- Submissions

Full Text
Orthopedic Research Online Journal
Evaluating the Effectiveness of Treatment Options for Pain: Literature Review
Joseph Jacobs1*, Madison Sielski2, Tiffany Jones3, Henry Huynh4, Mario Victoria5, Cameron Miles6, Lora Reed7,Kaitlin Mooneyham8 and Ivy Nguye9
1 Doctor of Physical Therapy, University of St. Augustine for Health Sciences, USA
2 Department of Kinesiology, Chapman University, USA
3 Department of Community Health Sciences, University of Nevada, USA
4 Department of Sociology, University of California, USA
5 Department of Kinesiology, California State University, USA
6 Department of Kinesiology, Mt. San Antonio College, USA
7 Department of Kinesiology, Orange Coast College, USA
8 Department of Kinesiology, California State Polytechnic University, USA
9 Department of Biology, University of California, USA
*Corresponding author: Joseph Jacobs, Doctor of Physical Therapy, University of St. Augustine for Health Sciences, Inventor of ASTR, 26895 Aliso Creek Rd. Suite B270 Aliso Viejo, CA 92656, USA
Submission: June 26, 2018; Published: July 25, 2018

ISSN: 2576-8875 Volume3 Issue5
Abstract
Objectives: This literature review assesses the short and long term effectiveness for chronic pain management of single modality treatment approaches such as opioid use, non-steroidal anti-inflammatory drugs, massage therapy, manual therapy (soft tissue mobilization), instrument assisted soft tissue mobilization, myofascial release, acupuncture, soft tissue release, dry needle, trigger point injection, joint manipulation/joint mobilization, active release technique, strain counter strain, craniosacral therapy, stretching/exercise, McKenzie method, and kinesio taping in comparison to treatment methods that follow the biopsychosocial model such as the multidisciplinary approach, cognitive behavioral rehabilitation and Advanced Soft Tissue Release.
Methods: A comprehensive literature search was conducted in major search databases including Medline, ScienceDirect, Pubmed, Embase, Google Scholar, Cinahl, BioMed Central, and Cochrane. 16,145 articles were found. Studies that met the inclusion criteria included systematic reviews and metaanalyses evaluating the treatment options for musculoskeletal pain.
Results: 57 studies met the criteria of this study, with 50 being systematic reviews, 4 randomized controlled trials (RCT), 1 non-RCT, and 2 literature reviews. The single modality studies were 47 studies, totalled as 53 individual different findings because some studies evaluated several single modalities in the same study. The findings of the 47 studies were consistent regarding that the single modalities provided short term pain reduction or no pain reduction. The biopsychosocial model studies were 7 systematic reviews, 1 literature review, 1 cohort study that consistently showed long term pain reduction, improved range of motion, and improvement in functional activities.
Conclusion: Based on the studies evaluated, treatment methods following the biopsychosocial model seem to yield long term pain reduction, increased range of motion, and improvement in functional activities. On the other hand the single modality treatment methods seemed to yield either short term pain reduction or no pain reduction.
Abbreviations:ART: Active Release Technique; ASTR: Advanced Soft Tissue Release; IASTM: Instrument Assisted Soft Tissue Mobilization; IRB: Institutional Review Board; KT: Kinesio Tape; MCE: Motor Control Exercise; MTrP: Myofascial Trigger Points; NSAIDs: Non-Steroidal Anti-Inflammatory Drugs; NSCLBP: Non-Specific Chronic Low Back Pain; OT: Occupational Therapy; RCT: Randomized Control Trials; ROM: Range of Motion; SCS: Strain Counter Strain; SMFR: Self-Myofascial Release
Introduction
Chronic pain affects a vast majority of the population. It carries the potential to be highly debilitating and can restrict some from performing normal daily activities, such as working. In fact, the National Institute of Health found that about 100 million Americans are affected by chronic pain, and a quarter of that number experience diminished quality of life and restricted activity due to moderate to severe chronic pain [1]. There are many ways to treat chronic pain, and these modes of treatment usually fall into one of two categories: single discipline approaches and multidiscipline approaches. Examples of single discipline approaches include opioid use, massage therapy, manual therapy, acupuncture, spine manipulation, stretching and exercises, dry needle, trigger points injection, and use of Kinesio Tape and other specialized instruments.
A multidiscipline approach, or a biopsychosocial approach, includes analyzing all aspects of a patient’s health which include biological, psychological, and social aspects. 3 Examples of biopsychosocial approaches in treating chronic pain include cognitive-behavioral rehabilitation, multidisciplinary approach, and Advanced Soft Tissue Release, or ASTR. Considering the two different approaches to chronic pain, single discipline and multidiscipline/biopsychosocial, the goal is to determine if one is more effective than the other.
Method
A literature search of several databases was conducted from February 2017 until January 2018. We used a range of sources to identify relevant literature. A comprehensive literature search was conducted in major search databases including Medline, ScienceDirect, PubMed, Embase, Google scholar, Cinahl, BioMed Central and Cochrane. Five reviewers searched the database to determine studies that met the inclusion criteria. The remaining reviewers collected and analyzed data from the selected studies. Studies that met the inclusion criteria included systematic reviews, meta-analyses and literature reviews for treatment options for musculoskeletal pain. There was no limitation for age group or type of musculoskeletal injury. Search words in the title area included acupuncture, dry needle and trigger points, exercise, stretching instrument assisted soft tissue mobilization, soft tissue release, joint manipulation and mobilization, kinesio taping, manual therapy, massage, myofascial release, Active Release Technique (ART), Strain Counterstrain (SCS), craniosacral therapy, McKenzie method, NSAIDs, opioids, trigger point injections, biopsychosocial, multidisciplinary, and systematic review. If systematic reviews were not found for the topic, randomized controlled trials and cohort studies were included. Exclusion criteria included case reports and commentary articles, treatments for cancer, neurological diseases such as cerebral palsy, stroke, Parkinson’s disease, organ pain, or organ transplant, and studies conducted on post surgical patients. In addition, if a systematic review covering the topic was identified through research individual studies pertaining to that particular topic were disregarded.
Discussion
Single medical model
Opioid use: The use of opioids to treat chronic pain has increased in the last few decades. It is estimated that 5 to 8 million Americans currently use opioids to treat their chronic pain.3 There is an increasing number of opioid misuse, ranging from 76 million in 1991 to 219 million in 2011. The Centers for Disease Control found several statistics pertaining to increasing opioid abuse, including the number of those admitted due to addiction to prescribed opioids. Between 2000 and 2010, that number increased from about 40,000 people to over 160,000 people [1]. In 2015, there were 52,404 drug overdose deaths in the United States; of those, 20,101 deaths were related to prescription pain relievers, and 12,990 deaths were related to heroine [2]. 1 of out of every 8 deaths for those aged 25 to 34 in 2010 was related to opioid use [1]. In the state of Georgia alone, the number of deaths related to drug overdoses surpassed the number of deaths due to motor vehicle crashes in 2014 [3]. While many patients, providers, and advocates agree that opioids can be an effective way of managing chronic pain in a certain subset of patients, the potential adverse reactions have become an increasing threat.
According to the National Institute of Health, there is lacking research pertaining to the long-term effects of opioid use on pain or functioning in patients who used opioids in the long term (defined as daily or near daily use for two months or more) [4]. Some observational studies found that patients who use opioids and patients who are on a higher dose of opioids have lower functional status and lower quality of life than patients who do not use opioids and patients who are on a lower dose of opioids. Also, patients receiving rehabilitation services withdrawn from opioids show improved function and improved pain. Even with a large amount of research on the positive effect of opioids on short-term pain, the lack of research on long-term effects of opioids on pain, in addition to the overwhelming evidence of adverse effects of opioid use, makes the controversial topic more ambiguous. Long-term opioid use for chronic pain may not be a fool proof way of managing pain.
Clinical trials performed by Xue et al. [5] on 316 patients have shown no evidence that opioid medication provides long-term beneficial effects for chronic musculoskeletal pain, as it is associated more with severe adverse events, such as nausea, constipation, hyperalgesia, and drowsiness [6]. These effects of opioids might hinder and prevent patients from participating in more effective management programs [6]. The use of opioids as a means to reduce pain has been proven effective, although only in short term pain relief. For long term pain relief, randomized controlled trials (RCT) have proven that opioid use is ineffective.
Non-steroidal anti-inflammatory drugs (NSAIDS): For many patients and providers, the use of NSAIDs, for pain reduction is a common option. In a sys-tematic review of the efficacy of NSAIDs on spinal pain, 35 trials were evaluated [7]. While NSAIDs were proven effective for short term spinal pain reduction, the results in comparison to the placebo groups were not clinically significant. It was concluded that a simple analgesic is necessary for spinal pain since there is not one currently available that has been proven effective for long term pain.
The effect of NSAIDs on pain reduction is temporary, and comes with possible adverse outcomes. For example, a systematic review by Varas-Lorenzo et al. [8] showed that current use of rofecoxib and diclofenac may increase risk of ischemic stroke [9]. However, the research only focuses on these two types of NSAIDs, and more research is necessary to analyze other NSAIDs, as well as the dose/ duration of NSAIDs that increase risk of stroke and subtypes of stroke. The use of NSAIDs as a means to reduce pain has been shown to be ineffective, as systematic reviews demonstrates that this method only temporarily reduces pain.
Massage therapy: Massage therapy is a common method used to reduce pain and relieve muscle tension. A 2015 systematic review by Bervoets et al. [10] looked at the efficacy of massage therapy for treating chronic pain in 26 randomized trials of 2,565 participants. Researchers found that massage therapy alone was more effective in reducing pain and improving function in comparison to no treatment at all. However, massage therapy was not as effective in reducing pain and improving some musculoskeletal conditions in comparison to other active treatments [10]. A systematic review by Chou et al. [11] analyzed 9 trials that researched massage therapy. One of the trials found small effects on the Roland Morris Disability Questionnaire after massage therapy, while most trials saw no difference in reported pain and function after massage therapy. Most trials found increased efficacy of massage therapy on shortterm pain, but not long-term.
Another systematic review by Furlan et al. [12] studied the effectiveness of massage therapy on low back and neck pain. The results found that subjects with nonspecific acute/sub-acute pain receiving massage exhibited significantly reduced pain intensity and disability compared to no treatment or placebo immediately or short-term after the end of treatment. They also found that massage therapy, compared to no treatment, significantly improved pain intensity but not range of motion in subjects with chronic or unknown duration of nonspecific pain, immediately after the end of treatment [13]. Massage therapy have been proven to be more effective in reducing pain compared to not receiving treatments at all, however, systematic reviews have illustrated that the effectiveness of this method has no long-term pain reduction.
Manual therapy-soft tissue mobilization: Manual therapy seems to yield short-term results in regards to pain reduction. According to a 2010 systematic review by Miller et al. [14], 17 controlled randomized trials looked at the efficacy of exercise and manual therapy on neck pain. These trials found no longterm difference for (sub) acute/chronic neck pain with or without cervicogenic headaches.
Another systematic review by Penas et al. [15] studied the effectiveness of manual therapy in treating myofascial trigger points (MTrP) [16]. Results did not produce any rigorous evidence that some manual therapies have an effect beyond placebo in treatment of myofascial trigger points. Controlled trials are needed to investigate whether manual therapy has an effect beyond placebo on MTrP management [16]. Manual therapy does produce shortterm pain reduction and improves range of motion. However, these systematic reviews indicate that there is a lack of evidence to prove that this method has any actual lon term benefits.
Instrument assisted soft tissue mobilization (IASTM): Specially designed instruments can aide in the restoration of muscle pain, decreased mobility, and myofascial restrictions [17]. A systematic review of 7 randomized control trials by Cheatham et al. [17] looked at the efficacy of IASTM. This review found that there was insignificant evidence that IASTM was beneficial for treating musculoskeletal pathology, although some evidence showed increased short-term joint range of motion. The use of instruments yields positive increases in range of motions temporarily, but according to this systematic review there lacks evidence if this method has long-term effects.
Myofascial release: Self-myofascial release (SMFR) is a popular method used to enhance a client’s myofascial mobility [18]. Some of the common tools used in this method are the foam roll and foam roller massage. A systematic review by Cheatham et al. included 14 different articles meeting the inclusion criteria, with a total of 260 healthy subjects, (Male=179, Female=81). The average age of the subjects was 19.6 years, with their ages ranging from 15- 34 years old. Cheatham et al. [17] reviewed studies that examined subjects using the foam roller, which were hip range of motion (ROM), foam rolling sit and reach, knee ROM, and ankle ROM [18]. 5 studies used the roller massage which was ankle ROM, knee ROM, hip ROM, and roller massage sit and reach. Researchers found that SMFR with a foam roller or roller massage can have short term effects on increasing the joint ROM without negatively affecting muscle performance. In addition, researchers found that SMFR can help after intense exercise, as it can help attenuate decrements in muscle performance and delayed onset of muscle soreness but there is currently not enough high quality evidence to draw any firm conclusions.
In the systematic review by Beardsley et al. [19], researchers assessed studies on acute and chronic clinical effects of SMFR. Researchers concluded that SMFR increases flexibility and reduces muscle soreness and does not hinder athletic performance. It can also improve arterial function, vascular endothelial function, and increase parasympathetic nervous system activity, all factors of which may be useful in recovery but there is conflicting evidence whether SMFR can improve flexibility long-term.
The systematic review by Ajimsha et al. [20] included 19 randomized controlled trials assessing the effectiveness of myofascial release [21,22]. Researchers concluded that myofascial release may be useful alone or in conjunction with other therapies and that treatment effects seemed to be retained. Upon further investigation of the specific article reviewed, it was discovered that 11 of the 19 systematic reviews suggested that lack of follow up or use of only immediate follow up measurements may have been limitations to the studies. This makes it difficult to assess the longterm effects of myofascial release. In addition, one of the studies that supported the long-term effectiveness of myofascial release was actually a multimodal treatment method including myofascial release, indicating that this treatment followed the biopsychosocial model. Due to insufficient follow up in 11 of 19 of the studies, the suggestion that treatment effects are maintained may not be supported. Myofascial release has been proven to be effective in increasing range of motion and reducing pain temporarily without hindering performance, however, numerous systematic reviews show that myofascial release alone does not yield any long-term effects.
Acupuncture: Acupuncture is an unorthodox approach towards relieving muscle pain; however, the practice does not provide any clear clinical effectiveness as a treatment. A systematic review of 63 randomized controlled trials, including 6382 individuals by Yuan et al. [23], assessed the effectiveness of acupuncture techniques for musculoskeletal pain [23]. Researchers found that acupuncture alleviated pain at about 12-point on the 100mm visual analogue scale, demonstrating low-quality evidence of acupuncture’s effectiveness in terms of musculoskeletal pain.
In their systematic review of 13 trials with 3025 participants, Madsen et al. [22] studied the effectiveness of acupuncture by assessing the differences present between participants who received acupuncture, placebo acupuncture, and no acupuncture. Treatment was given to patients on a range between 1 day and 12 weeks and pain conditions included knee osteoarthritis, tension headaches migraine, low back pain, fibromyalgia, abdominal scar pain, postoperative pain, and pain during colonoscopy procedure [22]. While there was a moderate difference between placebo acupuncture and no acupuncture groups, there was a small difference between acupuncture and placebo acupuncture groups. A conclusion of the study is that there is a small analgesic effect of acupuncture that seems to lack clinical relevance and cannot be clearly distinguished from bias.
Another systematic review of 21 trials by Andrea Furlan compared acupuncture, no treatment, sham acupuncture, and other therapies to assess the effectiveness of acupuncture for treating chronic low-back pain [24]. Results showed that while acupuncture seemed more sufficient than no treatment, acupuncture was not any more effective than other treatments. Another study by Furlan et al. [24] looked at the effectiveness of acupuncture in treating neck pain [13]. There were inconsistent results for immediate or short-term post-treatment pain intensity between acupuncture and pain medication groups of subjects. Acupuncture did not differ from standard mobilization and traction techniques or laser therapy in short-term post-treatment pain intensity or disability. Immediate/short-term post-treatment pain and disability were better in manipulation than acupuncture groups.
A systematic review by Chou et al, studied the effectiveness of acupuncture in treating back pain [11]. The study evaluated 49 trials, but only included 11 for acute or sub acute back pain. The studies found that for acute low back pain, acupuncture decreased pain intensity more than sham acupuncture with non-penetrating needles. The studies also concluded that acupuncture had no clear effects on function. Several of these systematic reviews indicate that acupuncture is insignificantly more effective compared to its placebo counterparts; yielding short-term pain reduction, with no long-term benefits whatsoever.
1.1.1. Dry needle: Dry needling is used for management of a variety of neuromusculoskeletal pain syndromes by treating muscles, ligaments, tendons, scar tissue, subcutaneous fascia, peripheral nerves, and neurovascular bundles [25]. Dry needling is defined as the penetration of a solid needle through the skin without the introduction of any drug to stimulate trigger points and connective tissue for the management of neuromusculoskeletal pain [26]. In a systematic review, Morihisa et al. [27] analyzed the effectiveness of dry needling for the reduction of symptoms associated with muscular trigger points. Based on chosen criteria, of 2,232 potential studies screened for eligibility, only 6 were identified for inclusion. The review suggests that dry needling is effective in reducing pain associated with lower quarter trigger points in the short-term, however it does not have a positive effect on function, quality of life, depression, range of motion, or strength.
A systematic review of 13 studies, including a total of 723 participants by Gattie et al. [25], assessed the effectiveness of dry needling for musculoskeletal conditions in a 12-week followup period [28]. Evidence of low-quality to moderate-quality suggests dry needling performed by physical therapists is more effective when compared to no treatment, sham dry needling, and other treatments for reducing pain and improving pressure pain threshold. Evidence showed a small but significant effect of dry needling for improving functional outcomes when compared to no treatment or sham needling. The long-term benefits of dry needling are currently lacking supporting evidence.
In a systematic review, Cotchett et al. [6] evaluated the effectiveness of dry needling and/or injections of myofascial trigger points associated with plantar heel pain [29]. Of the 342 studies identified, only 3 quasi-experimental studies fulfilled the inclusion criteria. Plantar heel pain is one of the most common musculoskeletal pathologies of the foot, estimating to affect 10% of the population at some time in their life. The findings of the studies were combined using a narrative rather than a quantitative approach, noting poor methodological quality and secondary outcome measures. The review suggests limited evidence for the effectiveness of dry needling and/or injections of myofascial trigger points associated with plantar heel pain, due to the poor quality and heterogeneous nature of the included studies.
A literature review by Dunning et al. [26] suggests that although there are several studies which have demonstrated immediate or short-term improvements in pain and/or disability by targeting trigger points; however, there are no high-quality long-term trials supporting dry needle techniques at exclusively muscular trigger points [25]. Overall, dry needling has been beneficial for reducing pain short-term, but there is poor evidence to support long-term effectiveness.
A systematic review of 15 studies by Espejo et al. [30] evaluated the effectiveness of dry needle treatment for myofascial trigger points compared to other interventions such as oral drugs, acupuncture, and placebo [31]. Although there is evidence that implies dry needling may have a positive short-term effect on pain and mobility in comparison to the placebo, there are no demonstrations of long-term effects. Further randomized clinical trials must be conducted using dry needling to determine the effectiveness of this application. Multiple systematic reviews indicate that dry needling is proven effective in reducing pain temporarily, but there is lacking evidence on whether or not this method yields long-term pain relief.
Trigger point injection: Myofascial trigger point pain is defined as pain arising from one or more myofascial trigger points, which are hyperirritable spots in the skeletal muscle that are associated with hypersensitive palpable nodules in taut bands [27]. A systematic review by Cummings and White assessed the effectiveness of trigger point injection therapy for myofascial pain. The systematic review included a total of 23 randomized controlled trials in which all tested needle therapy to relieve myofascial pain. While the needling was effective, the positive effect of the therapy was more likely attributed to the needle of the placebo, not the drug injected. There was no pain improvement between direct needling or placebo.
Scott et al. [32] studied the effectiveness of trigger point injections for chronic nonmalignant musculoskeletal pain in their systematic review. Participants’ pain must have lasted more than 3 months to be included in the study. 15 randomized controlled trials were included for the purpose of the study. Researchers found no evidence supporting the effectiveness or ineffectiveness of trigger point injections [33].
In a systematic review, Cotchett et al. [6] evaluated the effectiveness of dry needling and/or injections of myofascial trigger points associated with plantar heel pain [29]. Of the 342 studies identified, only 3 quasi-experimental studies fulfilled the inclusion criteria. Plantar heel pain is one of the most common musculoskeletal pathologies of the foot, estimating to affect 10% of the population at some time in their life. The findings of the studies were combined using a narrative rather than a quantitative approach, noting poor methodological quality and secondary outcome measures. The review suggests limited evidence for the effectiveness of dry needling and/or injections of myofascial trigger points associated with plantar heel pain, due to the poor quality and heterogeneous nature of the included studies. In regards to pain relief, the systematic reviews assessed seem to lack evidence for the effectiveness of trigger point injection therapy.
Joint manipulation-joint mobilization: Joint mobilization is used in restoring decreased mobility. However, this method may not be as effective as perceived. A systematic review by Rubinstein et al. [28] researched the effectiveness of spinal manipulation therapy for those suffering from chronic lower back pain [34]. This study assessed 26 randomized controlled trials including 6070 participants. Evidence showed no significant difference between spinal manipulation therapy and other intervention approaches.
A systematic review by Young et al. [35], which included 5 studies meeting the criteria, observed the effectiveness of thoracic manipulation for mechanical neck pain [32]. The researchers found no definitive clinical evidence supporting thoracic manipulation’s efficacy. The method did, however, yield short-term effects in improving neck pain and the range of motion. However, further research is required to determine if this method produces longterm effects on relieving mechanical neck pain.
A systematic review published by Canter and Ernst studied the effectiveness of spinal manipulation for treatment of multiple regions of pain, including, but not limited to, back and neck pain. 16 trials were included for the purpose of this study. Evidence suggested that spinal manipulation was ineffective for all evaluated forms of pain [5].
A systematic review published by Furlan et al. [12] studied the effectiveness of joint manipulation in treating low back and neck pain [13]. The studies found no significant difference between manipulation and placebo in post-treatment pain, medication intake, disability, or back flexibility. Results from studies comparing manipulation to massage or physiotherapy in improving posttreatment pain intensity or mobility were inconsistent, either in favor of manipulation or indicating no significant difference between the two treatments. The studies also evaluated the effectiveness of joint mobilization in treating low back and neck pain. They found no significant differences in pain intensity and range of motion between subjects who received mobilization and placebo immediately or short-term after treatment. Mobilization was significantly better than massage or physiotherapy in improving pain, disability, global assessment, analgesic medication intake, and the number of sick leave days in chronic nonspecific pain at intermediate-term post-treatment followup.
A systematic review by Chou et al. [11], evaluated the effectiveness of spinal manipulation. While researchers initially found 61 trials pertaining to the subject, only 19 met the inclusion criteria and were included in the systematic review of manipulation for low back pain. Results showed that spinal manipulation had small, statistically nonsignificant effects on pain at 1 month compared with sham manipulation. The systematic review found no differences in pain relief at 1 week between spinal manipulation and treatments considered inactive.
A 2009 systematic review by Vernon & Schneider [36] looked at manipulation for treatment of myofascial trigger points (MTrP) [37]. The studies found that moderately strong evidence supports manipulation and ischemic pressure for immediate pain relief at MTrPs, but only limited evidence exists for long-term pain relief at MTrPs. Limited evidence supports electrical muscle stimulation, highvoltage galvanic stimulation, interferential current, and frequency modulated neural stimulation in the treatment of MTrPs and myofascial pain syndrome. Evidence is weak for ultrasound therapy. Based on the evidence presented in the included systematic reviews, spinal manipulation does not appear to be an effective form of treatment for different pain types, including back pain.
Stretching and exercises: Stretches and exercises are utilized for a variety of reasons that include pain management, injury prevention, and increased range of motion and function. In a 2015 systematic review by Gross et al. [38], 27 trials looked at 2,485 analyzed and 3,005 randomized participants who had completed exercises for mechanical neck disorders [20]. The systematic review intended to assess the effectiveness of exercise in improving pain, disability, function, patient satisfaction, and quality of life in neck pain patients. The participants were adults suffering from neck pain with or without cervicogenic headache or radiculopathy. The results of the study varied. For acute neck pain, no evidence was found; for chronic neck pain and chronic cervicogenic headache, moderate quality evidence was found; for acute radiculopathy, low quality evidence was found. The study concluded that due to the lack of high quality evidence, there is still uncertainty concerning the effectiveness of exercise for treating neck pain. Researchers did find that using strengthening exercises for chronic neck pain, cervicogenic headache, and radiculopathy may be beneficial as well as using strength and endurance exercises for the cervico scapulothoracic and shoulder.
In a 2014 systematic review of 32 studies, Filho et al. [39], assessed the effectiveness of stretching for posture correction. Researchers found very little evidence supporting effectiveness in this particular treatment modality [40]. In a 2004 systematic review of 6 studies by Thacker et al. [41], researchers sought to determine if stretching has the capability to reduce the risk of a sports injury [35]. There was no evidence that supported either the continuation or discontinuation of stretching before or after exercise to reduce risk of injury. In a 2008 systematic review of 7 randomized controlled trials by Small et al., researchers found no decrease of overall exercise-related injuries by means of stretching. However, researchers did find that musculotendinous injuries reduced as a result of static stretching [39].
A systematic review carried out by Gordan & Bloxham [42] examined 480 studies, but only 14 studies met the criteria on how physical activity or exercise interventions affected patients with non-specific chronic low back pain (NSCLBP), by specifically looking at aerobic exercise, muscular strength and stabilization exercises and/or flexibility training. The researchers found that exercise programs that involved the previously mentioned methods are beneficial for NSCLBP, but did not help with acute low back pain, as exercise produced more swelling in the affected area [43].
A systematic review carried out by Saragiotto et al. [13], examined 2431 studies, but only included 29 trials that met the criteria on how motor control exercise (MCE) can aid in relief of patients with nonspecific low-back pain [44]. The study found very low to moderate evidence showing how MCE can clinically help chronic low-back pain, low quality evidence that MCE has a clinically important effect compared with exercise plus electrophysical agents, moderate to high quality evidence that showed how MCE provides similar outcomes to manual therapies, and low to moderate quality evidence that it provides similar outcomes to other form of exercise. Due to the evidence showing that MCE is not superior to the other methods of treatment, the choice of exercise for lower-back pain should be dependent on patient or therapist preferences [44].
In a systematic review by Miller et al. [14], researchers sought to determine whether a combination of manual therapy and exercise was more effective than using either manual therapy or exercise alone. Participants included adults with acute to chronic neck pain with or without radiculopathy or cervicogenic headache. 17 trials were selected from 31 different publications with 1,820 citation postings. Of the 31 different publications 17 studied acute neck pain, 5 studied whiplash associated disorders, 1 studied degenerative changes, 5 studied cervicogenic headache, and 3 studied neck disorders. The review suggests that when using manual therapy, there is greater short-term pain relief, rather than exercise alone, but there are no long-term differences across the multiple outcomes for acute/chronic neck pain. Moderate quality evidence supports the combination of manual therapy and exercise for pain reduction and improved quality of life over manual therapy alone for chronic neck pain. It also suggests greater short-term pain reduction when compared to traditional care for acute whiplash. A combination of manual therapy and exercise produce greater shortterm pain reduction than exercise alone when compared to manual therapy alone. Researchers found moderate, low, or no evidence supporting the idea that exercise is a beneficial mode of treatment in itself. The systematic reviews showed that a combination of manual therapy and exercise has longer short-term effective in pain relief than the use of manual therapy or exercise alone but there is no long-term effect.
A systematic review by Chou et al. [11], found 122 trials that evaluated exercise and included 37 trials that evaluated the effectiveness of exercise in treating low back pain. The results showed that there was no difference between exercise therapy and no exercise on pain. For comparisons involving other types of exercise techniques, no clear differences were observed in more than 20 head-to-head trials of acute or chronic back pain. An overwhelming amount of systematic reviews show that stretches and exercises provides little to no pain relief.
Manual therapy and exercise: Therapeutic exercise and orthopedic manual therapy are the most common treatment methods for impingement syndrome [45]. The systematic review by Desmeules et al. [44] reviewed the effectiveness of therapeutic exercise and orthopedic manual therapy for the treatment of impingement syndrome. The studies were included if: they were a randomized controlled trial; they were related to impingement syndrome, rotator cuff tendinitis, or bursitis; one of the treatments included therapeutic exercise or manual therapy. Seven trials met these inclusion criteria and 4 of the 7 trials suggested some benefit of manual therapy or therapeutic exercise compared with other treatments such as acromioplasty, placebo, or no intervention. The study found that there is limited evidence that support the efficacy for treatment of impingement syndrome by using therapeutic exercise and manual therapy [42].
In a systematic review by Miller et al. [14], researchers sought to determine whether a combination of manual therapy and exercise was more effective than using either manual therapy or exercise alone. Participants included adults with acute to chronic neck pain with or without radiculopathy or cervicogenic headache 17 trials were selected from 31 different publications with 1,820 citation postings. Of the 31 different publications 17 studied acute neck pain, 5 studied whiplash associated disorders, 1 studied degenerative changes, 5 studied cervicogenic headache, and 3 studied neck disorders. The review suggests that when using manual therapy, there is greater short-term pain relief, rather than exercise alone, but there are no long-term differences across the multiple outcomes for acute/chronic neck pain [11]. Moderate quality evidence supports the combination of manual therapy and exercise for pain reduction and improved quality of life over manual therapy alone for chronic neck pain. It also suggests greater shortterm pain reduction when compared to traditional care for acute whiplash. A combination of manual therapy and exercise produce greater short-term pain reduction than exercise alone when compared to manual therapy alone. Researchers found moderate, low, or no evidence supporting the idea that exercise is a beneficial mode of treatment in itself. The systematic reviews showed that a combination of manual therapy and exercise has longer short-term effective in pain relief than the use of manual therapy or exercise alone but there is no long-term effect.
Kinesio tape: Kinesio Taping is a therapeutic taping technique that supports fascia, muscles, and joints while allowing an unrestricted range of motion. Kinesio Tape, or KT, is theorized to help with lymphatic and blood circulation, and therefore reducing pain, inflammation and recovery times. A systematic review by Borchers et al. [45] reviewed 6 studies that researched the efficacy of Kinesio Taping for musculoskeletal injury [41]. The review found insufficient evidence to either support or oppose the use of KT to prevent injury, decrease inflammation and pain not related to injury, and recovery time. According to these systematic reviews, there is lacking evidence on whether or not Kinesio Tape is effective or ineffective in reducing pain.
Active release technique: The active release technique (ART) is a manual therapy method that is used for the recovery of function within soft tissue, which focuses on removing scar tissue that may cause stiffness, pain, mechanical dysfunctions and muscle weaknesses [12]. There is only one randomized study that looks at the applications of ART, with the rest of the studies being pilot studies. The randomized clinical trial done by Kim, et al looked at 24 subjects with a history of neck pain that lasted more than three months, and looked at the effectiveness of using ART to increase the range of motion in patients. The results of the study show that using ART and joint mobilization show improvement for chronic neck pain; however, ART demonstrated a greater improvement for patients with neck pain involving a soft tissue injury. Therefore, the study concluded that ART appears to be a better option in the short term for treating patients with chronic neck pain. However, due to the small sample size and limited information regarding patient function activities, it is hard to conclude that the treatment is clinically effective. Although it was found that ART can be effective in the short term, the sample size is too small and the study did not look at any aspects of long-term effectiveness, patient’s function activities, so further studies would be needed to evaluate that.
Strain counterstrain technique: Strain counterstrain (SCS) is an technique that uses passive positioning to relieve tender point palpation pain and associated dysfunction [15]. The systematic review by Wong et al. [46] included randomized control trials comparing tender point palpation pain after isolated strain counter strain treatment compared to control conditions assessed with a visual analog scale. The systematic review and meta analysis found low quality evidence suggesting that strain counter strain may reduce tender point palpation pain. Future studies with larger samples of better quality studies with patient populations that assess long-term pain, impairment, and dysfunction outcomes could enrich the literature. Based on this study review, there was no evidence that SCS has effect in treating tender point pain in the long term and more studies are needed to evaluate what effect it does have on tender point palpation pain and patient function activities.
Craniosacral therapy: Craniosacral Therapy is a treatment approach that aims to release restrictions around the spinal cord and brain and subsequently restore body function [36]. In a systematic review by Jakel & Hauenschild [47] aimed to evaluate the clinical benefits of craniosacral therapy. The systematic review included studies describing observational or randomized controlled trials in which craniosacral therapy was the only treatment method was used [36]. 7 studies met the criteria, they consisted of 3 randomized controlled trials and 4 observational studies. This review revealed the paucity of craniosacral therapy research in patients with different clinical pathologies. Craniosacral therapy is feasible in randomized control trials and has the potential to provide valuable outcomes to further support clinical decision making. However, due to the current lack of methodological quality of the studies, further research is needed.
Another systematic review by Green et al aimed to assess the biological plausibility, assessment reliability, and clinical effectiveness of craniosacral therapy [48]. They gathered 33 studies that provided primary data on craniosacral therapy. Of the 33 studies, 7 provided data on the effectiveness of craniosacral therapy and were included in the systematic review. The systematic review found that there was insufficient evidence to support craniosacral therapy as clinically effective. The available research on craniosacral treatment effectiveness represents low quality evidence conducted using inadequate research protocols. Research methods that could conclusively evaluate effectiveness of craniosacral therapy as an intervention have not been applied to date. After reviewing the studies on craniosacral therapy, further research is needed to get better quality evidence that supports this form of treatment because cur-rent evidence is low quality and shows no conclusive evidence of effectiveness.
McKenzie method: The McKenzie method is a popular approach to manage spinal pain. One of the key aspects of the McKenzie method is that patients receive individualized treatment based on their condition [47]. In a systematic review by Clare et al. [49], the goal was to investigate the efficacy of McKenzie therapy in the treatment of spinal pain. For this systematic review they gathered 24 studies, with 6 randomized trials that qualified for the review [46]. At short term follow up the McKenzie therapy provided a mean 8.6 pain reduction on a 0 to 100 point scale. In one cervical trial Mckenzie therapy provided similar benefits to an exercise program. The results of the review showed that McKenzie therapy does result in a greater decrease in pain and disability in short term compared to standard therapies. There is not enough data on the long term effects of the Mckenzie method.
In another systematic review by Machado et al, they looked at randomized trials to evaluate the effectiveness of the McKenzie method for low back pain [47]. 11 randomized trials were included in this review. In these 11 randomized trials, it showed that on a 0 to 100 point scale pain reduction was at -4.16 points and disability at -5.22 points at the 1 week follow-up when compared with passive therapy for acute lower back pain. When the McKenzie method was compared with the stay active advice, a reduction in disability favored the advice, at the 12 week follow up. The review concluded that the McKenzie method is more effective than passive therapy for lower back pain. However, the magnitude of difference suggest that there are no clinically worthwhile effects. There is also limited evidence for the use of the McKenzie method in chronic low back pain [47].
Biopsychosocial
While chronic pain continues to plague the American population, research shows that a biopsychosocial model such as the multidisciplinary approach, cognitive-behavioral rehabilitation and Advanced Soft Tissue Release (ASTR) may be the answer to this epidemic. The biopsychosocial model is a holistic approach as it encompasses multiple aspects, including the biological, psychological, and social aspects [50]. This multidisciplinary approach was developed by Engel [51]. Engel argues that there are certain limitations to a purely biomedical model in regards to treatment. In order to better understand a disease and determine an effective treatment approach, medical care providers should take into account the social context of the patient, the physician’s role in the illness, and the encompassing whole self of the patient, thus suggesting the biopsychosocial model.
In industrialized countries, chronic musculoskeletal pain has eased its way into becoming more prevalent, with 35% commonality in these given populations [50]. Rather than addressing symptoms on a one dimensional perspective, the biopsychosocial model strives to understand and treat pain on a multidimensional platform. While single modality models evaluate how to treat a patient’s immediate symptoms, the biopsychosocial model strives to identify the underlying cause of the symptoms in order to treat the patient in a more holistic manner. The systematic review by Mavrocordatos et al. [31] suggests that biopsychosocial treatment is beneficial for not only treatment but also early diagnosis. These two factors are important for many conditions that cause chronic pain, such as rheumatoid arthritis [52]. Researchers determined that those who received multidisciplinary treatment that includes a range of strategies was more effective compared to a non-multidisciplinary approach. Turk & Okifuji [52] argue in their literature review that there have been no specific surgical procedures, pharmacological agents, or physical treatment methods that yielded effective results in regards to treating chronic pain long-term. While pain does affect a person physically, it can promote negative emotional feelings as well. Pain is not simply limited to the injury in the body; rather, it encompasses psychological and environmental factors in addition to the injury. Researchers suggest that the greatest improvement in medicine has been the development of the multidisciplinary, holistic treatment approach. While some third party payers are more inclined to pay for surgery than a multidisciplinary pain clinic, most patients who turn to multidisciplinary pain clinics have already had surgery that has not proved to be effective. This suggests that having patients go to a multidisciplinary pain clinic instead of surgery may be a more cost effective plan. Research points to the fact that more than 60% of people in a multidisciplinary pain clinic have more than one psychological impairment thus demonstrating the importance of a holistic approach. Research also suggests that in multidisciplinary pain clinics, there is a 20-30% of pain reduction. In addition, this pain reduction either seems to stay around 20-30% or continue to decline [22].
In the systematic review published by Tzenalis et al. [50] randomized controlled trials were evaluated to determine how the biopsychosocial model compares to other treatment methods, either when utilized together or individually. The biopsychosocial model in this study included medical, education, cognitive behavioral therapy, relaxation, biofeedback, and social therapy. The study included subjects between the ages of 18 and 75 who had been suffering from chronic pain for longer than 12 weeks. Based on their review, researchers argue that cognitive-behavioral rehabilitation, a form of the biopsychosocial model, yields longterm results.
In the systematic review conducted by Kamper et al. [53], researchers analyzed how effective a multidisciplinary treatment approach was in the long term. This study was limited to assessing individuals who suffered from lower back pain for more than three months, many of which had little success with other treatment methods. The systematic review included 41 trials, 16 of which compared usual care to multidisciplinary approaches and 19 of which compared the multidisciplinary approach physical treatment methods. There were a total of 6,858 participants. The data suggests moderate quality evidence pointing to positive effectiveness of multidisciplinary approach as opposed to usual care. The study concluded that multidisciplinary rehabilitation programs resulted in better outcomes with respect to long term pain and disability compared with usual care (moderate quality evidence) or physical treatments (low quality evidence).
Guzmán et al. [54] addressed the effectiveness of a biopsychosocial treatment approach for those suffering from chronic low back pain. The systematic review included randomized controlled trials. 1,964 individuals were included in this study, all of which expressed issues with low back pain for at least 3 months. In each of the 10 studies included in this systematic review, the biopsychosocial method of treatment was compared to a control. The control was defined as treatment that did not meet the qualifications to be considered a multidisciplinary treatment approach. When compared to a control, strong evidence suggests that the biopsychosocial treatment approach was more effective with functional improvement compared to non-multidisciplinary treatment. In addition, moderate evidence indicates superior effectiveness of the multidisciplinary model for pain treatment than a non-multidisciplinary approach.
A systematic review by Karjalainen et al. [55] aimed to evaluate the effectiveness of multidisciplinary biopsychosocial rehab for sub acute low back pain among adults [49]. Many randomized controlled trials were identified that met the criteria. Of 1808 references, only 2 relevant studies were included. The study showed that there was moderate evidence showing that multidisciplinary rehabilitation for sub acute low back pain helps patients return to work faster and results in fewer sick leaves. Based on the review, there is moderate evidence which show that multidisciplinary rehabilitation for sub acute low back pain is effective, but there is a need for more highquality trials in this field of study [49].
A systematic review by Ospina and Harstall looked to evaluate the effectiveness of multidisciplinary pain programs for chronic pain [56]. There were a total of 13 systematic reviews identified as relevant, although only 5 met the inclusion criteria. Out of the 5, they focused on 1 that addressed the effectiveness of multidisciplinary pain programs on chronic pain. The review they chose included 65 controlled and non-controlled trials. The results from the systematic review showed support for the effectiveness of intensive multidisciplinary pain programs for chronic pain patients in terms of their effects on functional improvement and pain reduction.
A systematic review by Van Geen et al. aimed to determine the long-term effect of multidisciplinary back training on the work participation of patients with chronic low back pain [57]. They found 10 studies that met the inclusion criteria and of the 10, 5 studies had a low methodologic quality. The other 5 were high quality studies and each of them found a positive effect on at least one of the 4 outcomes being measured. The review concluded that in the long-term, multidisciplinary back training has a positive effect on work participation in patients with chronic low back pain.
Figure 1:The bar graph above illustrates the table by listing the modalities that provided short-term pain relief on the bottom of the graph. The names are lined up according to the bar that shows the bar that shows the number of studies that support the fact that they have a short-term effect on pain relief. The bar graph helps illustrate which modalities had the highest number of studies showing that they are only effective for short-term pain relief. *All systematic review studies except: ART & opioid are RCT dry needle has 1 literature review.

A systematic review by Ravenek et al. [57] reviewed 12 articles and the effectiveness of multidisciplinary methods in regards to the employment outcomes of chronic lower back pain (CLBP) [58]. The quality of these methods for each of the articles varied as some had higher quality methods compared to others. The findings of the review indicate conflicting results for the effectiveness of the multidisciplinary approach for reducing pain, and improving function and employment outcomes for individuals with CLBP without the use of occupational therapy (OT) methods. However, the data illustrated that 3 of the 12 articles, which included OT approaches, had low quality ratings with two employment outcomes of sick leave from work, and one returning to work. The review overlooked the other articles, which had no OT component, where 2 multidisciplinary treatments with high quality ratings with an employment outcome of returning to work, 3 treatments with low quality ratings approaching the higher quality side, and 2 low quality ratings for articles without occupational therapy as part of the multidisciplinary treatment. The results of this review will not be added to the statistics due to biases towards OT methods in regards to the multidisciplinary approach (Figure 1 & 2).
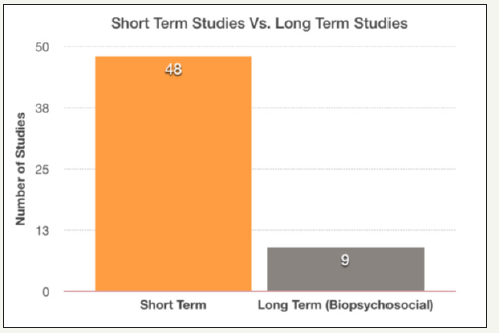
Figure 2:The bar graph above illustrates the number of short-term pain relief studies conducted versus the number of long-term pain relief (biopsychosocial) studies conducted.
Advanced Soft Tissue Release (ASTR) is a biopsychosocial treatment model implemented by one clinician and includes working on multiple aspects including soft tissue release, ergonomics, stress management, behavior modification, body mechanics, posture, gait, exercise and patient education. Reviewers determined to include ASTR retrospective cohort study even though it is not a systematic review study for two reasons. First, the biopsychosocial model was implemented by one clinician, which is different from other biopsychosocial studies that were included. Previous biopsychosocial studies were executed by several clinicians. Second reason is that the subjects in ASTR study were not a sample subjects, they were the entire population during the period between March 2013 and April 2015 who met the study criteria. This study is unique due to including all population which made it a valuable study to review in this report. ASTR approach shows the potential of cost saving through implementing the biopsychosocial by one clinician instead of several clinicians which will save time and reduce financial burden on patients and decrease overall healthcare cost.
In a research study assessing the long-term benefits of ASTR, 105 participants who sought treatment for neck pain between March 2013 and April 2015 were included. Some of these patients had a history of past treatment that had not relieved their symptoms. The study exclusions included those who were pregnant, had a cancer diagnosis, structural deformity of the neck, pain from a car accident, stroke, cerebral palsy, multiple sclerosis, spinal stenosis, Parkinson’s disease, or recent surgery. 83% of participants expressed feelings of pain relief after one session. In a follow up questionnaire, which occurred about one year later, 87% of patients had no neck pain. This specifically supports the longterm effectiveness of ASTR as biopsychosocial treatment model [30].
Results
16,145 articles were identified during the database research. Only a total of 57 studies met the criteria of this study, with 50 being systematic reviews, 4 randomized controlled trials (RCT), 1 non- RCT, and 2 literature reviews. The single modality studies were 47 studies, totalled as 53 individual different findings because some studies evaluated several single modalities in the same study. The findings of the 47 studies were consistent regarding that the single modalities provided short term pain reduction or no pain reduction. The biopsychosocial model studies were 7 systematic reviews, 1 literature review, 1 cohort study that consistently showed long term pain reduction, improved range of motion, and improvement in functional activities.
Table 1, read left to right, the author, type of study, treatment, body part, the number of participants or studies, and the effect of the treatment. This table can be used to compare the different types of treatment and their effects of pain management. It shows that the biopsychosocial treatment seems to be a better option for long term pain reduction. The other treatment methods yielded either short term pain reduction or no pain reduction. Table 2 shows short term and long term treatments, along with the type and number of studies within each type of treatment. This table shows the amount of options for short term pain management in comparison to the long term pain management options (Table 3).
Table 1:

Table 2:The table above shows short term modalities for pain in the first column. The second column shows the type of studies done mostly consisting of systematic reviews (SR). The third column shows the number of studies. The fourth column shows long term modalities for pain. The fifth column shows the type of studies done mostly consisting of systematic reviews (SR). The last column shows the number of studies.
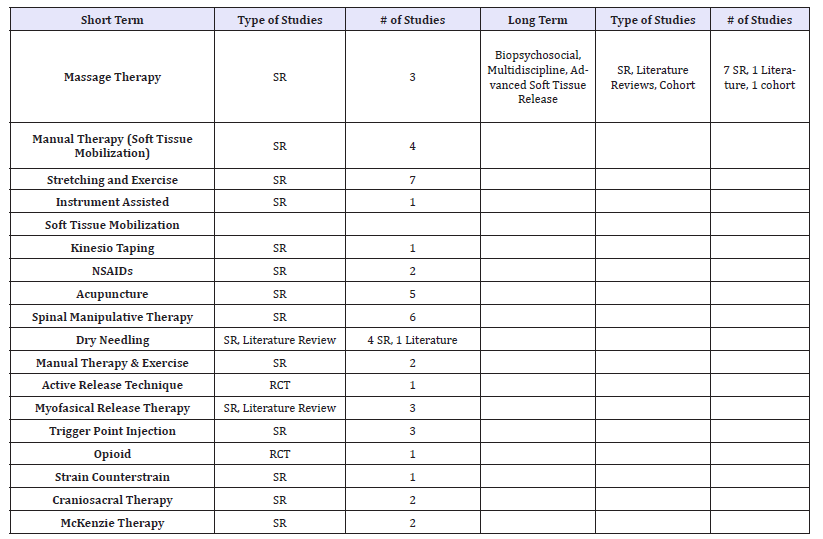
Table 3:The table above lists the different types of modalities that were studied on the left side. On the right side of the table, the number of studies done for each modality is listed. All the modalities listed were found to have a shortterm effect on pain relief.
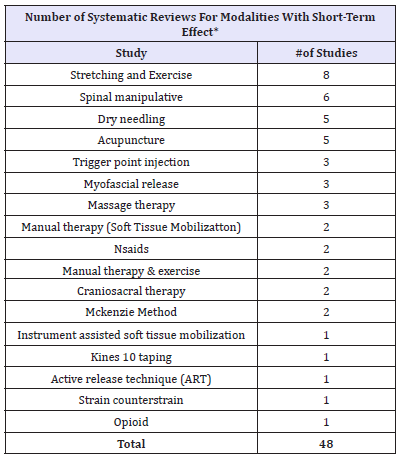
*All systematic review studies except: ART & opioid are RCT and dry needle has 1 literature review.
Future Study Recommendations
Further research should be conducted to further assess the relationship between treatment methods and improvement of health and duration of improvement. We would suggest future research assessing how many kinds of treatment should be included in the biopsychosocial treatment model and how long treatment should last to attain the long term effects. In addition, further research should be conducted to specifically address why single modality models seem to yield only short term results.
Conclusion
Chronic pain affects 100 million Americans, limiting functioning and quality of life in these individuals.2 Modern medicine has developed multiple ways to treat chronic pain, ranging from various single modalities to holistic, biopsychosocial approaches. As research progresses, clinicians have argued the effectiveness of certain treatment methods over others in regards to long term pain relief. In regards to opioid used, the risk may outweigh the benefits. In addition, there is minimal research discussing the long term effects of opioid use. Patients who utilize high dose opioids appear to have decreased levels of functioning and quality of life. NSAIDs, another method of pain reduction, seem to have fleeting results and some forms may produce possible adverse outcomes. For example, rofecoxib and diclofenac have been correlated with an increased risk of ischemic stroke [9]. While Bervoets et al. [10] found that massage therapy was effective when compared to no treatment massage therapy was not as effective as some other treatment forms and did not yield long-term results.
As seen through research conducted by Cheatham et al., minimal evidence exists supporting the effectiveness of instrument assisted soft tissue mobilization (IASTM) for treatment of musculoskeletal pathology. Some evidence supported increased range of motions in the joints from utilization of IASTM, but these results were short term [17]. Similarly, manual therapy yielded short-term results for neck pain reduction, as supported by research by Miller et al. [14] Acupuncture, another single modality approach, was more effective than no treatment, but less effective than other treatment methods [24]. In addition, minimal difference exists in pain reduction between those who received acupuncture and those who received placebo [22]. Continuing with single modality treatments, dry needling reduced pain short term, but did not have a positive effect on function, quality of life, depression, range of motion, or strength [26]. Furthermore, there seemed to be no pain improvement between trigger point injections and placebo [27]. Researchers found no evidence supporting the effectiveness or ineffectiveness of trigger point injections [33]. As for joint manipulation, evidence suggests that spinal manipulation seemed ineffective for all evaluated forms of pain, including but not limited to, neck and back pain [5].
As for kinesio tape, yet another single modality treatment method, researchers found insufficient evidence for both support and opposition of the use of kinesio tape to prevent injury and decrease inflammation, pain, and recovery time. In regards to exercise treatment, researchers found no more than moderate quality evidence supporting the effectiveness of exercise therapy in itself. Researchers argue that the combination of manual therapy and exercise produced greater short-term pain reduction than exercise alone compared to manual therapy alone [45].
In regards to Active release technique (ART), there results of the study provided insignificant evidence supporting the effectiveness of using this method to treat chronic neck pain in a clinical setting, as the short term benefits were not sufficient enough for daily functional activities. Due to the duration of the study, it failed to provide any long term effects for this method [12]. After reviewing the studies on craniosacral therapy, further research is needed to get better quality evidence that supports this form of treatment because current evidence is low quality and shows no conclusive evidence of effectiveness. In regards to Strain counter strain, there was no evidence that SCS has effect in treating tender point pain in the long term and more studies are needed to evaluate what effect it does have on tender point palpation pain and patient function activities. There is a positive short term effect on pain reduction and disability using the Mckenzie method when compared to passive therapy. However, a long term effect is not a seen in the McKenzie therapy when compared to the advice of staying active, as it is better to just stay active rather than go through the McKenzie therapy [47].
Based on the studies reviewed, the biopsychosocial model yields positive results in terms of long term effectiveness for pain relief and overall health. The biopsychosocial model uses multidisciplinary approaches to treat chronic back pain, and the studies showed that using this methods yields long-term pain relief. Cognitive-behavioral rehabilitation, a form of the biopsychosocial model, yielded positive results in regards to long-term health [50]. ASTR, a treatment method that follows the biopsychosocial model, yielded positive results for those suffering from neck pain in the long term. During follow up sessions, which occurred about one year later, 87% of patients had no neck pain [30].
Based on the studies evaluated, treatment methods following the biopsychosocial model seem to yield long term pain reduction, increased range of motion, and improvement in functional activities. On the other hand the single modality treatment methods such as opioid use, non-steroidal anti-inflammatory drugs, massage therapy, manual therapy (soft tissue mobilization), instrument assisted soft tissue mobilization, myofascial release, acupuncture, soft tissue release, dry needle, trigger point injection, joint manipulation/joint mobilization, active release technique, strain counter strain, craniosacral therapy, stretching/exercise, McKenzie method, and kinesio taping seemed to yield either short term pain reduction or no pain reduction. Based on this literature review there is solid evidence that the biopsychosocial treatment model is more effective than single modalities in providing longterm pain reduction. We hope that more clinicians embrace the biopsychosocial model in their practice to improve the quality of patient’s care.
Ethical Approval and Consent to participate
Even though the study does not report on or involve the use of any animal or human data or tissue, the study received Institutional Review Board (IRB) committee approval to conduct literature review
Availability of Supporting Data
The datasets generated and/or analyzed during the current study are available when search the following databases Medline, ScienceDirect, PubMed, Embase, Google Scholar, Cinahl, BioMed Central, and Cochrane.
Authors’ Contributions
JJ, MS, TJ, HH and IN searched and collected the studies form the online databases. MS, TJ, HH, MV, CM, LR, KM and IN analyzed and interpreted the collected research studies.
Acknowledgement
Israel Rodriguez proofread this study.
References
- Reuben DB, Alvanzo AA, Ashikaga T, Bogat GA, Callahan CM, et al. (2015) National institutes of health pathways to prevention work-shop: the role of opioids in the treatment of chronic pain. Ann Intern Med 162(4): 295- 300.
- ASAM (2016) Opioid Addiction 2016 Facts & Figures. American Society of Addiction Medicine, USA.
- Georgia Prevention Project (2017) Prescription opioids and heroin epidemic in Georgia. SARA, Georgia.
- Korff MRV (2013) Long-term use of opioids for complex chronic pain. Best Pract Res Clin Rheumatol 27(5): 663-672.
- Ernst E, Canter PH (2006) A systematic review of systematic reviews of spinal manipulation. JR Soc Med 99(4): 192-196.
- Xue CC, Helme RD, Gibson S, Hogg M, Arnold C, et al. (2012) Effect of electroacupuncture on opioid consumption in patients with chronic musculoskeletal pain: protocol of a randomised controlled trial. Trials 13: 169.
- Machado GC, Maher CG, Ferreira PH, Day RO, Pinheiro MB, et al. (2017) Non-steroidal anti-inflammatory drugs for spinal pain: a systematic review and meta-analysis. Ann Rheum Dis 76(7): 1269-1278.
- Turk DC, Okifuji A (1998) Treatment of chronic pain patients: clinical outcomes, cost-effectiveness, and cost-benefits of multidisciplinary pain centers. Critical ReviewsTM in Physical and Rehabilitation Medicine 10(2): 181-208.
- Lorenzo VC, Guardia NR, Calingaert B, Castellsague J, Pariente A, et al. (2011) Stroke risk and NSAIDs: a systematic review of observational studies. Pharmacoepidemiol Drug Saf 20(12): 1225-1236.
- Bervoets DC, Luijsterburg PA, Alessie JJ, Buijs MJ, Verhagen AP (2015) Massage therapy has short-term benefits for people with common musculoskeletal disorders compared to no treatment: a systematic review. J Physiother 61(3): 106-116.
- Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, et al. (2017) Nonpharmacologic therapies for low back pain. Ann Intern Med 166(7): 493-505.
- Kim JH, Lee HS, Park SW (2015) Effects of the active release technique on pain and range of motion of patients with chronic neck pain. J Phys Ther Sci 27(8): 2461-2464.
- Furlan A, Yazdi F, Tsertsvadze A, Gross A, Tulder MV, et al. (2010) Complementary and alternative therapies for back pain II. Evid Rep Technol Assess (Full Rep) 194: 1-764.
- Miller J, Gross A, Dsylva J, Burnie SJ, Goldsmith CH, et al. (2010) Manual therapy and exercise for neck pain: A systematic review. Man Ther 15(4): 334-354.
- Wong CK, Abraham T, Karimi P, Ow-Wing C (2014) Strain counterstrain technique to decrease tender point palpation pain compared to control conditions: a systematic review with meta analysis. J Bodyw Mov Ther 18(2): 165-173.
- Penas CF, Campo MS, Carnero JF, Miangolarra JC (2005) Manual therapies in myofascial trigger point treatment: a systematic review. Journal of Bodywork and Movement Therapies 9(1): 27-34.
- Cheatham SW, Lee M, Cain M, Baker R (2016) The efficacy of instrument assisted soft tissue mobilization: a systematic review. J Can Chiropr Assoc 60(3): 200-211.
- Cheatham SW, Kolber MJ, Cain M, Lee M (2015) The effects of selfmyofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: a systematic review. Int J Sports Phys Ther 10(6): 827-838.
- Beardsley C, Škarabot J (2015) Effects of self-myofascial release: A systematic review. J Bodyw Mov Ther 19(4): 747-758.
- Gross A, Kay TM, Paquin JP, Blanchette S, Lalonde P, et al. (2015) Exercises for mechanical neck disorders. Cochrane Database Syst Rev 1: CD004250.
- Ajimsha M, Al-Mudahka NR, Al-Madzhar J (2015) Effectiveness of myofascial release: Systematic review of randomized controlled trials. J Bodyw Mov Ther 19(1): 102-112.
- Madsen MV, Gotzsche PC, Hrobjartsson A (2009) Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ 338: a3115.
- Yuan Q, Wang P, Liu L, Sun F, Cai YS, et al. (2016) Acupuncture for musculoskeletal pain: A meta-analysis and meta-regres-sion of shamcontrolled randomized clinical trials. Sci Rep 6: 30675.
- Furlan AD (2010) Systematic review of acupuncture for chronic lowback pain. JAM 6(1): 37-44.
- Dunning J, Butts R, Mourad F, Young I, Flannagan S, et al. (2014) Dry needling: a literature review with implications for clinical practice guidelines. Phys Ther Rev19(4): 252-265.
- Morihisa R, Eskew J, McNamara A, Young J (2016) Dry Needling in subject with muscular trigger points in the lower quarter: a systematic review. Int J Sports Phys Ther 11(1):1-14.
- Cummings TM, White AR (2001) Needling therapies in the management of myofascial trigger point pain: a systematic review. Arch Phys Med Rehabil 82(7): 986-992.
- Gattie E, Cleland JA, Snodgrass S (2017) The effectiveness of trigger point dry needling for musculoskele-tal conditions by physical therapists: a systematic review and meta-analysis. J Orthop Sports Phys Ther 47(3): 133-149.
- Cotchett MP, Landorf KB, Munteanu SE (2010) Effectiveness of dry needling and injections of myofascial trigger points associated with plantar heel pain: a systematic review. J Foot Ankle Res 3: 18.
- Jacobs J, Wilson J, Ireland K (2016) Advanced soft tissue release® (ASTR®) long- and short-term treatment results for patients with neck pain. MOJ Orthopedics & Rheumatology 5(4): 00188.
- Antúnez LE, Tejeda JF, Cabello AM, Mansilla JR, Torres CB, et al. (2017) Dry needling in the management of myofascial trigger points: A systematic review of randomized controlled trials. Complement Ther Med 33: 46-57.
- Young JL, Walker D, Snyder S, Daly K (2014) Thoracic manipulation versus mobilization in patients with mechanical neck pain: a systematic review. J Man Manip Ther 22(3): 141-153.
- Scott NA, Guo B, Barton PM, Gerwin RD (2009) Trigger point injections for chronic non-malignant musculoskeletal pain: a systematic review. Pain Med 10(1): 54-69.
- Rubinstein SM, Terwee CB, Assendelft WJ, Boer MRD, Tulder MWV (2011) Spinal manipulative therapy for acute low-back pain: an update of a Cochrane review. Spine 36(13): E825-E846.
- Thacker SB, Gilchrist J, Stroup DF, Kimsey CD (2004) The impact of stretching on sports injury risk: a systematic review of the literature. Med Sci Sports Exerc 36(3): 371-378.
- Jakel A, Von Hauenschild P (2012) A systematic review to evaluate the clinical benefits of craniosacral therapy. Complement Ther Med 20(6): 456-465.
- Vernon H, Schneider M (2009) Chiropractic management of myofascial trigger points and myofascial pain syndrome: a systematic review of the literature. J Manipulative Physiol Ther 32(1): 14-24.
- Sánchez AMC, Peñarrocha GAM, Morales MA, Hernández MS, Sola CF, et al. (2011) Effects of myofascial release techniques on pain, physical function, and postural stability in patients with fibromyalgia: a randomized controlled trial. Clin Rehabil 25(9): 800-813.
- Small K, Naughton LM, Matthews M (2008) A systematic review into the efficacy of static stretching as part of a warm-up for the prevention of exercise-related injury. Res Sports Med 16(3): 213-231.
- Filho S, Nunes DJ, Lírio GJ, Flávia P (2014) Effects of stretching exercises for posture correction: systematic review. Manual Therapy, Posturology & Rehabilitation Journal 12: 265-272.
- Borchers J, Mostafavifar M, Wertz J (2012) A systematic review of the effectiveness of kinesis taping for musculoskeletal injury. Phys Sportsmed 40(4): 33-40.
- Desmeules FCA, Côté CH, Frémont P (2003) Therapeutic exercise and orthopedic manual therapy for im-pingement syndrome: a systematic review. Clin J Sport Med 13(3): 176-182.
- Gordon R, Bloxham S (2016) A systematic review of the effects of exercise and physical activity on non-specific chronic low back pain. Healthcare 4(2): E22.
- Saragiotto BT, Maher CG, Yamato TP, Costa LO, Costa MLC, et al. (2016) Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev 1: CD012004.
- Desmeules (2016) Impingement syndrome: also called swimmer’s shoulder.
- Helen CA, Roger A, Christoper MG (2004) A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother 50(4): 209-2016.
- Machado, Carneiro LA, Sperling MG, Henrique FP, Loureiro FM (2006) The Mckenzie method for low back pain: a systematic review of the literature with a meta-analysis approach. Spine (Phila Pa 1976) 31(9): E254-E262.
- Green C, Martin CW, Bassett K, Kazanjian A (1999) A systematic review of craniosacral therapy: biological plausibility, assessment reliability and clinical effectiveness. Complement Ther Med 7(4): 201-207.
- Karjalainen KA, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, et al. (2001) Multidisciplinary biopsychosocial rehabilitation for subacute low back pain in working-age adults: a systematic review within the framework of the cochrane collaboration back review group. Spine (Phila Pa 1976) 26(3): 262-269.
- Tzenalis A, Beneka A, Malliou P, Godolias, G, Staurou N (2016) The biopsychosocial treatment approach for chronic neck and back pain: A systematic review of randomized controlled trials. European Psychomotricity Journal 8(1): 29-48.
- Engel GL (1977) The need for a new medical model: a challenge for biomedicine. Science 196(4286): 129-136.
- Mavrocordatos (2016) Benefits of the multidisciplinary team for the patient.
- Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, et al. (2015) Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ 350: h444.
- Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, et al. (2001) Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ 322(7301):1511-1516.
- Geen V, Edelaar MJ, Janssen M, van Eijk JT (2007) The long-term effect of multidisciplinary back training: a systematic review. Spine (Phila Pa 1976) 32(2): 249-255.
- Ospina M, Harstall C (2002) Multidisciplinary pain programs for chronic pain: evidence from systematic reviews. Alberta Heritage Foundation for Medical Research, pp. 1-57.
- Ravenek MJ, Hughes ID, Ivanovich N, Tyrer K, Desrochers C, et al. (2010) A systematic review of multidisciplinary outcomes in the management of chronic low back pain. Work 35(3): 349-367.
- Shete K, Suryawanshi P, Gandhi N (2012) Management of low back pain in computer users: A multidisciplinary approach. J Craniovertebr Junction Spine 3(1): 7-10.
© 2018 Joseph Jacobs. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






