- Submissions

Full Text
Orthopedic Research Online Journal
Ulnar Collateral Ligament Reconstruction: Allograft Versus Autograft – A Systematic Review
Austin Moore DO1, Dylan Matthews DO1, Julie Stausmire2, Amy Singleton BS1*, Kirk Davis DO1 and Anil Gupta MD3
1Department of Orthopedics, Mercy Health St Vincent Medical Center, 2409 Cherry Street, USA
2Regional Academic Affairs, Mercy Health St Vincent Medical Center, 2215 Cheery Street, USA
3Toledo Orthopedic Surgeons, 2865 N Reynolds Rd, USA
*Corresponding author:Amy Singleton BS, Department of Orthopedics, Mercy Health St Vincent Medical Center, 2409 Cherry Street, USA
Submission: August 16, 2021;Published: August 31, 2021

ISSN: 2576-8875 Volume8 Issue4
Abstract
Background: Ulnar Collateral Ligament (UCL) reconstruction of the elbow, a Tommy John surgery, is a common procedure often performed in throwing athletes. Autograft tendon has traditionally been utilized, although recently allograft tendon has been of interest due to the possibility of decreasing donor site morbidity. There is a lack of literature on patient outcomes and complication rates following the use of allograft tendon for UCL reconstruction. Currently, there is no consensus on utilizing autograft versus allograft tendon for UCL reconstruction.
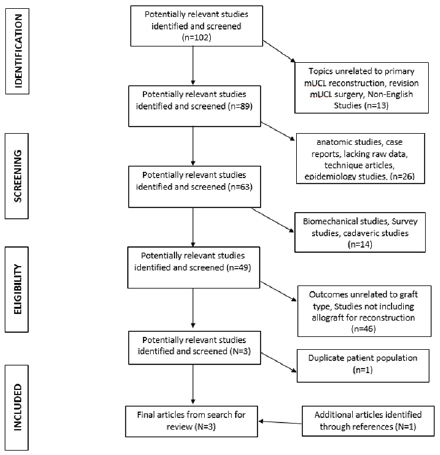
Methods: A PRISMA compliant literature search in online databases Medline, Cochrane and Embase was performed for level 4 and higher studies through June 2019. Any studies reporting clinical outcome results of allograft reconstruction were included. Exclusion criteria included studies unrelated to primary UCL reconstruction, studies specifically looking at revision UCL reconstruction, epidemiological studies, case reports, studies lacking raw data, technique articles, biomechanical studies, cadaveric studies, studies with outcomes unrelated to graft choice, and studies with outcomes unrelated to the use of allograft tendon for reconstruction. Studies were analyzed for graft type, functional scores, return to play rate, and complication rates.
Results: Three out of 103 studies met inclusion criteria. Two cohort studies and 1 retrospective review were included in this review. No significant differences in functional outcomes regardless of scoring system utilized, return to play rate, or complication rates were found between allograft versus autograft.
Conclusion: The use of allograft tendon appears to have similar outcomes regarding functional scores, return to play, and complication rates compared to autograft tendon. Use of allograft tendon seems to be a viable option for UCL reconstruction, though further studies are needed.
Keywords: Allografts; Autografts; Elbow; Ulnar collateral ligament reconstruction; Tommy john; Elbow instability
Abbreviations: UCL: Ulnar Collateral Ligament; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; KJOC: Kerlan-Jobe Orthopaedic Clinic Shoulder and Elbow Scores; MEPS: Mayo Elbow Performance Scores; OES: Oxford Elbow Scores; DASH: Disabilities of the Arm, Shoulder and Hand Scores
Introduction
Injury to the medial Ulnar Collateral Ligament (UCL) was originally described by Waris [1] in 1946 in Javelin throwers. Today, baseball pitchers are an increasingly common demographic who sustain injuries to the UCL [2]. Commonly, UCL injuries in pitchers are overuse injuries due to the repetitive valgus force applied during the acceleration phase of throwing [2]. Throwing athletes with acute UCL injuries may describe a pop associated with pain and difficulty with throwing. They often have pain during the late cocking and early acceleration phases of throwing. This leads to decreased velocity and accuracy with throwing [3]. UCL injuries are not only limited to the throwing athletes; injury can also occur during any activities that cause repetitive valgus moments on the elbow. Traumatic elbow dislocation can also lead to acute UCL injury. On physical exam, the most common
finding is tenderness to palpation over the medial elbow at the UCL
origin. Patients may or may not report having pain at rest, and many
chronic tears are symptomatic only during a throwing motion [2].
The medial UCL is the primary restraint to valgus stress on the
elbow, and anatomically is divided into 3 components, the anterior
bundle, posterior oblique ligament, and transverse ligament [4].
In the anterior bundle, the anterior oblique ligament originates at
the anteroinferior ridge of the medial epicondyle to the sublime
tubercle, and along its course subdivides into anterior and posterior
bands of which the anterior band is the primary valgus restraint
[5]. The anterior band of the anterior bundle is the primarily
stabilizer from 30 to 120 degrees of flexion while the posterior
band has the same function at terminal phase of elbow flexion
[6]. The transverse ligament does not contribute to stability of the
elbow. During the late cocking and acceleration phases of throwing,
a significant valgus stress is placed on the elbow, which leads to
repetitive micro-trauma to the anterior band of the UCL, which can
eventually lead to rupture.
In 1974, Jobe et al. [7] performed the first successful medial
ulnar collateral ligament reconstruction on baseball pitcher Tommy
John, leading to the procedure’s moniker. Later on, in 1986, Jobe
et al. [7] described a technique for reconstruction of the ligament
with use of ipsilateral palmaris longus tendon autograft via flexor
pronator mass detachment with transposition of ulnar nerve.
Since then, there have been several modifications and variations
of Dr. Jobe’s original technique. There have also been an increasing
number of tendon graft origins for UCL reconstruction that have
been utilized including palmaris, hamstring, plantaris, and Achilles
autograft. Unfortunately, with autograft harvest, there can be
complications involving the graft site including graft site pain,
infection, numbness, and even incidental harvesting of the median
nerve. With recent improved tissue processing techniques, allograft
has become a viable treatment option to avoid donor site morbidity.
To date, there has been a paucity of literature surrounding
outcomes following UCL reconstruction with allograft. The purpose
of this study is to evaluate outcomes after UCL reconstruction with
allograft versus with autograft tendons in regard to functional
scores, return to play rate, and complication rates.
Methods
A systematic review was first registered on Prospero and a
literature search was performed using Preferred Reporting Items
for Systematic Reviews and Meta-Analyses (PRISMA) guidelines
(Figure 1); [8,9]. The search was performed utilizing Medline,
Cochrane, and Embase electronic databases, first in March and
then in June 2019 to identify the most contemporary articles.
Full text versions of articles were reviewed by two independent
resident physician reviewers. Primary search terms included: ulnar
collateral ligament reconstruction, allograft, autograft, Tommy
John, reconstructive surgical procedures, and surgical repair used
in combination and/or independently.
Inclusion criteria were defined as any studies reporting clinical
outcome results of allograft reconstruction. Exclusion criteria for
studies were studies in a non-English language, studies unrelated to
primary medial UCL reconstruction, studies specifically looking at
revision medial UCL reconstruction, epidemiological studies, case
reports, studies lacking raw data, technique articles, biomechanical
studies, cadaveric studies, studies with outcomes unrelated to graft
choice, and studies with outcomes unrelated to the use of allograft
tendon for reconstruction.
Studies with levels of evidence of 4 or higher were included
and then reviewed for identical patient populations. Two studies
by Erickson et alwere identified which included the same patient
population [10,11]. The study with the higher level of evidence
between these two studies was included in our review. The
references of our included studies were then cross examined for
any additional studies which could be included, resulting in one
additional study. Studies identified were then reviewed for graft
type used and various functional outcomes, return to play, and
complications
Figure 1: PRISMA Flowsheet for study inclusion.
Results
Out of 103 studies initially identified in our literature search, 3
met all inclusion criteria. Two studies were level 3 cohort studies,
and one study was a level 4 retrospective review. Of the studies
identified, no significant differences were found between functional
outcome scores, return to play, or return to play at previous level of
competition.
In Erickson et al. [11] a level 3 cohort study, 85 patients between
2004-2013 underwent UCL reconstruction. 11 patients underwent
reconstruction with allograft tendon, 20 underwent reconstruction
with hamstring autograft tendon, and 54 underwent reconstruction
with palmaris autograft tendon. Functional outcomes scores were
reported using the Kerlan-Jobe Orthopaedic Clinic Shoulder and
Elbow Score (KJOC) and the Timmerman-Andrews Score. KJOC
scores for palmaris autograft, hamstring autograft, and allograft
were 91.67±8.59, 89.62±9.12, and 91.66±3.20 respectively
(p=0.251). Timmerman-Andrews Score between the palmaris
autograft, hamstring autograft, and allograft were 91.67±8.59,
93.75±5.82, and 94.55±4.72 respectively (p=0.181). Percentage
of patients who returned to play at the same level or higher as
preinjury was 92.59 % for palmaris autograft, 95% for hamstring
autograft, and 100% for allograft reconstruction (p=0.999). No
difference in complications between the type of graft used was
identified. Complications included reoperation for ulnar nerve
transposition (n=6), ulnar stress fracture (n=1), loss of motion
requiring reoperation with elbow arthroscopy (n=1), and one UCL
re-tear, ultimately treated non-operatively.
Merolla’s et al. [12] study included 15 patients who
underwent UCL reconstruction between 2006-2012. Of the 15
patients, 5 underwent reconstruction with palmaris autograft
and 10 underwent reconstruction with semitendinosus allograft.
Functional outcome scores were reported using the Mayo
Elbow Performance Score (MEPS), Oxford Elbow Score (OES),
and Disabilities of the Arm Shoulder and Hand score (DASH).
Overall MEPS scores improved from 56.3 preoperatively to 93.8
postoperatively, OES from 23.9 to 45.8, and DASH from 31.8 to 1.81.
This study reported improvement in post-operative functional
scores in each scoring system, though there were no significant
difference noted between any of the above outcome scores between
autograft and allograft groups (p>0.05). This study did not report
complication rates, though they did identify calcific deposition in all
grafts, 10 at the humeral insertion and 5 at the ulnar insertion. They
did not report on return to play rates.
A retrospective study by Savoie et al. [8] evaluated functional
outcome scores, return to play rate, range of motion, and
complications at 2 years in 116 patients who underwent ulnar
collateral ligament reconstruction with allograft tendon. Of the
116 patients, gracilis allograft was used in 100 patients, and
semitendinosus allograft was used in 16 patients. Functional
outcome scores were reported with the Conway-Jobe scale. 93
patients reported excellent outcomes (81%), 15 patients reported
good outcomes (13%), 8 patients reported fair outcomes (7%), and
no patient reported poor outcomes. 33 patients (28.4%) returned
to play above preinjury level, 64 (55.1%) returned at preinjury
level, 13 (11.2%) returned below preinjury level, and 6 (5.2%)
did not return to play, 3 of which were for reasons unrelated to
their surgery. Average return to competition was 9.5 months.
Postoperative complications, reported in 7 patients (6%), included
1 ulnar neuropathy, 2 late sensory neuropathy, 2 postoperative
wound issues, 1 medial humeral epicondyle fracture, and 1 flexorpronator
muscle and tendon tear. No graft failures were reported.
Savoie et al concluded that outcomes following reconstruction
with allograft versus autograft were similar in regard to Conway-
Jobe outcome scores, return to play rate, range of motion, and
complication rates.
Discussion
Ulnar collateral ligament tears occur most often in pitchers
and other overhead throwing athletes resulting in instability of the
elbow joint [10]. Reconstruction of the UCL with autograft tendon
has been a mainstay in treatment since the late 1900’s. Although
successful as a treatment for returning elbow stability, the use of
autograft also provides the potential opportunity for donor site
morbidity as well as extended operating room time. Donor site
morbidity ranges from minor symptoms such as donor site pain and numbness, to severe complications, including infection and
damage to surrounding structures. Numbness in the infrapatellar
branch of the saphenous nerve distribution has been reported in
up to 88% of patients who underwent hamstring autograft harvest
[13]. A more severe and detrimental complication of incidental
harvest of the median nerve has also been reported with palmaris
longus tendon autograft harvest [14]. The use of allograft tendon
for UCL reconstruction appears to be an appropriate alternative
for reducing these potential complications that can be seen with
autograft harvesting.
Functional outcomes after UCL injury and surgical repair are
of great interest due to injury often occurring in the workplace. In
previous papers, UCL reconstruction with autograft has resulted in
favorable functional scores and patient satisfaction [1]. In reviewing
the articles discussed here, improvement and good to excellent
functional scores were reported in all patient cohorts regardless of
the score system utilized. The use of allograft versus autograft does
not seem to significantly impact functional outcome, but further
large-scale studies are needed to identify subtle differences in
function.
As UCL injury occurs often in athletes, return to play rates
are of particular interest. Previously published studies on UCL
reconstruction demonstrate favorable return to play rates. In
2015, Erickson et al. [10] performed a systematic review reporting
on return to play rates and functional outcome scores of patients
undergoing UCL. Twenty studies were included reviewing 2,019
elbows that underwent UCL reconstruction. They found an overall
return to play rate at 86.2%. A study by Marshal et al. [3] evaluated 46
major league baseball pitchers who underwent UCL reconstruction
with the use of gracilis or palmaris autograft tendons and did not
determine any significant difference in performance outcomes
between the two patient cohorts [4]. They found an overall return
to play rate of 96%, with 82% returning to play at the previous
MLB level. A larger systematic review and meta-analysis by Peters
et al. [15] found an overall return to play of 90% among all patients
who underwent UCL reconstruction. Interestingly, based on level
of expertise, 78% of Major League Baseball players, 67% of Minor
League Baseball Players, 92% of collegiate players, and 83% of
high school players returned to previous level of play. Erickson et al
reported similar levels of return to play as found in these previous
studies, and also found that 100% of patients who underwent UCL
reconstruction with allograft returned to play at the same level or
higher, although there was no significant difference found due to
the high return to play rate in both groups, and the small population
size [11]. Savoie et al. [8] also demonstrated a high return to play
rate of 83.5% at or above previous level of play. Overall, there is
a high return to play rate utilizing either autograft or allograft for
UCL reconstruction, and further studies are needed to demonstrate
a significant difference.
As with any surgical procedure, identifying and minimizing
postoperative complications is imperative to improving patient
outcomes. Complications following UCL reconstruction have been
reported in as high as 10.4% of patients and include in decreasing
incidence: ulnar neuritis (77%), donor site issues (12.5%), need for
revision UCLR (6.6%), stiffness (2.8%), reactive synovitis (1.4%),
post-operative hematoma (0.9%), ulnar tunnel fracture (0.9%) [10].
A meta-regression and systematic review performed by Somerson
et al. [16] demonstrated a similar overall complication rate of
10.2% with the primary complications being ulnar neurapraxia
developing in 6.7% of all patients. Of interest, they found patients
were more likely to report excellent or good Conway outcome
rating if they did not report an ulnar neurapraxia, demonstrating
that neurapraxia is subjectively related to how patients perceive
their functional outcome. Erickson et al. [11] found that while
there were no differences in complications between the type of
graft used, more complications were identified with the standard
docking technique that the double-docking technique. Interestingly,
allografts were used more often with the double-docking technique,
while hamstring autograft were used primarily with the standard
docking technique. In Savoie et al, the rate of complications was
reported as 6%, though this is a single study and may be the result
of a small patient cohort.8 Further studies with equal technique
distribution and reporting methods are needed to determine if
there is a difference in complication rate and type between allograft
and autograft.
The studies identified by our literature search appear to
demonstrate comparable functional outcomes, return to play rate,
and complication rates with the use of allograft tendon versus
autograft tendon in UCL reconstruction. The main limitation of our
study was the availability of very few comparative studies directly
evaluating autograft versus allograft use in UCL reconstruction.
Those that do exist consist of very small patient cohorts which
limits the possibility of statistical analysis. While there appear
to be trends toward similar, and favorable, outcomes between
the two graft options, the heterogeneity of the studies limit data
extrapolation. Additionally, the studies reviewed were retrospective
in nature, and prospective double-blind control studies are needed
for more substantial data. While these limitations exist, there
appear to be similar outcomes between graft types, and we feel
allograft reconstruction is an appropriate treatment option for UCL
reconstruction.
Conclusion
While there is a paucity of comparative literature regarding the use of allograft versus autograft tendon in UCL reconstruction, there does not appear to be any significant difference in regards to functional scores, return to play rate, or complication rates. Further study into this topic is needed to determine more adequate reliability of our conclusions, although from the available literature it does appear to be an appropriate option while sparing potential complications of donor site morbidity. Overall, allograft reconstruction is an adequate option for ulnar collateral ligament reconstruction.
References
- Waris W (1946) Elbow injuries of javelin-throwers. Acta Chir Scand 93(6): 563-575.
- Petty DH, Andrews JR, Fleisig GS, Cain EL (2004) Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med 32(5): 1158-1164.
- Marshal N, Keller R, Orr L (2019) Major league baseball pitching performance after Tommy John surgery and the effect of tear characteristics, technique, and graft type. Am J Sports Med 47(3): 713-720.
- Regan WD, Korinek SL, Morrey BF, An KN (1991) Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res (271): 170-179.
- Molenaars R, Bekerom M, Eygendaal D (2019) The pathoanatomy of the anterior bundle of the medial ulnar collaterallLigament. J Shoulder Elbow Surg 28: 1497-1504.
- Morrey BF, An KN (1983) Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med 11(5): 315-319.
- Jobe F, Stark H, Lombardo S (1986) Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am 68(8): 1158-1163.
- Savoie F, Morgan C, Yaste J, Hurt J (2013) Medial ulnar collateral ligament reconstruction using hamstring allograft in overhead throwing athletes. J Bone Joint Surg Am 95(12): 1062-1066.
- Moher D, Liberati A, Tezlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyzes: the PRISMA statement. BMJ 339: b2535.
- Erickson B, Chalmers P, Bush-Joseph C (2015) Ulnar collateral ligament reconstruction of the elbow: A systematic review of the literature. Orthop J Sports Med 3(12): 2325967115618914.
- Erickson B, Cvetanovich G, Frank R (2016) Do clinical results and return-to-sport rates after ulnar collateral ligament reconstruction differ based on graft choice and surgical technique. Orthop J Sports Med 4(11): 2325967116670142.
- Merolla G, Del Sordo S, Paladini P, Porcellini G (2014) Elbow ulnar collateral ligament reconstruction: Clinical, radiographic, and ultrasound outcomes at a mean 3- year follow up. Musculoskelet Surg 98 Suppl 1: 87-93.
- Hardy A, Casabianca L, Andrieu K (2017) Complications following harvesting of patellar tendon or hamstring tendon grafts for anterior cruciate ligament reconstruction: Systematic review of literature. Orthop Traumatol Surg Res 103(8S): S245-S248.
- Leslie B, Osterman A, Wolfe S (2017) Inadvertent harvest of the median nerve instead of the palmaris longus tendon. J Bone Joint Surg Am 99(14): 1173-1182.
- Peters S, Bullock G, Goode A (2018) The success of return to sport after ulnar collateral ligament injury in baseball: A systematic review and meta-analysis. J Shoulder Elbow Surg 27(3): 561-571.
- Somerson J, Petersen J, Neradilek M (2018) Complications and outcomes after medial ulnar collateral ligament reconstruction: A meta-regression and systematic review. JBJS Rev 6(5): e4.
© 2021 Amy Singleton BS. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






