- Submissions

Full Text
Orthopedic Research Online Journal
Inguinomalacia: Alternative Nomenclature to the Sports Hernia
José Martins Juliano Eustaquio1*
1Mário Palmerio Hospital, University of Uberaba (UNIUBE - Universidade de Uberaba), Uberaba, Minas Gerais, Brazil
*Corresponding author: José Martins Juliano Eustaquio, Mário Palmerio Hospital, University of Uberaba (UNIUBE – Universidade de Uberaba). Av. Cecília Palmerio, s/n, Uberaba, MG, Brazil
Submission: January 24, 2022;Published: January 27, 2022

ISSN: 2576-8875 Volume9 Issue2
Abstract
The groin pain syndrome affects athletes with high incidence and, mainly due to the anatomical complexity of the pelvic region and the difficult management of its pathologies, it is the subject of great debate in the scientific community. One of these disagreements is in relation to the nomenclature employed in sports hernia, as it does not translate the reality as to its pathophysiological findings. In fact, there is no hernial sac in this condition, but a weakness of the posterior wall of the inguinal canal and, with it, the protrusion of the omentum (pre-peritoneal) fat. In this article, it is proposed to create and use the term ʻʻinguinomalaciaʼʼ as a replacement for sports hernia.
Introduction
The groin pain syndrome [1], despite being a nonspecific term and much discussed in the literature, is an objective initial parameter for the diagnostic reasoning of the athletes with a disorder in this anatomical segment. In general, it includes pathologies that are difficult to diagnose and treatment, as well as many differential diagnoses that present similar pathophysiological and clinical characteristics [2].
In addition, some pathologies may coexist, in particular associated cases of osteitis pubis (athlete’s pubic pain) and sports hernia [3]. However, these pathologies and their nomenclatures are still difficult to understand and are the subject of debate in the scientific community, especially in relation to sports hernia [2,4]. This article will address an alternative nomenclature for sports hernia, which is one of the reasons for confusion, as well as a mini review of the main factors related to its management.
Opinion
Proposal to change the nomenclature sports hernia
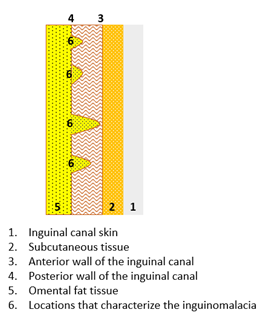
The term athlete’s hernia is a matter of disagreement among different authors [1,2], since the condition does not involve the protrusion of a hernial sac with part of an abdominal viscera, characteristic of classic hernia, but rather the protrusion of omental fat into the inguinal region (Figure 1). This protrusion occurs due to multifocal weakening of the posterior wall of the inguinal canal [5,6], with consequent compression of inguinal sensory nerves [7].
Moreover, some authors consider that sports hernia and osteitis pubis are synonyms for the same pathology [1,3], since they may share similar signs and symptoms and even occur together in the same patient. However, it is observed in clinical practice that they are distinct pathologies and, as such, should be approached differently.
Figure 1: Representative illustration of the anatomical layers of the inguinal canal and the points of weakness of the posterior wall of the inguinal canal, which characterize the inguinomalacia (Author’s own file).
Despite the recent positions of some Consensus on the appropriate expressions in reference to sports hernia [2,8], their recommendations are not routinely employed among health professionals. As an example, the British Hernia Society Consensus, published in 2014, suggested the use of the term ʻʻInguinal disruptionʼʼ [8]. Whereas the World Conference on Groin Pain in Athletes, held in Doha in 2014, suggested the adoption of the expression ʻʻInguinal-related groin painʼʼ [2].
Because of these factors, the use of an alternative term to sports hernia is interesting because the current terminology does not clearly express its pathophysiology and still causes confusion among health professionals. In this sense, as the pathology is characterized by an anatomical weakness of part of the floor of the inguinal canal, the current article proposes the use of the term inguinomalacia to replace sports hernia.
The suffix ʻʻmalaciaʼʼ is commonly employed in the medical literature to express pathological alterations similar to the one found in this disturb [9,10]. Thus, with this nomenclature, a more objective notion of the pathology is allowed, without referring to more generic expressions such as ʻʻInguinal-related groin painʼʼ and still avoids confusion with the term hernia.
General features of inguinomalacia
Pain in the inguinal region, which is one of the alterations that characterize the athlete’s groin pain syndrome, is commonly found in athletes who practice sports related to pliometric and rotational movements, especially in soccer [11]. In a large proportion of those affected, this condition evolves with significant limitation of performance in sports.
The main pathologies that make the differential diagnosis of this syndrome in athletes are osteitis pubis, proximal lesion of the adductor muscles, intra-articular pathologies of the hip and inguinal hernias [12]. These conditions often share similar clinical alterations, which makes clinical diagnosis difficult to make. The main complaint in common between them is pain in the groin and adductor regions, which worsens with rotational movements and active adduction of the hips against resistance [1]. The classical scenario of the patient when seeking medical care is of a chronic pathology with frequent aggravations and, very often, based on misdiagnoses, which makes treatment increasingly complex.
Moreover, the presence of some of these pathologies concomitantly is frequent, mainly because they share similar pathophysiological mechanisms [12]. In these cases, besides the supraphysiological mechanical stress typical of certain sports, muscle imbalances are also observed between the abdominal segment and the proximal region of the lower limbs, with emphasis on a greater relative strength in favor of the adductor muscles [1]. The most commonly observed association is that of inguinomalacia with osteitis púbis [3,11,12].
Figure 2: Dynamic ultrasound images of the inguinal region of an athlete diagnosed with inguinomalacia, without (A) and with (B) exertion through the Valsalva maneuver (Author’s own file).
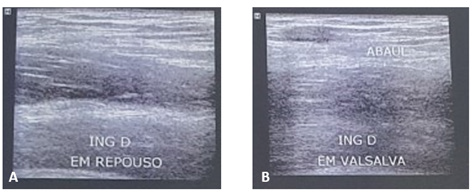
As for inguinomalacia, its diagnosis is possible through dynamic imaging examinations, especially inguinal ultrasonography (Figure 2); [13]. In this examination, the radiologist asks the patient to perform the Valsalva maneuver, in different ways, in order to increase the pressure in the inguinal canal and allow the protrusion of fatty tissue. Static examinations are not able to diagnose this pathology. Other imaging examinations of the pelvis, such as panoramic radiography and magnetic resonance imaging, help in the search for a differential diagnosis [14].
Based on current knowledge [15-17], a practical algorithm is proposed regarding priority treatment options for cases of osteitis pubis, inguinomalacia and their associations, according to the athlete’s performance level (Figure 3). Furthermore, once the diagnosis of inguinomalacia is made, its treatment should be prioritized over other pathologies of the inguinal region.
Thus, for the recreational athlete, in the isolated presence of this pathology, an attempt at conservative treatment for 3 to 6 months is indicated. If this fails, surgical treatment is indicated. However, in the joint presence with osteitis pubis, surgical treatment of inguinomalacia and conservative treatment of osteitis are indicated (Figure 3).
Figure 3: Recommended treatments for osteitis pubis, inguinomalacia and the association of both, in amateur and professional athletes.
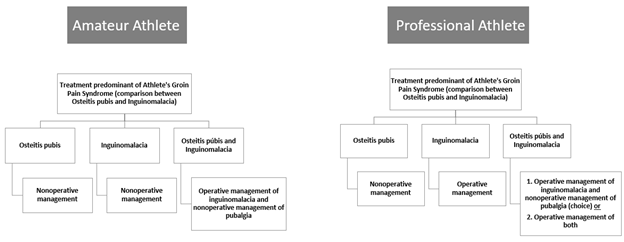
In professional sports, more precisely in modalities that involve pliometric and rotational movements, surgical treatment is indicated whenever inguinomalacia is present, regardless of the coexistence of osteitis pubis (Figure 3). The dynamics of these modalities involves increased abdominal and inguinal pressures, which is precisely the precursor mechanism of pain. Therefore, due to this pathophysiology, the professional demand, and also in order to shorten the time away from the sport, surgical treatment is indicated.
The surgery for inguinomalacia correction is based on the mechanical stabilization of the inguinal canal wall, through the herniorrhaphy procedure, with or without the placement of a mesh, and this includes both open or minimally invasive operative approaches [1,18,19]. This procedure is performed by the general surgeon. If joint surgical treatment of osteitis pubis is indicated, the presence of both the general surgeon and the orthopedic surgeon is required [12].
Conclusion
Osteitis pubis and sports hernia are different pathologies, very incident in the athlete population and that are commonly present together in the same patient. As an alternative to the term sports hernia, which causes much confusion in the scientific literature, we propose the use of the term inguinomalacia.
Conflict of Interests
Author declared no conflict of interests regarding the publication of this manuscript.
References
- Zuckerbraun BS, Cyr AR, Mauro CS (2020) Groin pain syndrome known as sports hernia: A Review. JAMA Surg 155(4): 340-348.
- Weir A, Brukner P, Delahunt E, Ekstrand J, Griffin D, et al. (2015) Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med 49(12): 768-774.
- Elattar O, Choi HR, Dills VD, Busconi B (2016) Groin injuries (athletic pubalgia) and return to play. Sports Health 8(4): 313-323.
- Kingston JA, Jegatheeswaran S, Macutkiewicz C, Campanelli G, Lloyd DM, et al. (2014) A European survey on the aetiology, investigation and management of the “sportsman’s groin.” Hernia 18(6): 803-810.
- Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ (2011) Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy 27(2): 252-269.
- van Veen RN, de Baat P, Heijboer MP, Kazemier G, Punt BJ, et al. (2007) Successful endoscopic treatment of chronic groin pain in athletes. Surg Endosc 21(2): 189-193.
- Comin J, Obaid H, Lammers G, Moore J, Wotherspoon M, et al. (2013) Radiofrequency denervation of the inguinal ligament for the treatment of ‘sportsman’s hernia’: a pilot study. Br J Sports Med 47(6): 380-386.
- Sheen AJ, Stephenson BM, Lloyd DM, Robinson P, Fevre D, et al. (2014) Treatment of the sportsman’s groin’: British Hernia Society’s 2014 position statement based on the Manchester Consensus Conference. Br J Sports Med 48(14): 1079-1087.
- Hysinger EB (2018) Laryngomalacia, tracheomalacia and bronchomalacia. Curr Probl Pediatr Adolesc Health Care 48(4): 113-118.
- Kim YK, Yoo JD, Oh M, Cho E, Kim NK (2021) Patellofemoral chondromalacia does not influence radiographic and clinical outcomes following high tibial osteotomy. J Knee Surg 34(7): 685-692.
- Candela V, De Carli A, Longo UG, Sturm S, Bruni G, et al. (2021) Hip and groin pain in soccer players. Joints 7(4): 182-187.
- Kraeutler MJ, Mei-Dan O, Belk JW, Larson CM, Talishinskiy T, et al. (2021) A Systematic review shows high variation in terminology, surgical techniques, preoperative diagnostic measures, and geographic differences in the treatment of athletic pubalgia/sports hernia/core muscle injury/inguinal disruption. Arthroscopy 37(7): 2377-2390.
- Vasileff WK, Nekhline M, Kolowich PA, Talpos GB, Eyler WR, et al. (2017) Inguinal hernia in athletes: Role of dynamic ultrasound. Sports Health 9(5): 414-421.
- Bou Antoun M, Reboul G, Ronot M, Crombe A, Poussange N, et al. (2018) Imaging of inguinal-related groin pain in athletes. Br J Radiol 91(1092): 20170856.
- Castle JP, Kessler A, Abbas MJ, Wager S, Khalil LS, et al. (2021) High return to play rate and reduced career longevity following surgical management of athletic pubalgia in national basketball association players. Arthrosc Sports Med Rehabil 3(5): e1359-e1365.
- Choi HR, Elattar O, Dills VD, Busconi B (2016) Return to play after sports hernia surgery. Clin Sports Med 35(4): 621-36.
- Drager J, Rasio J, Newhouse A (2020) Athletic pubalgia (Sports Hernia): Presentation and treatment. Arthroscopy 36(12): 2952-2953.
- Minnich JM, Hanks JB, Muschaweck U, Brunt LM, Diduch DR (2011) Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med 39(6): 1341-1349.
- Hatem M, Martin RL, Bharam S (2021) Surgical outcomes of inguinal-, pubic-, and adductor-related chronic pain in athletes: A systematic review based on surgical technique. Orthop J Sports Med 9(9): 23259671211023116.
© 2022 José Martins Juliano Eustaquio. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






