- Submissions

Full Text
Orthopedic Research Online Journal
Outcomes of Distal 1/3rd Fracture Shaft Femur, Fixed with Retrograde Intra Medulary Nailing: A Short-Term Study
Noor Arshad1, Jibran Bashir2* and Anshu Kumar Anshu3
1Department of Orthopedics, Deen Dayal Upadyay Hospital, New Delhi, India
2Department of Orthopedics, Asian Institute of Medical Sciences, Faridabad Haryana, India
3Department of Orthopedics, Asian Institute of Medical Sciences, Faridabad Haryana, India
*Corresponding author: Jibran Bashir, Department of Orthopedics, Asian Institute of Medical Sciences, Faridabad Haryana, India
Submission: September 21, 2020;Published: October 14, 2020

ISSN: 2576-8875 Volume7 Issue4
Abstract
Background: Fractures of distal femur are complex and nearly all of times a tailored approach is required for these fractures. Over a phase of time variety of approaches and implants have been used for these fractures. The use of retrograde femur nail for fixing femur fracture, by means of entry from inter-condylar notch of femur, is a recognized technique of treatment, but the majority surgeons are concerned of making an entry from the knee joint because of possible complications like knee pain, arthro-fibrosis, infections etc. The aim of this study was to look into its effectiveness in fixation of distal 1/3rd fracture of femur with particular emphasis on the outcome and inherent surgical challenges.
Methods: A prospective study of 45 patients with fracture femur distal one third were treated by retrograde nailing, from Aug 2018 to Aug 2020, after obtaining necessary approval from the Institutional ethical & research committee. All the patients were followed till fracture union and evaluated on the basis of demography, length of healing, complications, and surgical challenges.
Results: We observed that mean age of patients was 46.5 years (18 years to 75 years) where 75% were male and 25% were female. Average duration of healing was 24 weeks (ranging from 10 weeks to 40 weeks) with 100% healing achieved. Mean knee range of motion was 124-degree, rate of knee pain 10%, re-operation rate 2.2%, infection rate 2.2%.
Conclusion: Retrograde femoral nailing is a dependable option to antegrade nailing or plate fixation for diaphyseal fracture distal one third femur, and might be even advantageous when antegrade nail entry is challenging like ipsilateral hip fractures, previous implant in hip & proximal femur, ipsilateral pelvi-acetabular injury, bilateral femoral shaft fracture, floating Knee injuries, poly-trauma and obese patients.
Keywords: Distal femur fractures; Retrograde femoral nailing; Supracondylar nail
Introduction
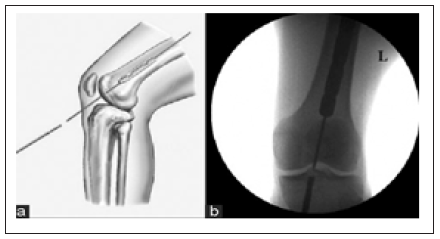
The incidence of distal femur fractures is around 37/100,000 patients per year [1]. Characteristically, two separate mechanisms of injury cause distal femur fractures. In the elder population with osteoporotic bone and susceptible soft tissue envelope, distal femoral fractures occur predominately after low energy trauma, e.g., falls and sprain injuries complicated by a high rate of comorbidity (60% female, older than 60 years). In young patients (60% male, younger than 40 years), high energy trauma causes complex injury with comminuted and open fracture pattern. Approx. 30% of patients with distal femur fractures are poly traumatized. 40% had soft tissue injuries, 10% had ligamentous lesions, 8% had meniscal lesions, 10% had dissected cartilage fragments and 15% had patella fractures and 38% of supracondylar/intercondylar distal femoral fractures have a coronal plane fracture [2-6]. Intramedullary femoral nailing has classically been performed using antegrade entry from piriformis fossa and has produced excellent results. Winquist et al had 99.1% union rate with postoperative knee ROM averaging 130degree and 0.9% infection rate [7]. Since antegrade nail has been so successful there has been resistance in surgeons to accept retrograde nailing as an alternative as shown in Figure 1 & 2; [8].
Retrograde nailing has a benefit over other techniques, viz
Figure 1: X-ray showed traumatic fracture at distal femur.

Figure 2: Postoperative radiographs of a distal third femoral shaft fracture treated with a retrograde interlocking nailing.

- Successful treatment of ipsilateral femur shaft and femoral leg fractures [9].
- In patients with ipsilateral hip acetabular or pelvic fractures most surgeons prefer independent fixation
- of each injury this approach allows for the best possible treatment of each fracture without compromising the surgical approach of other [10].
- Ostrum RF [11] have advocated retrograde femoral nailing to treat bilateral femur fractures, both fractures can be fixed simultaneously on a simple table [11].
- No significant post-operative abductor weakness, no postsurgical hetero-tropic ossification in the region of hip, simultaneous treatment of bilateral lower extremity injuries [12].
- Decreased operative time and decreased positioning time [13-15].
- Since there is no direct radiation to the pelvic region during retrograde nailing, pregnant patients may benefit from this technique [16].
- Gregory et al have demonstrated its usefulness in floating knee injuries by using single incision over patellar tendon [17].
- No risk of pudendal nerve palsy which is as high as 17% in antegrade femoral nailing on a fracture table, less reaming required [18].
- Obese patients can be operated with ease using this technique.
- Patients with unhealthy skin in the region of hip can be considered as a candidate for retrograde nailing.
- Floating knee injury stabilized by retrograde nail and tibia interlocking nail using single incision over patellar tendon.
Lonnel et al. [19] described the use of retrograde nail in a patient with ankylosed hip and stiffed knee with prior history of head injury [19]. The patient had hetereotopic ossification around hip and sustained a femoral shaft fracture after a fall. The presence of heterotopic ossification in the hip region pre-operatively made an antegrade starting portal almost impossible. The authors proceeded with retrograde femoral nailing and obtained good results. Polytrauma patients where a team approach is required with abdominal and thoracic injuries. Team of surgeons can manage injuries simultaneously or sequentially without needing to change operation table. Interventions are accompanied by both benefits and problems. The problem with retrograde nailing is patella-femoral arthrosis, knee stiffness quadriceps atrophy, risk of intra- articular infections, synovial metallosis, and need for orthrotomy for hardware removal [12,20,21]. Technically the proximal locking in retrograde nailing can be demanding as the lateral target device often mismatch in proximal locking due to strong muscle forces. To negotiate this issue new nail designs are considering anterio-posterior free hand locking option for proximal locking.
Methods
A prospective study was done in 45 patients of distal 1/3rd fractures of femur treated by retrograde nailing from Aug 2018 to Aug 2020, after approval from institutional ethical and research committee of the institute. The femoral shaft was separated into 3 equal segments and only fractures of distal third were included. Fractures without involvement of the lower third of the femoral shaft, those with intercondylar extension, grade-III open fractures, and those with an open physeal plate were excluded. All relevant data were collected in a standardised proforma. All the patients were followed till fracture healing (average 24 weeks) and were evaluated on the basis of demography, duration, percentage of healing, complications, range of motion, and surgical challenges. Written informed consent was taken from individual study participants.
Operative procedure
Supine on a radiolucent table. Knee is kept in 20 to 40degree flexion by keeping a bump below the knee.
The entry point for the procedure is in the intercondylar notch 1 finger breadth anterior to the PCL origin.
There are at least 3 ways to approach inter-condylar notch.
- Medial parapatellar arthrotomy-this approach is preferable when there is an intra-articular fracture which requires reduction and fixation.
- Per cutaneous technique (patellar tendon retraction)-an incision about 5-7cm is made from inferior border of patella to superior border of tibial tuberosity. The patellar tendon is retracted laterally and entry point is localized.
- Percutaneous technique (splitting the patellar tendon)-an incision is made from inferior border of patella to the superior border of tibial tuberosity. The patellar tendon is split in the middle and entry point is located.
After locating entry point 2cm anterior to the PCL origin, an awl is kept over it the position of the awl is confirmed by Xray. The awl is advanced into the condylar notch. After which a 7mm entry reamer is introduced in the canal. Once the position in the medullary canal is satisfactory a guide wire is inserted in the medullary canal. Fracture reduction is achieved by traction, closed manipulation, adjustment of the bolster underneath the knee and guide wire negotiated through fracture site. Once the guide wire is in canal gradual reaming is done in increments up to the required diameter. Caution should be taken to avoid fracturing the patella by using tissue protractor and reamer sleeve.
In our study we reamed one size higher (i.e. 10mm for a 9mm nail). We reamed canal only up to desired length of nail to avoid complications of reaming. Once reaming was done, the nail of required length and diameter was introduced. We used nails of a maximum 30cm length and a minimum 15cm length. Hence only those patients which had fracture within 25cm of distal-end of femur were included in this study. Once the nail is introduced, locking was performed using lateral targeting device. The nail had 3 locking options in distal region and two in the proximal. Distal locking bolts were 6.5mm caliber and proximal locking bolt were 5mm. We performed minimum 2 proximal and 2 distal locks. Occasionally one proximal screw was used when nail had at least 10cm of secure intramedullary purchase. Before locking it was always mandatory to confirm that the distal end of nail is buried at least 2mm deep to the subchondral bone.
Postoperative management
Postoperative knee brace was given with gradual knee bending with quadriceps and hamstring streching exercise. Weight bearing was begun as early as possible, depending upon the fracture anatomy, quality of fixation and concomitant injuries. Presence of callus on radiograph helped to decide the ambulation program. Occasionally continuous passive motion programme was initiated to gain the desired range of movement (Figure 3).
Figure 3:
Results
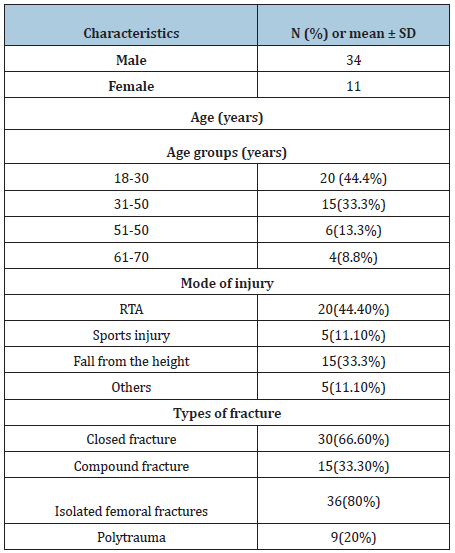
In the present study, out of 45 study subjects there were 20 patients (44.4%) in the age group of 18-30 years, 15 patients (33.3%) were in the age group of 31-50 years, 6 patients (13.3%) were in the age group of 51-60 years, 4 patients (8.8%) in the age group of 61-70 years with mean age of the patients was 44 years. We divided the patients according to the gender where 75% were male and 25% patients were female as given in Table 1. males were more prone to distal femur fracture as they are engaged in various outdoor activities. The mode of injury in most of the patients was RTA (road traffic accident) 20 patients (44.4%). Rest of the patients had: fall from height 15 patients (33.3%), sports injury 5 patients (11.1%) and domestic injury 5 patients (11.1%) as in Table 1 Out of all study participants 30 patients (66.6%) had closed fractures and rest 15 patients (33.3%) had compound fractures as in Table 1. Commination was graded according to the WH classification system.
Mean time from the injury to operation was 3 days. The mean duration of the surgery was 90 minutes. Majority of the patients 36 (80%) had isolated femoral fractures while others 9 patients (20%) had polytrauma as in Table 1. Mean time of the fracture healing was 18.75 weeks [SD ± 7.35]. About 20 patients (44.4%) had healing time of 18 weeks, 9 patients (20%) had healing time of 10 weeks, 8 patients (17.7%) had healing time of 16 weeks, 4 patients (8.8%) had healing time of 24 weeks, 4 patients (8.8%) had healing time of 14weeks.
In the present study we have observed that the post-operative knee range of motion (ROM) achieved;
Table 1: Demographic particulars of the distal 1/3rd fracture shaft femur patients (n=40).
20 patients (44.4%) had 120º,
8 patients (17.7%) had 130º,
12 patients (26.6%) had 125º,
3 patients (6.6%) had 135º,
2 patients (4.4%) had 110º,
and with mean of 124º post-operatively.
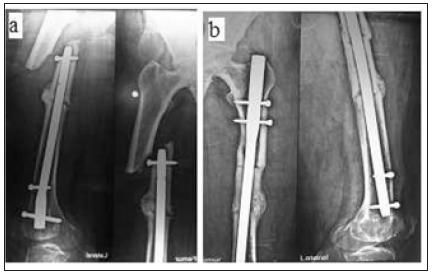
We noticed complication in 4 patients out of which 2 patients had knee joint pain (causes being- nail impingement & iliotibial band irritation by the locking screw), out of these, 1 patient was re-operated, due to impingement of the nail (protrusion of the nail) with the exchange nailing. 1 patient (2.2%) had infection with septic arthritis knee during the treatment as he was a case of compound fracture grade 2 eventually healed with targeted antibiotic but lost knee ROM due to arthrofibrosis. About 11% (5/45) cases developed painful knee and decreased range of motion due to protrusion of nail in intercondylar notch 2 of which had minimal 1or 2 mm protrusion which became asymptomatic with time. One patient developed post operating infection with painful septic arthritis for which through joint lavage and suction irrigation was done and antibiotic according to sensitivity was given which eventually healed but resulted in a stiff knee. One of the patient had stress fracture from the tip of nail, which was managed by exchange by antigrade nailing as in Figure 4a & 4b.
Figure 4a&4b:
Discussion
Faten Hsoumi and Yasmina ELARIBI wrote the manuscript;
Papadokostakis et al. [22] in his metanalysis showed that in patients with distal femoral fractures, the mean time to union and rate of union were 13 weeks and 96.9% respectively.22 The mean ROM of the knee was 104.6 degree. The rates of knee pain, malunion and re-operations were 16.5, 5.2 and 17%, respectively. The overall incidence of infection was 1.1% and for septic arthritis of the knee was 0.18%. Ricci et al. [23] presented a series of 359 femur fractures, 175 treated with antegrade femoral nailing and 166 managed using a retrograde technique [23]. The mal-reduction rate was 0-3% for both groups. They concluded that both antegrade and retrograde rodding can lead to excellent fracture reduction and alignment for femoral mid-shaft fractures. However, retrograde nailing proved to be superior in the reduction and alignment of distal femoral fractures when compared to antegrade nailing. Even treating the implant failure for the femoral shaft distal third fracture retrograde nailing can be a good option as in Figure 5a & 5b.
Figure 5a&5b: Implant failure treated with retrograde nailing successfully.

Tornetta et al. [8] presented a series of 38 antegrade femoral nailings and 31 retrograde nailings [8]. They found no difference in knee or hip range of motion between the groups. However, they had a higher incidence of mal reductions in the retrograde group. They concluded that achieving length and judging rotation is more difficult without a fracture table. Therefore, one should be very cognizant of achieving proper length and rotation when using a retrograde femoral rod. Ostrum et al. [11] presented a series of 100 femur fractures that were treated by either antegrade or retrograde femoral [11]. They found no significant difference in postoperative knee range of motion between the antegrade and retrograde groups. Full ipsilateral knee range of motion was achieved in 63.6% of the antegrade group and in 72.3% of the retrograde group. However, the antegrade group achieved full knee range of motion quicker than the retrograde group, averaging 8.7 weeks versus 14.6 weeks in the retrograde group. The authors concluded that this difference was related to the increased amount of associated knee pathology in the retrograde group preoperatively. The union rate for retrograde nailing was lower in this series, 89% versus 100% for antegrade nailing.
There has constantly been a worry for potential patella-femoral arthritis with an intra-articular entry portal. To date, there has not been enough long-term follow- up to decide whether this should truly be a concern. Some authors have argued that retrograde nailing probably does not lead to significant posttraumatic arthritis because the intercondylar entry point is not in a weight-bearing area and is brought into contact with the patella only in extreme flexion. Moed et al. [16] had 6 patients in their series of fractures that complained of continued knee pain postoperatively [15]. Arthroscopy was performed in three of these patients approximately 6 months after femoral fixation. Arthroscopy revealed no abnormalities except for some scarring in a patient who had a history of an ipsilateral patellar dislocation.
Moed et al. [15] also performed exchange nailing in two of the six patients, allowing close inspection of the knee joint after previous retrograde femoral nail insertion [15]. Inspection of the joint once again revealed no pathologic changes. The inter-condylar entry portal was actually covered by fibrous tissue. Biopsy of this tissue revealed that it was fibrocartilage
In Moed et al. [13-15] second series of 35 femoral shaft fractures treated with retrograde nailing, they exchanged a nail to prevent infection in a quadriplegic patient who developed a decubitus ulcer [14]. Inspection of the joint at that time again showed no intra-articular pathology and an inter-condylar notch portal that was completely covered by fibrous tissue. Postoperative knee stiffness is another potential concern with retrograde femoral nailing. However, several studies have shown that knee range of motion is not adversely affected by this technique. The risk of intraarticular infection and metallosis has also been mentioned in the literature as a potential problem [24]. Ironically, the alternative fixation used for supracondylar femur fractures such as a 95degree screw and side plate, a 95degree blade plate, or a condylar buttress plate is also in an intraarticular location. Therefore, it can be hypothesized that a retrograde rod does not have an increased risk of infection or metallosis when compared to traditional supracondylar femoral fracture fixation, when righty inserted.
The issue of quadriceps atrophy and weakness is another potential pitfall of retrograde nailing. In Moed et al. [14] most recent series, only 2 of 31 ambulatory patients (four patients were nonambulatory secondary to either closed head injury or spinal cord injury) demonstrated mild quadriceps weakness [14]. One of the two patients had a limp with prolonged walking. Both patients were responding to exercise therapy at their latest follow-up. In Herscovici et al. [25] series of 45 fractures, eight patients had decreased strength in the affected leg [25]. Six of these patients had full motor strength but a mild difference that could be appreciated when comparison was made to the unaffected leg. Two of the eight patients lost a full grade of strength. This loss of strength was attributable to reflex sympathetic dystrophy in one patient and to multiple traumatic knee injuries in the other patient. Although loss of quadriceps strength is a concern, the literature reveals that it is usually mild and responsive to exercise therapy. Overall, patients treated with a retrograde technique have a low incidence of limping and pain. Although antegrade nailing has been considered a relatively benign procedure, Bain et al. [26] have shown that it is associated with trochanteric pain, thigh pain, stiffness, abductor weakness, limp, reduced walking distance, and difficulty with stair climbing [26]. Trochanteric pain is the most common complaint.
Conclusion
We established that distal femoral locking nail as a helpful option for the orthopaedic surgeon to deal with distal one third femoral shaft fractures, as it offers advantages over antegrade nailing and plate fixation, in many clinical situations like floating knee, ipsilateral pelvic acetabular injuries, ipsilateral hip arthroplasty or osteosynthesis, and obese patients. It also allows the surgeons to treat bilateral lower extremity injuries (polytrauma) on simple radiolucent operating table by minimizing operative time. The approach to the intercondylar notch can be reached quickly with minimal dissection and can be performed without fracture table. There are few troubles with retrograde nailing like patella-femoral arthritis knee stiffness, quadriceps atrophy, synovial metallosis and intrarticular infections. Although the literature has not shown any increase in these complications by the use of retrograde nailing. By this we conclude that retrograde femoral nailing is an helpful method of treatment of distal one third femur shaft fractures, as an substitute option but should be only after careful patient selection and acquaintance with implant to gain the desired results.
References
- Arneson TJ, Melton LJ, Lewallen DG (1988) Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop 234: 188-194.
- Martinet O (1996) The mechanics of internal fixation of fractures of the distal femur: A comparison of the condylar plate (CP) with the condylar screw (DCS) MD Thesis, University of Zurich, Switzerland.
- Krettek C, Schandelmeier P, Tscherne H (1996) Distal femoral fractures. Unfallchirurg 90: 2.
- Schütz M, Müller M, Krettek C, Hontzsch D, Regazzoni P, et al. (2001) Minimally invasive fracture stabilisation of distal femoral fractures with the LISS: A prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury 32: 48-54.
- Tscherne H, Trentz O (1977) Recent injuries of the femoral condyles. Langenbecks Arch Chir 345: 396-401.
- Hierholzer C, von Rüden C, Pötzel T, Woltmann A, Bühren V (2011) Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: A retrospective analysis. Indian J Orthop 45(3): 243-250.
- Winquist R, Hansen S, Clawson K (1984) Closed intramedullary nailing of femoral fractures. J Bone Joint 66: 529-539.
- Tornetta P 3rd, Tiburzi D (2000) Reamed versus nonreamed anterograde femoral nailing. J Orthop Trauma 14(1): 15-19.
- Swiontkowski MF, Hansen ST Jr, Kellam J (1984) Ipsilateral fractures of the femoral neck and shaft. A treatment protocol. J Bone Joint Surg Am 66(2): 260-268.
- Sanders R, Koval KJ, DiPasquale T, Helfet DL, Frankle M (1993) Retrograde reamed femoral nailing. J Orthop Trauma 7(4): 293-302.
- Ostrum RF, Agarwal A, Lakatos R, Poka A (2000) Prospective comparison of retrograde and antegrade femoral intramedullary nailing. J Orthop Trauma 14(7): 496-501.
- Patterson BM, Routt ML Jr, Benirschke SK, Hansen ST Jr (1995) Retrograde nailing of femoral shaft fractures. J Trauma 38(1): 38-43.
- Moed BR, Watson JT (1995) Retrograde intra- medullary nailing, without reaming, of fractures of the femoral shaft in multiply injured patients. J Bone Joint Surg Am 77(10): 1520-1527.
- Moed BR, Watson JT, Cramer KE, Karges DE, Teefey JS (1998) Unreamed retrograde intramedullary nailing of fractures of the femoral shaft. J Orthop Trauma 12(5): 334-342.
- Moed BR, Watson JT (1999) Retrograde nailing of the femoral shaft. J Am Acad Orthop Surg 7(4): 209-216.
- DeLong WG, Bennett FS (1997) The GSH supracondylar nail. In: Bruce D Browner (Ed.), The Science and Practice of Intramedullary Nailing. (2nd edn), Media, Williams and Wilkins, Philadelphia, PA.
- Gregory P, DiCicco J, Karpik K, DiPasquale T, Herscovici D, Sanders R (1996) Ipsilateral fractures of the femur and tibia: treatment with retrograde femoral nailing and unreamed tibial nailing. J Orthop Trauma 10: 309-316.
- Brumback RJ, Wells JD, Lakatos R, Poka A, Bathon GH, et al. (1990) Heterotopic ossification about the hip after intramedullary nailing for fractures of the femur. J Bone Joint Surg Am 72(7): 1067-1073.
- Lonner BS, Lonner JH, Sadler AH (1995) Retrograde femoral nailing between an ankylosed hip and a stiff knee. J Orthop Trauma 9(3): 266-269.
- Insall JN, Kelly MA (1993) Fractures of femoral condyles. In: Insall JN (Ed.), Surgery of the Knee. Churchill Livingstone, New York, USA, p. 1017.
- Johnson EE, Marroquin CE, Kossovsky N (1993) Synovial metallosis resulting from intraarticular intramedullary nailing of a distal femoral non-union. J Orthop Trauma 7(4): 320-326.
- Papadokostakis G, Papakostidis C, Dimitriou R, Giannoudis PV (2005) The role and efficacy of retrograding nailing for the treatment of diaphyseal and distal femoral fractures: A systematic review of the literature. Injury 36(7): 813-822.
- Ricci WM, Bellabarba C, O’Boyle M (1998) Retrograde vs. antegrade nailing of femoral shaft fractures. Presented at the Orthopaedic Trauma Association Annual Meeting, Vancouver, British Columbia, Canada.
- Janzing HM, Stockman B, Van Damme G, Rommens P, Broos PL (1998) The retrograde intra- medullary nail: Prospective experience in patients older than sixty-five years. J Orthop Trauma 12(5): 330-333.
- Herscovici D Jr, Whiteman KW (1996) Retro- grade nailing of the femur using an intercondylar approach. Clin Orthop Relat Res 332: 98-104.
- Bain GI, Zacest AC, Paterson DC, Middleton J, Pohl AP (1997) Abduction strength following intra- medullary nailing of the femur. J Orthop Trauma 11(2): 93-97.
© 2020 Jibran Bashir. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






