locations of disc protrusion had good or excellent outcomes.
Table 3: The association between MacNab criteria and the patient’s characteristics.
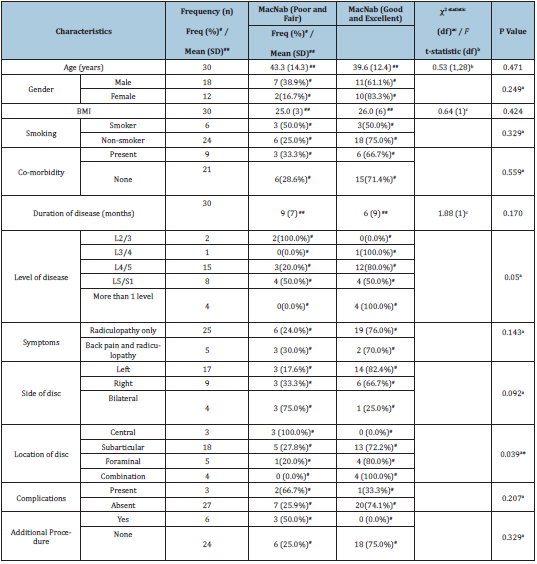
n- number; SD standard deviation
*paired t-test comparison with pre-operative VAS
**paired t-test comparison with pre-operative ODI
Discussion
The conventional Open Lumbar Discectomy (OLD) is a practical method to treat symptomatic lumbar disc herniation (LDH) [5,6]. Nonetheless, violation of the posterior musculoligamentous structures during OLD may induce post-operative back pain and muscle atrophy [17]. Up to one-third of patients suffer from back pain following mechanical trauma secondary to OLD during a longterm follow-up [18]. Among these patients, 9% have debilitating back pain necessitating a subsequent fusion surgery at the level of the primary discectomy [18]. Furthermore, spinal surgery at the thoracolumbar junction is associated with higher risk of infection [19]. Ergo, Transforaminal Percutaneous Endoscopic Discectomy (TPED) which utilises Minimally Invasive Spine Surgery (MISS) principle appears to be an attractive option to treat patients with symptomatic LDH. By creating a lateral portal through the skin and subcutaneous tissue, the midline posterior musculoligamentous structures can be spared [5,6]. Taking advantage of the highdefinition endoscopic vision, dissection of the disc and removal of the pathological fragments are made easier with minimal muscle dissection, if any [5,6].
As highlighted in other studies, TPED demonstrates superiority with regards to short-term back pain and radiculopathy improvement [5,6]. Our results concur with their findings where there is a significant reduction of VAS at one-month, six-month and one-year after the index surgery. Besides that, TPED has shown a comparable improvement of quality of life (ODI) and patients’ satisfaction (Macnab criteria) as OLD [5,6]. A metaanalysis involving 27 studies by Muthu et al reveals a superiority of endoscopic discectomy compared to open microdiscectomy in the aspect of ODI [3]. Similarly, the quality of life of our patients are enhanced at one-year after TPED. With respect to patients’ satisfaction, more than two-third of patients reported excellent and good outcomes which is consistent with other studies.
One of the advantages of TPED is shorter length of hospital stay compared to open surgery [3-6]. Generally, patients undergoing endoscopic surgery are discharged approximately 3 days earlier than their counterparts who undergo open surgery [3-6]. In our study, all patients are warded for three days (admission day, surgery day and discharged home on the following day). This is consistent with other studies whereby the average length of hospital stay is 2.84 days for patients who undergo endoscopic discectomy [3]. Minimal intra-operative blood loss in TPED is also an added benefit to this procedure. Nevertheless, we did not capture this data in our study as the one or two soaked gauzes were not actively weighed during the surgery.
In this study, we found no association between patients’ satisfaction (Macnab criteria) and patients’ characteristics except for location of the disc. All three patients with central disc protrusions were not satisfied with their outcomes. Central lumbar disc protrusion is known to have a poorer outcome compared to disc bulges in other locations [20]. Long-term follow-up (mean 3.3 years) of patients with central lumbar disc herniation by Barlocher et al. [20] showed only 24% of their patients had excellent outcomes [20]. Central lumbar disc herniation is associated with a higher recurrence rate owing to the higher degree of internal disc disruption and unstable posterior longitudinal ligaments [20].
Limitations
There are some limitations in this study. Firstly, retrospective nature of this study precludes some potentially important data. Besides that, a small sample size and involvement of only one centre limit the generalization of this study results to the whole Malaysian population. Likewise, owing to the small sample size and limited variables, we do not perform a multivariate analysis to determine the predictive factor of good patients’ satisfaction in this study. Finally, there is no comparison with open discectomy, hence the risks and benefits of this new technique may not be clearly defined. Nonetheless, despite the above-stated limitations, this is the first study to report on clinical outcomes of TPED among the Malaysian population. Future larger prospective studies may compare TPED and open microdiscectomy to determine the optimal treatment for patients with prolapsed intervertebral discs.
Conclusion
Transforaminal Percutaneous Endoscopic Lumbar Discectomy (TPED) is an effective and safe surgery for patients with lumbar disc herniation in the Malaysian population. Improvement in terms of visual analogue scale and Oswestry Disability Index is significant up to 1 year after TPED. Favourable patients’ satisfaction after TPED is also reported in this study.
References
- Liounakos JI, Wang MY (2020) The endoscopic approach to lumbar discectomy, fusion, and enhanced recovery: A Review. Global Spine J 10(2 Suppl): 65S-69S.
- Xu J, Li Y, Wang B, Lv G, Li L, et al. (2020) Minimum 2-year efficacy of percutaneous endoscopic lumbar discectomy versus microendoscopic discectomy: A meta-analysis. World Neurosurg 138: 19-26.
- Muthu S, Ramakrishnan E, Chellamuthu G (2021) Is endoscopic discectomy the next gold standard in the management of lumbar disc disease? Systematic review and superiority analysis. Global Spine J 11(7): 1104-1120.
- Lee YC, Zotti MGT, Osti OL (2016) Operative management of lumbar degenerative disc disease. Asian Spine J 10(4): 801-819.
- Kim SK, Kang SS, Hong YH, Park SW, Lee SC (2018) Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: a multicenter, retrospective analysis. J Orthop Surg Res 13(1): 22.
- Kim M, Lee S, Kim HS, Park S, Shim SY, et al. (2018) A comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for lumbar disc herniation in the Korean: A meta-analysis. Biomed Res Int 2018: 9073460.
- Hua W, Tu J, Li S, Wu X, Zhang Y, et al. (2018) Full-endoscopic discectomy via the interlaminar approach for disc herniation at L4-L5 and L5-S1: An observational study. Medicine (Baltimore) 97(17): e0585.
- Phan K, Xu J, Schultz K, Alvi MA, Lu VM, et al. (2017) Full-endoscopic versus micro-endoscopic and open discectomy: A systematic review and meta-analysis of outcomes and complications. Clin Neurol Neurosurg 154: 1-12.
- Sivakanthan S, Hasan S, Hofstetter C (2020) Full-endoscopic lumbar discectomy. Neurosurg Clin N Am 31(1): 1-7.
- Marappan K, Jothi R, Raj SP (2018) Microendoscopic Discectomy (MED) for lumbar disc herniation: comparison of learning curve of the surgery and outcome with other established case studies. J Spine Surg 4(3): 630-637.
- Kanno H, Aizawa T, Hahimoto K, Itoi E (2019) Minimally invasive discectomy for lumbar disc herniation: current concepts, surgical techniques, and outcomes. Int Orthop 43(4): 917-922.
- Ahn Y (2019) Endoscopic spine discectomy: indications and outcomes. Int Orthop 43(4): 909-916.
- Ahn Y (2012) Transforaminal percutaneous endoscopic lumbar discectomy: technical tips to prevent complications. Expert Rev Med Devices 9(4): 361-366.
- Jarebi M, Awaf A, Lefranc M, Peltier J (2021) A matched comparison of outcomes between percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for the treatment of lumbar disc herniation: a 2-year retrospective cohort study. Spine J 21(1): 114-1121.
- Wu K, Zhao Y, Feng Z, Hu X, Chen Z, et al. (2020) Stepwise local anesthesia for percutaneous endoscopic interlaminar discectomy: Technique strategy and clinical outcomes. World Neurosurg134: e346-352.
- Sanusi T, Davis J, Nicassio N, Malik I (2015) Endoscopic lumbar discectomy under local anaesthesia may be an alternative to microdiscectomy: A single centre’s experience using the far lateral approach. Clin Neurol Neurosurg 139: 324-327.
- Wu CY, Jou IM, Yang WS, Yang CC, Chao LY, et al. (2014) Significance of the mass-compression effect of postlaminectomy/laminotomy fibrosis on histological changes on the dura mater and nerve root of the cauda equina: an experimental study in rats. J Orthop Sci19(5): 798-808.
- Parker SL, Xu R, McGirt MJ, Witham TF, Long DM, et al. (2010) Long-term back pain after a single-level discectomy for radiculopathy: incidence and health care cost analysis. J Neurosurg Spine 12(2): 178-182.
- Khan ES, Kow RY, Arifin KBBM, Komahen C, Low CL, et al. (2019) Factors associated with deep surgical site infection following spinal surgery: A pilot study. Cureus 11(4): e4377.
- Barlocher CB, Krauss JK, Seiler RW (2000) Central lumbar disc herniation. Acta Neurochir (Wien) 142(12): 1369-1375.
© 2022 Ren Yi Kow. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






