- Submissions

Full Text
Orthopedic Research Online Journal
The Differences in Patient Reported Outcomes/ Experience between Cheilectomy and Fusion of the 1st MTPJ for Hallux Rigidus
Karam Ahmad1* and Anand Pillai2
1 University Hospital of the North Midlands, UK
2 University Hospital of South Manchester, UK
*Corresponding author: Karam Ahmad, University Hospital of the North Midlands, UK
Submission: October 08, 2018;Published: October 29, 2018

ISSN: 2576-8875 Volume4 Issue3
Abstract
Background: Patient reported outcome measures (PROMs) and patient reported experience measures (PREMs) are fundamental to the NHS. We used PROMs2.0, a semi-automated web-based system to assess the patient reported outcomes and experience measures between different operative treatments for hallux rigidus.
Patients and methods: PROMs scores used - EQ-5D VAS and EQ-5D Health Index, and MOxFQ. Data collected pre- post-operatively (follow-up 6 months) PREMs data collected using Picker Patient Experience questionnaire (PPE-15) postoperatively. Average union time- 6weeks. No complications/ infections. No conversions from cheilectomy to fusion.
Results:
Cheilectomy- Average MOxFQ improved- pain: 33.5->25.0 (p=0.084),
walking/standing: 27.6->24.3 (p=0.249),
social interaction: 24.9->21.9(p=0.327).
Average EQ-5D regressed: Index: 0.72->0.70 (p=0.392).
VAS: 86.8->80.4. (p=0.158)
Fusion-Average MOxFQ improved-
pain: 50.7->9.7,walking/standing: 49.1->16.1,
social interaction: 48.4->20.1 (all p< 0.0001)
Average EQ-5D improved: Index:0.68->0.83 (p=0.003).
VAS: 72.5->83.6 (p=0.014)
Fusion outcomes with OA grades- 4/4 patients with grade 2 improved, 11/12 with grade 3. Cheilectomy, 2/2- grade one improved, 3/7 with grade
2 and 0/1 with grade 3. (p< 0.0001). 17 patients (10 fusion/7 cheilectomy) did the PPE-questionnaire. Results show satisfactory experience for both groupsConclusion: Both procedures show improved outcomes. Fusions have greater improvements than cheilectomy. Higher grades of OA do better with fusion.
Introduction
Patient reported outcome measures (PROMs), and patient reported experience measures (PREMs) have been a major part of the 21st century National Health Service (NHS) [1]. Since 2009 it has been a national requirement to collect this data for the Department of Health. This initially started for elective hip and knee procedures [1]. But, has now extended to any form of surgery. This is a change in direction from previous monitoring, where the only outcomes measured were physician based and used mainly for research purposes [1]. The use of PROMs allows us to move towards a more patient centric NHS. Elective foot and ankle surgery and PROMs go hand in hand. The specialty can directly impact mobility and quality of life. Hallux rigidus is a common, painful and quality of life impairing condition. Several conservative and surgical management strategies exist in order to help alleviate symptoms. Two common surgical procedures carried out are cheilectomy and arthrodesis of the 1st metatarsophalangeal joint. Our aim is to establish PROMs and PREMs for these two treatments of hallux rigidus and briefly observe how grades of OA impact PROMs for the two.
Patient and Methods
This is a prospective study looking at all patients who underwent cheilectomy or arthrodesis of the 1st MTPJ. Patients reported their outcomes using a semi-automated email-based system- Amplitude. Patient outcomes were measured using various scoring systems. Firstly, the Manchester- Oxford foot questionnaire, which is a 16- item patient reported outcome-measuring tool. This score has been officially been validated for use in foot and ankle surgery [1].
Secondly, we used the ‘Euroqol research foundation’ derived- EQ-5D index and EQ-5D Visual analogue scale (VAS). EQ-5D-index is a generic 5-item health status measuring tool. Studies have shown the Index score to be suitable for our work, being “sensitive to changes in health status at six months’ [1]. EQ-5D VAS allows a patient to rate their health on a scale from 1-100. 100 being the best they can imagine, 1 being the worst. The overall EQ-5D score allows comparison of health in general, and when used together allow us to assess the change of perceived patient health post-surgery of the foot [1] (Figure 1-3).
Figure 1:Chellectomy Vs Fusion MOXFQ-pre-op vs post-op.
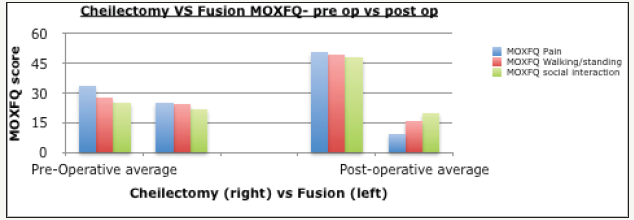
Figure 2:EQ-5D index comparison between chellectomy and fusion.

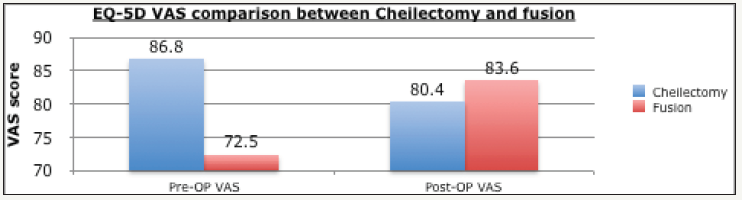
Figure 3:EQ-5D VAS comparison between chellectomy and fusion.
Picker patient experience data (PPE-15) was collected postoperatively. Patients rated their overall experience of being in hospital, ranging from how queries were answered, passing of information, involvement in decision-making, fears, pain, involvement in care and explanation of medicines. This data was collected and overall positive responses per individual domain were summed up to give a picture of how satisfactory experience was in that particular area.
All procedures were part of a single unit series and day case. All procedures were under general anesthesia and antimicrobials according to local policy were given. Rehab was standardized throughout. Weight bearing was allowed post operatively, and all patients were seen at 2 weeks post op for a wound check. At six weeks physiotherapy was commenced for patients, and weight bearing AP, lateral and oblique x-rays were ordered. Statistical tests carried out were done using the program IBM SPSS Statistics, IBM, New York. We assume a p value to be significant when p< 0.05. Use of T-tests ANOVA has been done where appropriate.
Once the data was collated, we stratified according to procedure and looked at radiographs to grade osteoarthritis using Hattrup Johnson classification. For our data, the average union time was 6weeks. There were no complications or infections. No conversions from cheilectomy to fusion took place.
Results
10 patients (4 female and 6 Male) (9 right sided and 1 left sided) had a cheilectomy. 2 were ‘Hattrup and Johnson’ grade one, 7 were grade two, and 1 was grade three. 16 patients (12 female, 4 male) (9 right sided and 7 left sided,) underwent a fusion for the 1st MTPJ. 4 were ‘Hattrup and Johnson’ grade two, and 12 were grade three. Average age for cheilectomy-47.3 (range 34-70), for fusion- 60.3yrs (range 19-83).
Cheilectomy
Table 1:Cheilectomy PROMs-MOxFQ/EQ-5D.
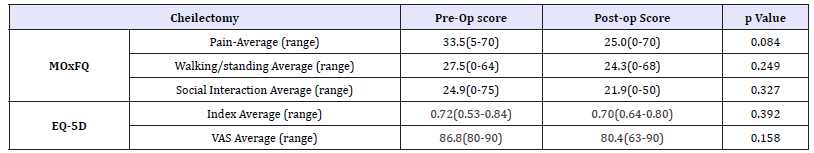
Cheilectomy MOxFQ scores all improved. Pain scored on average 33.5 (range 5-70) pre-operatively, and improved to 25.0 (range 0-70). (p=0.084) Walking/standing outcomes improved from pre-operatively being 27.6 (range 0-64) to 24.3 (range 0-68). (p=0.249) Social interaction also improved from pre-operatively being 24.9 (range 0-75) to 21.9 (range 0-50). (p=0.327) (Table 1 and Figure 1).
EQ-5D scores reduced: with pre-operative index average of 0.72 (range 0.53-0.84) decreasing to 0.70 (range 0.64-0.80). (p=0.392) The pre-operative VAS score average of 86.8 (range 80- 90) decreased to 80.4 (range 63-90). (p=0.158) (Table 1 and Figure 2 & 3)
Arthrodesis
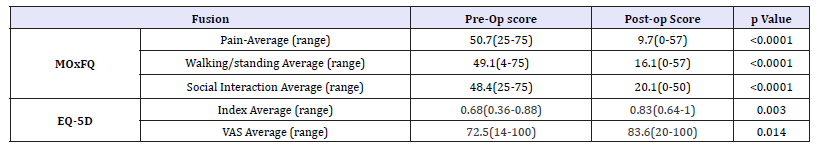
MOxFQ scores all improved. Pain scored on average 50.7 (range 25-75) pre-operatively, and improved to 9.7 (range 0-57). Walking/ standing outcomes improved from pre-operatively being 49.1 (range 4-75) to 16.1 (range 0-57). Social interaction also improved from pre-operatively being 48.4 (range 25-75) to 20.1 (range 0-50). (All p-values< 0.00001) (Table 2 and Figure 2).
EQ-5D scores improved: with pre-operative index average of 0.68 (Range 0.36-0.88) increasing to 0.83 (Range 0.64-1). (p=0.003). The pre-operative VAS score average of 72.5 (Range 14- 100) increased to 83.6 (Range 20-100)). (p=0.0140) (Table 2 and Figure 2 & 3)
Table 2:Fusion PROMs-MOxFQ/EQ-5D.
OA and PROMs
For Cheilectomy, 2/2 (100.0%) patients who had grade 1 OA reported improvements in all three MOxFQ domains. 3/7 (42.9%) of those who had grade 2 reported the same and 0/1 for grade 3. For fusion, 4/4 (100%) patients who had grade 2 OA reported improvements in all MOxFQ domains, and 11/12 (91.7%) for grade 3. (p< 0.00001)
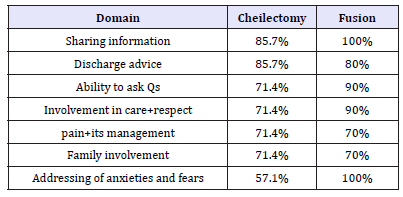
Our patient experience data for cheilectomy showed 6/7 (85.7%) patients were satisfied with the sharing of information and discharge advice. 5/7 (71.4%) with ability to ask questions, involvement in care/respect, pain and its management, and family involvement. 4/7 (57.1%) were satisfied with how their anxieties and fears were addressed. Our fusion data show that 7/10 (70%) patients were satisfied with pain and its management, and the opportunity to involve family. 8/10 (80%) with the discharge advice received. 9/10 (90%) with ability to ask questions, involvement in care and respect. 10/10 (100%) with sharing of information and addressing of anxiety/fears. (p=0.394) (Table 3).
Table 3:PREMs-cheilectomy vs fusion.
Discussion
PROMs have changed the way in which healthcare professions judge the standards of the care they provide. They were developed in 2009 [1], as part of a department of health initiative. Their use becomes especially important where survival is not as important as is quality of life [1]. This makes the use of PROMs in Hallux rigidus surgery especially useful, as the changes in quality of life post operatively are well known to be an important prognostic indicator to a satisfied patient. There have been countless studies looking at PROMs for hip and knee arthroplasty, and factors, which can influence them such as, implant brands and types of hospital [1].
Our data suggests that fusion leads to a statistically significant improvement in PROMs when compared to cheilectomy. We saw improvements in all three domains of MOxFQ for both. But the cheilectomy improvements were not significant. For individual aspects of EQ-5D, we saw varying results for the two procedures; Fusions reported an increase in VAS by 11.1, statistically significant. Whereas there was a decline in VAS for cheilectomy, by a score of 6.4. This however was not statistically significant. Index scores showed similar outcomes, fusion improving significantly, and cheilectomy decreasing but not to a significant extent. EQ-5D scores are in line with current literature covering most orthopaedic surgeries in that they show improvement albeit not always significant [1-4]. At this stage it would be prudent to not read too much in to the VAS scores, sources suggest that the EQ-5D VAS is not as sensitive as the MOxFQ and EQ-5D Index score in measuring health changes post operatively [5].
One meta-analysis concluded that at this point there was no significant way to measure outcomes from either procedure but did point favourably towards arthrodesis over cheilectomy in general [1,2]. When looking at objective outcomes for treatment of hallux rigidus, other studies have found that fusion is superior to cheilectomy [3-9]. This once again correlates with our patient reported outcomes data. Reasons for arthrodesis doing better than cheilectomy may be due to the relatively later stage at which arthrodesis is done. Whilst cheilectomy is a joint preserving operative treatment, arthrodesis is purely for symptomatic relief. Patients who undergo arthrodesis generally have severe hallux rigidus, and therefore the potential for improvement from the procedure is much greater than a mild patient undergoing cheilectomy. This may explain why the PROMs for arthrodesis are better than cheilectomy [10,11].
Results
Results with regard to grade of OA, show that patients with fusions show better outcomes with higher grades of (Hattrup & Johnson classified) OA, whereas cheilectomy patients show better outcomes with lower grades. This data was statistically significant and in line with what literature has suggested, one study found that for low grade OA, cheilectomy was a satisfactory procedure on a radiograph basis, especially for grade 1,2 and some grade 3. Arthrodesis was better for more severe cases, such as grade 3 with < 50% of metatarsal cartilage head remaining, and grade 4 However, despite this, greater patient numbers, and further study are still required.
PREMs data shows that overall experience is better in fusion cases. It was higher in 4 of the 7 domains (asking questions, sharing information, involvement in care/respect and addressing anxiety and fears), the same in one (pain and management), and slightly lower in two (family involvement and discharge advice). The results are not statistically significant, but the trends suggest fusion has better PREMs, a reason for this may stem from the fact fusion is generally an end stage option. I.e. patients are more likely to have an improvement, as their initial condition was so bad in the first place.
Conclusions
Fusion of the 1st MTPJ shows better patient reported outcomes when compared to cheilectomy for hallux rigidus. It also shows better outcomes with high grades of osteoarthritis, whilst cheilectomy shows better outcomes for lower grades of OA. Further study is required to confirm this.
References
- NHS UK (2014) Monthly patient reported outcome measures (PROMs) in England a guide to PROMs methodology, UK.
- Judge A, Arden NK, Kiran A (2012) Interpretation of patient-reported outcomes for hip and knee replacement surgery: identification of thresholds associated with satisfaction with surgery. J Bone Joint Surg B 94(3): 412-418.
- Schrier JC, Palmen LN, Verheyen CC, Jansen J, Koëter S (2015) Patientreported outcome measures in hallux valgus surgery. A review of literature. Foot Ankle Surg 21(1): 11-15.
- Dawson J, Boller I, Doll H (2011) The MOXFQ patient-reported questionnaire: assessment of data quality, reliability and validity in relation to foot and ankle surgery. Foot (Edinb) 21(2): 92-102.
- Maher AJ, Kilmartin TE (2012) An analysis of Euroqol EQ-5D and Manchester oxford foot questionnaire scores six months following podiatric surgery. J Foot Ankle Res 5(1):17.
- Dawson J, Coffey J, Doll H, Lavis G, Cooke P, et al. (2006) A patient-based questionnaire to assess outcomes of foot surgery: validation in the context of surgery for hallux valgus. Qual Life Res 15(7): 1211-1222.
- Deshpande PR, Rajan S, Sudeepthi BL, Abdul nazir CP (2011) Patientreported outcomes: A new era in clinical research. Perspect Clin Res 2(4):137-144.
- Baker PN, Deehan DJ, Lees D (2012) The effect of surgical factors on early patient-reported outcome measures (PROMS) following total knee replacement. J Bone Joint Surg Br 94(8): 1058-1066.
- Jansson KÅ, Granath F (2011) Health-related quality of life (EQ-5D) before and after orthopedic surgery. Acta Orthop 82(1): 82-89.
- Mcneil DS, Baumhauer JF, Glazebrook MA (2013) Evidence-based analysis of the efficacy for operative treatment of hallux rigidus. Foot Ankle Int 34(1): 15-32.
- Coughlin MJ, Shurnas PS (2003) Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am 85-A(11): 2072- 2088.
© 2018 Karam Ahmad. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






