- Submissions

Full Text
Orthopedic Research Online Journal
An Audit of Post-Operative Hospital Stay and Complications of THR in a Tertiary Care Hospital
Muhammad Inam1*, Ihsanullah2, Javed Iqbal3, Muhammad Shabir1 and Mian Amjad Ali1
1Department of Orthopedic and Trauma, Medical Teaching Institute, Lady Reading Hospital Peshawar, Pakistan
2District Headquarter Hospital, Pakistan
3Medical Officer, Tehsil Headquarter Hospital, Pakistan
*Corresponding author:Muhammad Inam, Department of Orthopedic and Trauma, Medical Teaching Institute, Lady Reading Hospital Peshawar, Pakistan
Submission: March 12, 2021;Published: March 22, 2021

ISSN: 2576-8875 Volume8 Issue1
Abstract
Objective: The objective of this study is to determine post-operative hospital stay and complications of total hip replacement in a tertiary care hospital.
Material and Method: This Descriptive study was conducted in the Department of Orthopedic and Trauma, Medical Teaching Institute Lady Reading Hospital Peshawar from March 2017 to February 2018 on 39 consecutive patient of age 55 and above with primary osteoarthritis of the hip. In all these patients cemented arthroplasty of the same manufacturer was done through direct lateral approach and patients were mobilized on first post-operative day. Risk Assessment and Prediction Tool (RAPT) Score was calculated pre-operatively for every patient and hospital stay was arranged accordingly to avoid any complications.
Results: Out of thirty-nine patients, 13(33.3%) were female and 26(66.7%) were male. Mean age of the patients was 63.05(Std. Deviation 4.359) with minimum 55 years and maximum 70 years. Left side was affected in 17 (43.6%) patients, while right side was affected in 22(56.4%) patients. Pre-operatively the Risk Assessment and Prediction Tool (RAPT) Score was less than six score in 3(7.7%), score between 6-9 in 16(41.0%) and score more than 9 in 20(51.3%) patients. Average Post-operative hospital stay was 4.28 with minimum of 2days and maximum of 7 days with standard deviation of 1.654. Eleven (28.2%) patients have three days post-operative hospital stay, 8(20.5%) has five days and 7(17.9%) has six days post-operative hospital stay. The calculated predicted value in our study was 97.4%
Conclusion: Preoperative assessment of the patients undergoing Total Hip Replacement not only reduces complication rates but also reduces socioeconomic burden on hospital as well as on patients.
Keywords: Arthroplasty; Assessment; Hip; Hospitalization; Inpatient; Replacement
Introduction
In old age the quality of bone is poor and usually fracture occurs in load bearing areas which is called fragility facture [1]. Not only bone fracture in old age but also the Joints also became weak and painful which’s known as or Osteoarthritis. In both extreme the patient needs some intervention to reduce his pain and make him mobile [2]. If fracture of hip is extracapsular then fixation is needed which may be done by different methods like dynamic hip screw while intracapsular fracture needs some sort of arthroplasty [3]. Arthroplasty may be either hemi or total. It may be either cemented or uncemented. In osteoarthritis of the hip joint the only option that is used worldwide is arthroplasty. Most of the arthroplasty in this part of the world is cemented in old age. Arthroplasty or joint replacement is best option in old age due to fracture neck of femur or osteoarthritis, but it is not free of complications. Patients needs to be educated preoperatively [4]. Lifestyle modification is very important for a successful total hip replacement. If the patient does not follow the instruction it may dislocate. In our part of the world most of the people are uneducated and they dislocate their joint very easily [5]. There is operative option to reduce joint dislocation like approach, dual mobility joint and constrained joint. The surgeon tries to use the best approach to avoid dislocation and are more meticulous about closure of the joint [6]. The dual mobility and constrained joints are expensive, and the patient cannot afford it. So conventional joint is used most of time [7]. If the patients are well determined and follow the instruction, then dislocation changes are negligible [8]. There are certain tools that has to be used preoperatively and score it for prediction of post-operative hospitalization of patients to reduce the complication rate [9]. One of that tools is known as Risk Assessment and Prediction Tool (RAPT) [10,11]. This tool is scored preoperatively to predict any complication and to act accordingly. THR is a major surgery and most of time patient bear all the cost of the implants. Without knowing the tentative complication and hospital cost in terms of hospital stay make a big problem postoperatively for the patient. This study has shown us about the possible complication and hospital stay postoperatively in THR. The objective of this study is to determine post-operative hospital stay and complications of total hip replacement in a tertiary care hospital.
Material and Method
This Descriptive study was conducted in the Department of
Orthopedic and Trauma, Medical Teaching Institute Lady Reading
Hospital Peshawar from March 2017 to February 2018 on 39
consecutive patient of age 55 and above with primary osteoarthritis
of the hip. All those patients of either gender that have primary
osteoarthritis of hip, diagnosed clinically and confirmed by
radiograph of the hip taken in anteroposterior and lateral
projection. Then patients were counseled about the procedure
and postoperative protocol for daily living activities. That patient
who was willing to be put in the study were included in the study
with written informed consent. All the co morbid conditions were
optimized before operation.
Preoperative all the patients were evaluated with Risk
Assessment and Prediction Tool (RAPT) and categorized in high
risk, medium risk and low risk group. RAPT includes age of the
patient, gender, gait aid used, helper needed and living alone or
with others. Total score is 12, if the score is less than six (High
Risk Group) then extended hospitalization is needed, if the score is
between 6 and 9(Medium Risk Group) then rehabilitation is needed
at home while if the score is more than 9(Low Risk Group) then
early discharge without any rehabilitation is need (Figure 1).
Figure 1:

Risk Assessment and Prediction Tool (RAPT) was filled by the
patients, scored and evaluated before surgery to predict the hospitalization
days to avoid postoperative complication. Hip was operated
with direct lateral approach and cemented arthroplasty was
done and the implants used in all cases were from the same manufacturer.
After closure, a pillow was put to the outer side of limb
to avoid external rotation and hip flexion for 24 hours, and prophylactic
intravenous antibiotics were given for five days. Vancomycin
2 grams and Cefoperazone + sulbactum 2 grams were given intra
operatively 20 minutes before giving incision. The same antibiotics
were given for first twenty-four hours and then the vancomycin
was stopped. Anterior posterior and lateral radiograph were taken
to see the position of cup and stem. On first post-operative day the
patient is mobilized by the physiotherapist and walking is allowed
with the help of Zimmer frame to avoid fall. The patients were instructed
to sleep on operated side, use western commode in toilet,
use a stick to avoid fall, use of wall mounted handles in toilets, and
do not flex, abduct or adduct hip more than 900.
All the data collected with the help of a proforma was then put
into the SPSS version 17 and analyzed for frequencies.
Results
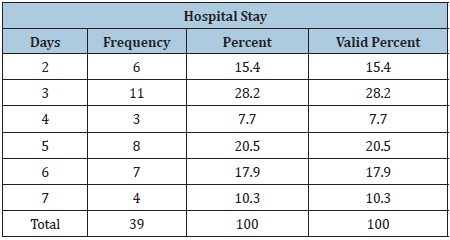
A total of fifty-four patients were included in the study but at final follow up only thirty-nine has been seen. So, we analyzed only those thirty-nine patients for any complication. Out of thirty-nine patients, 13(33.3%) were female and 26(66.7%) were male (Table 1). Mean age of the patients was 63.05(Std. Deviation 4.359) with minimum 55 years and maximum 70 years (Table 2). Left side was affected in 17 (43.6%) patients, while right side was affected in 22(56.4%) patients (Table 3). For ease we have divided the RAPT score into high-risk group (Score less than 6), medium risk group (Score 6-9) and low risk group (Score more than 9). Preoperatively the Risk Assessment and Prediction Tool (RAPT) Score was less than six score in 3(7.7%), score between 6-9 in 16(41.0%) and score more than 9 in 20(51.3%) patients (Table 4). Average post-operative hospital stay was 4.28 with minimum of 2days and maximum of 7 days with standard deviation of 1.654 (Table 2). According to the RAPT score 3(7.7%) needs prolonged hospital stay, 16(41.0%) needed discharge from hospital with rehabilitation at home and 20(51.3%) needed discharge direct to home while post operatively only 2(5.1%) patients has needed prolong stay due to complications. Eleven (28.2%) patients have three days postoperative hospital stay, 8(20.5%) has five days, 7(17.9%) has six days while 4(10.3%) patients have 7 days of post-operative hospital stay (Table 5). There were two cases of surgical site infection. In one patient it was a superficial infection and was treated with injection cefoperazone + sulbactam 2gram intravenously for 14 days and then switched to oral Co-amoxiclav 1 gram twice daily for one month. The other case with infection was managed with debridement and same antibiotics. These two patients had a prolong hospital stay as compare to other. If we put these two cases in high-risk group then the predicted value of RAPT score was 97.4%.
Table 1:
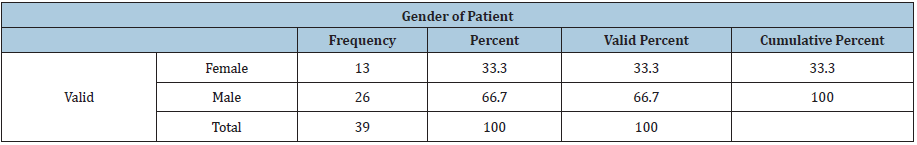
Table 2:
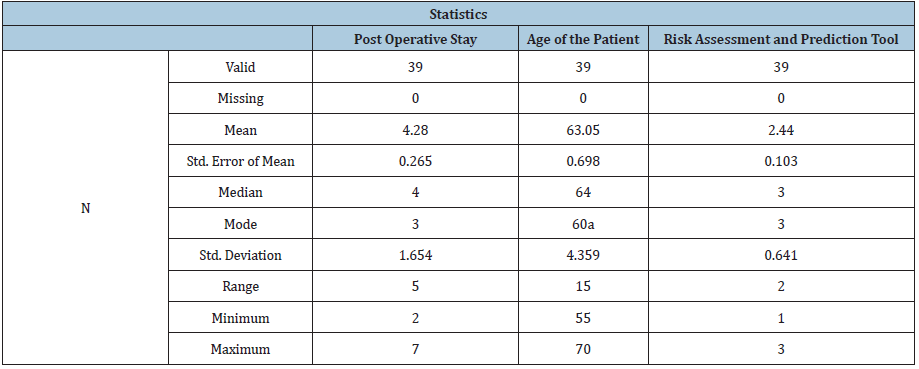
Table 3:
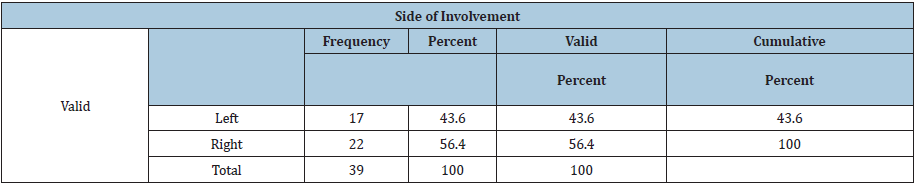
Table 4:
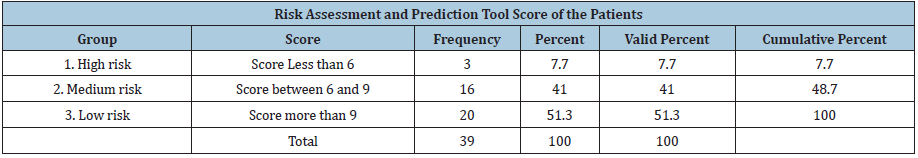
Table 5:
Discussion
Most of the hospital try to reduce the cost of hospital by cutting
short of the hospital stay either preoperative of postoperative
or both. As most of the economic burden is on the patients for
arthroplasties, we have tried to reduce the such cost by reducing
length of hospital stay that not only has helped in economy but
also has minimized complication like cross infection, so we started
using RAPT in our department for hip arthroplasty [3,5-7,10].
Australian orthopedist has originally developed the RAPT
which is aimed to predict discharge of patients in Arthroplasties
preoperatively. This allows the entire caregivers of the department
to optimize the patient’s care according to the needs [11]. A study
done by Abbas et al. [12] has reported complication rate of 19.6%
(39) in which the dislocation was most common13 patients (6.5%),
while infection occurred in 4(2%) of patient that all needed
some intervention. They have not used RAPT that’s why their
complication rate is high. In their study many minor complications
also occurred that were managed conservatively like; surgical site
infection in 2.5%, urinary tract infection in 2.5%, pleural effusion
and pneumonia in 2%, deep venous thrombosis in 0.5% and
myocardial infarction in 0.5%.
Hansen et al. [13] in 2015, studied 3,213 patients with
arthroplasties and showed that RAPT score has an accurate
prediction for patients discharge disposition. He found that there
was 78 % predictive accuracy overall but for hip it was 80%. The
predictive accuracy of RAPT was more than 90% of the score of <6
that has been sent to inpatient rehabilitation center and score >10
that has been sent to home, while it was lowest for scores between 7
and 10 which is almost comparable to our study. On the base of such
finding he categorized his patients into low risk > 10, intermediate
risk 7 to 10 and high risk <7 of RAPT score. In current study high
risk patients were 3(7.7%), intermediate risk was 16(41.0%) and
low risk patients were 20(51.3%).
Bozic et al. [14] has compared the hospital cost for primary
versus revision arthroplasties in term of in hospital stay and
found that revision arthroplasties have higher cost and in patient
stay. In his study the average complication rate was 32% higher
and the average inpatient stay was 16% longer than the primary
arthroplasty. He concludes that preoperative risk assessment
for arthroplasty can minimize higher resource utilization of the
hospital and as well as complication rate.
Bozic et al. [15] studied 7818 patients for discharge to inpatient
rehabilitation center after joint replacement evaluated by RAPT
score. In his study 29% of high-risk patients that have score of
less than six were discharged to inpatient rehabilitation center
after surgery. The patient has high risk and was send to inpatient
rehabilitation center was Old age, higher ASA grade, insured
patients, and female gender. In our study there was only 7.7%
patients that need inpatient rehabilitation.
Another study done by Tan et al. [16] in 2014 on 569 patient
in which he pointed out that RAPT score has high significance
for predicting the hospital stay following arthroplasty
(R=0.24, P <0.001); the shorter inpatient stay has the highest
the RAPT score which is comparable to our study. He found the predictive accuracy of 85% in RAPT score and concluded that those
patients who want to be discharge home has higher RAPT score.
(OR 9.79, 95% CI 5.07 to 18.89, P <0.001). The predictive accuracy
of our study was 97.4 %
Coudeyre et al. [17] studied 134 patients of hip replacement
for predictive outcome of surgery in which it was found that
RAPT score was useful tool in postoperative decision for patient
discharge. The usefulness of preoperative RAPT score in planning
patient care postoperatively has limited value because nearly 50%
of the patients has score of 6 to 9. To increase the accuracy of RAPT
score further study is need for 6-9 (intermediate risk group) [13].
Customs, traditions and values play a big role in medical field
in our set up and most of the patients that were enrolled were
highly cooperative in the postoperative management which has
minimized the complications as compared to other studies. There
are certain limitations in our study. The sample size is small and
only an educated patient who can read and understand the written
precautions were included which means that a great chunk of
patients was excluded from the study as they are only illiterate. The
follow up was very short- and long-term complications were not
evaluated.
Conclusion
Preoperative assessment of the patients undergoing Total Hip Replacement not only reduces complication rates but also reduces socioeconomic burden on hospital as well as on patients. Clinical scoring of a patient that undergo surgery can allow the patient as well as the surgeon to focus on those aspects that need special attention. The preoperative scoring system allows the patients to obtain safe assistance and appropriate care postoperatively.
References
- Benedetti MG, Sarti D, Bonfiglioli Stagni S, Marian E (2015) Setting, clinical pathways, fast-track and rehabilitation following primary knee arthroplasty: a literature review. Open Rehabil J 8: 17-24.
- Monticone M, Ambrosini E, Rocca B, Lorenzon C, Ferrante S, et al. (2014) Task-oriented exercises and early full weight-bearing contribute to improving disability after total hip replacement: A randomized controlled trial. Clin Rehabil 28(7): 658-668.
- Slover J, Mullaly K, Karia R (2017) The use of the risk assessment and prediction tool in surgical patients in a bundled payment program. Int J Surg 38: 119-122.
- Oldmeadow LB, McBurney H, Robertson VJ (2003) Predicting risk of extended inpatient rehabilitation after hip or knee arthroplasty. J Arthroplasty 18(6): 775-779.
- Dauty M, Schmitt X, Menu P, Rousseau B, Dubois C (2012) Using the Risk Assessment and Predictor Tool (RAPT) for patients after total knee replacement surgery. Ann Phys Rehabil Med 55(1): 4-15.
- Oosting E, Hoogeboom TJ, Appelman-de Vries SA, Swets A, Dronkers JJ, et al. (2016) Preoperative prediction of inpatient recovery of function after total hip arthroplasty using performance-based tests: A prospective cohort study. Disabil Rehabil 38(13): 1243-1249.
- Mathias S, Nayak US, Isaacs B (1986) Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil 67(6): 387-389.
- Peters DM, Fritz SL, Krotish DE (2013) Assessing the reliability and validity of a shorter walk test compared with the 10-Meter Walk Test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther 36(1): 24-30.
- Wolters U, Wolf T, Stützer H, Schröder T (1996) ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth 77(2): 217-222.
- Perry M A, Hudson S, Ardis K (2011) If I didn't have anybody, what would I have done?: Experiences of older adults and their discharge home after lower limb orthopaedic surgery. J Rehabil Med 43(10): 916-922.
- Konopka JF, Hansen VJ, Rubash HE, Freiberg AA (2015) Risk assessment tools used to predict outcomes of total hip and total knee arthroplasty. Orthop Clin North Am 46(3): 351-362.
- Abbas K, Murtaza G, Umer M, Rashid H, Qadir I (2012) Complications of total hip replacement. J Coll Phys Surg 22 (9): 575-578.
- Hansen VJ, Gromov K, Lebrun LM, Rubash HE, Malchau H, et al. (2015) Does the risk assessment and prediction tool predict discharge disposition after joint replacement? Clin Orthop Relat Res 473(2): 597-601.
- Bozic KJ, Katz P, Cisternas M, Ono L, Ries MD, Showstack J (2005) Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Joint Surg Am 87(3): 570-576.
- Bozic KJ, Wagie A, Naessens JM, Berry DJ, Rubash HE (2006) Predictors of discharge to an inpatient extended care facility after total hip or knee arthroplasty. J Arthroplasty 21(6 Suppl 2): 151-156.
- Tan C, Loo G, Pua YH, Chong HC, Yeo W, et al. (2014) Predicting discharge outcomes after total knee replacement using the Risk Assessment and Predictor Tool. Physiotherapy 100(2): 176-181.
- Coudeyre E, Eschalier B, Descamps S (2014) Transcultural validation of the Risk Assessment and Predictor Tool (RAPT) to predict discharge outcomes after total hip replacement. Ann Phys Rehabil Med 57(3): 169-184.
© 2021 Muhammad Inam. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






