- Submissions

Full Text
Orthopedic Research Online Journal
Comparison Results between Patients with Developmental Hip Dysplasia Treated with Either Salter or Pemberton Osteotomy
Dello Russo Bibiana* and Candia Tapia Jaime Gregorio
Hospital JP Garrahan Larrea, Argentina
*Corresponding author:Dello Russo Bibiana, Hospital JP Garrahan Larrea, Argentina
Submission: September 23, 2017:Published: November 13, 2017

ISSN: 2576-8875 Volume1 Issue4
Abstract
Background: Acetabular dysplasia is defined as the alteration of the normal relationship in the depth and orientation of the acetabulum typically accompanied by a valgus abnormality and ante version of the proximal femur. Different types of pelvic osteotomies were designed to improve the relationship between these components in order to anteversion improve femoral head coverage. The most commonly used techniques are the Salter innominate osteotomy, a re-directional osteotomy, and the Pemberton osteotomy, which is a remodelling technique.
Purpose: The aims of this study were:
a. To compare angle variation on pre- and postsurgical X-rays of patients who underwent correction of acetabular dysplasia with either Salter or Pemberton osteotomy as the primary treatment.
b. To evaluate post-osteotomy premature triradiate cartilage closure during follow-up in both groups.
c. To evaluate residual dysplasia in both groups of children that may have needed an additional acetabular procedure before reaching the age of 10 years.
Patients and method: A retrospective cohort of pediatric patients who underwent surgery because of congenital dislocation of the hip at the Department of Traumatology seen at the pediatric hospital Prof. J. P. Garrahan between 2000 and 2010 was assessed. The children were divided into two groups: 49 children who underwent Salter innominate osteotomy and 47 the Pemberton osteotomy, performed by orthopaedic surgeons with more than 10 years. Children who had received previous surgical or non-surgical interventions (corset or splints of any type, preoperative traction, etc.); children with teratologic dysplasia, syndrome-associated dysplasia, myelodysplasia, orneurological diseases werexcluded from the study.
Results: Correction of the dysplasia with normal angle values (AI: 20°; CE: 9-12 to 25°, and 13-20 to 26-30° ADR 60%) was achieved in 40 hips (83%) in the Pemberton group, and in 22(45%) of the Salter group, with a statistically significant difference (P< 0.001 - Odds ratio 2.17). Intra- and inter observer reliability was assessed using the kappa coefficient, which show it to be good (0. 92). For agreement on the definition of cartilage closure a kappa of 0.73 was found (p 0.001) in this series, X-rays that showed premature closure of the cartilage were more common in the cases treated with the Pemberton technique (52%). Avascular necrosis (in its different stages) was not present before operation. Therefore, avascular necrosis was observed principally (23%) in the Salter osteotomy group, in the group to the group without femoral shortening when compared with the Pemberton osteotomy group (13%). Only two patients in the Salter group required of triple osteotomy within the final follow-up.
Conclusion: Both types of osteotomy were found to be adequate for the management of walking DDH patients with a missed diagnosis under the age of 6 years. Our results suggest that the Pemberton osteotomy achieves better acetabular coverage and is maintained for longer periods of time than the Salter technique, in spite of a higher rate of closed triradiate cartilage. Only two patients in the Salter group required of triple osteotomy within the final follow-up. Level of Evidence: IV
Keywords: Dislocation; Pelvic osteotomy; Femoral shortening; Salter; Pemberton
Introduction
Different types of pelvis osteotomies have been designed to improve femoral coverage. The most commonly used techniques are the Salter in nominate osteotomy and the Pemberton osteotomy. The Salter technique is a complete osteotomy that reorients the entire acetabulum taking the distal segment of the ilion forward, downward, and outward [1] (Figure 1). The Pemberton technique is an osteotomy in which the acetabular roof is turned using the triradiate cartilage as a hinge (acetabuloplasty) [2] (Figure 2). Ponseti [3] showed that a congruent relationship between the femoral head and the acetabulum is important to develop acetabular depth and that this depth will be proportional to the residuary growth of the acetabulum. Conversely, a reduction of the acetabular depth leads to a reduction in the weight-bearing area of the joint surface, increasing the contact pressure in this zone which may lead to the development of osteoarthritis [4-6]. The correlation of acetabular depth index (ADI), acetabular index (AI), and the centeredge angle of Wiberg (CE), is used to evaluate the morphometry of the hip joint. These measurements are useful to determine the degree of acetabular dysplasia [6,7]. The aims of this study were:
Figure 1:
a. To compare pre- and postsurgical X-rays of patients who underwent correction of acetabular dysplasia with either Salter or Pemberton osteotomy as the primary treatment.
b. To evaluate post-osteotomy premature triradiate cartilage closure during follow-up in both groups.
c. To evaluate residual dysplasia in both groups of children that may have needed an additional acetabular procedure before reaching the age of 10 years.
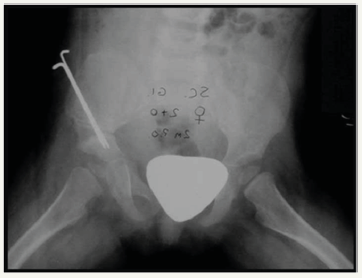
Figure 2a:A 4-year-old patient treated with Pemberton osteotomy.
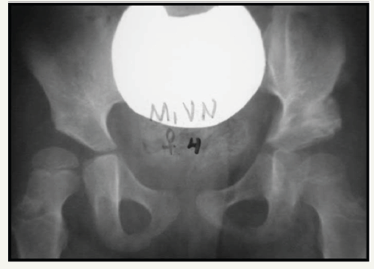
Figure 2b:Same patient at age 10th.

Material and Methods
Design and setting
A retrospective cohort of pediatric patients who underwent surgery because of congenital dislocation of the hip seen at the Department of Traumatology at the pediatric hospital Prof. J. P. Garrahan between 2000 and 2010 was assessed.
Population
Children who underwent surgery for hip dislocation (one group of 49 patients who underwent Salter osteotomy and a second group of 47 patients in whom the Pemberton was used) performed by orthopedic surgeons with at least 10 years of experience and who were followed up at the Department of Traumatology of the Hospital Nacional de Pediatría Profesor J.P. Garrahan were included in the study. Children who had received previous surgical or nonsurgical interventions (corset or splints of any type, preoperative traction, etc.); children with teratologic dysplasia, syndromeassociated dysplasia, myelodysplasia, or neurological diseases were excluded. Radiological studies from the medical records of the children were evaluated. All measurements were performed by two observers, radiologists with more than 10 years of experience, who had not been involved in the clinical follow-up of the patients. Intraand inter observer reliability was assessed using the Cohen-Kappa coefficient [4].
The surgeon who operated on the children also evaluated the X-rays at diagnosis, in the immediate postoperative period, and during follow-up. On the initial X-rays, the Tönnis classification [8] (Figure 1) was used to classify the grade of dislocation.
Classification
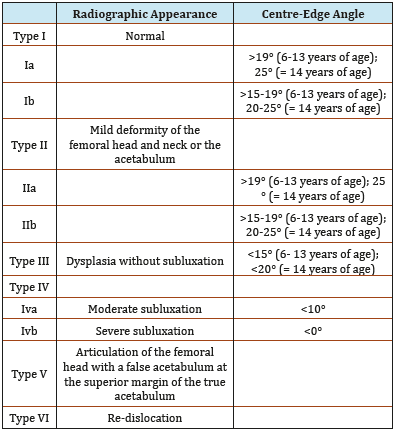
The Tönnis classification is based on the femoral ossification centers in the quadrants that are formed by a horizontal line through the Y cartilage and a vertical tangent from the most external point in the acetabular roof (the line of Ombredanne) (Figure 3). The Sever in classification is used to evaluate the grade of acetabular dysplasia described in six groups (Table 1). The ADI was measured using the Heyman method [7] by dividing the acetabular depth by the acetabular width and multiplying by 100 (Figure 4). The following values were considered as normal (correction of the dysplasia): ADI 60%, AI: 20°; CE: 9-12 years of age: 25°; 13-20 years of age: 26-30°. Additionally, premature closure of the triradiate cartilage during follow-up was reported.
Figure 3:Tönnis classification.
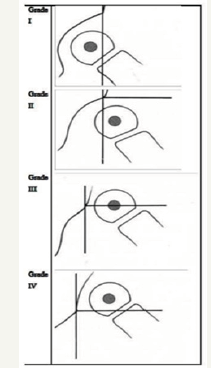
Figure 4:Tönnis classification.
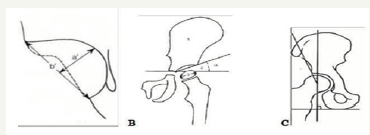
Table 1:Severin classification: Degrees of hip dysplasia and luxation.
Surgical procedures
Two different osteotomies were performed according to the techniques described by the original authors: The Salter osteotomy developed in 1961 [9] and the Pemberton technique, first described in 1965 [10] with intra-operative image intensifier guidance. Plain anteroposterior radiographs of the pelvis were taken immediately after the surgery and at 6 weeks and 3, 6, and 12 months postoperatively.
Femoral osteotomies
Femoral osteotomies were performed mainly in patients with subluxation of the femoral head (Tönnis 3 and 4) derotation was required in a patient with severe femoral torsion. Femurs were shortened an average of 2.5cm (range, 1.5-7cm) and derotation was performed to correct the torsion an average of 30-40° in both groups. Surgical reduction consists of a sequential intervention in which all intra- and extra-articular obstacles are removed and a capsulorrhaphy of the joint capsule to reduce its size is performed, followed by a stage of reduction of the dislocation of the femoral head in the acetabulum. The type of osteotomy is defined at the moment of the reduction. To assess closure of the cartilage, the radiographs were evaluated by two independent radiologists in a blinded fashion. Inter-observer agreement was calculated using the Cohen’s kappa coefficient [4], for inter-observer reliability was the Fleiss method was used, and the kappa coefficient was defined according to the guidelines proposed by Landis & Koch [11].
Statistical Analysis
Continuous variables are expressed as mean and standard deviation, and categorical variables as percentages and absolute frequency. The AI, ADR, Sever in, and CE were measured on preand post-surgical radiographs using a parametric test, the paired samples test, for continuous variables. To assess the differences between the Pemberton and Salter groups, continuous variables were evaluated using the t test or Wilcoxon log-rank test, and categorical variables with the chi-squared test. A p value of less than 0.05 was considered statistically significant. All the analyses were carried out with IBM/SPSS Statistics Version 19 [12].
Ethical considerations and declaration of interest of the authors
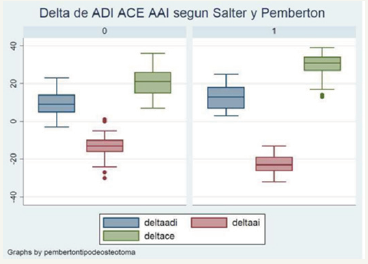
The study was approved by the Ethical Board of Hospital Nacional de Pediatría Prof. J. P. Garrahan. The authors have no conflict of interest to declare. The study received no specific funding. The statistical analysis were performed by an independent statistician specialized in health statistics (Figure 5).
Figure 5:Pre- and postsurgical delta ADI, AI, CE for the Salter (0) and Pemberton (1) osteotomy groups.
Results
In the Salter group, there were 3 Tönnis type II, 11 Tönnis type III, and 35 Tönnis type IV hips. In the Pemberton group there were 9 Tönnis type III, and 38 Tönnis type IV hips. The follow-up was mean 9 years, (range 8-11 years) for the Salter and mean 9 years (range 8-10) for the Pemberton group, with no significant statistical difference between groups (p 0.72) Salter in nominate osteotomy group: Between January 2001 and September 2009, 40 patients with DDH were treated with Salter osteotomy; 32 were girls (39 hips) and eight were boys (10 hips). Nine patients had bilateral dislocations. Overall, 25 were right hips and 24 left hips [13,14]. Mean age of the children at surgery was 34.8 months (SD±12.4; range, 18-68 months). Twenty-five hips (51 %) were treated with femoral shortening and 24 hips (49%) were treated without femoral shortening (Table 2).
Table 2:Baseline features of the patients overall and divided according to osteotomy technique into the Salter or Pemberton groups (n=96).
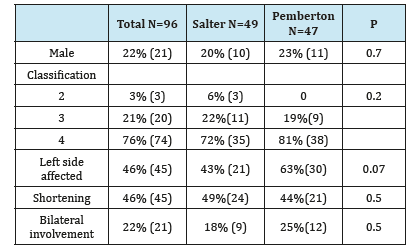
Pemberton osteotomy group: Between January 2000 and December 2010, 40 patients with DDH were treated with Pemberton osteotomy; 31 were girls (36 hips) and nine were boys (11 hips). Ten patients had bilateral dislocation. Of all the hips, 21 were right hips and 29 were left hips. The mean age of the children at surgery was 35.5 months (SD±16.5; range, 18-71 months). Twenty hips (42,55%) were treated with femoral shortening and 27 hips (57.44%) were treated without femoral shortening (Table 2). Of all 96 patients who underwent surgery, in 49% (47) the Pemberton technique and in 51% (49) the Salter technique was used. Twentytwo percent (21) of the children were boys. After the surgery, 64% (62) of the children met the criteria for normal hips: AI: 20 °; CE: 25 ° from 9-12 years and 26-30 ° from 13-20 years, and ADI: 60%. When comparing sex, classification, left hip affected, shortening, and bilateral involvement, no statistical significant differences were found between the Salter and the Pemberton techniques. Nevertheless, the rate of correction of the dysplasia was higher in the Pemberton than in the Salter group (83% vs 45%, respectively; p< 0.001) (Table 2).
Figure 1:Comparison of pre- and postsurgical ADI in both groups.
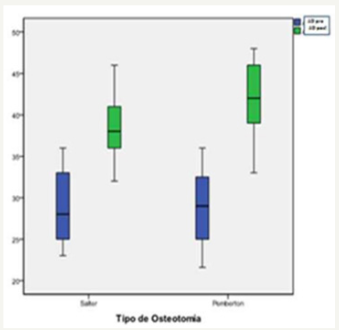
Figure 2:Comparison of pre- and postsurgical AI in both groups.

In the Pemberton group, the mean preoperative ADR was 33° (SD 28°), while in the Salter group it was 29° (SD 4°). The final radiological studies in the Pemberton group showed an ADR of 42° (SD 4°), with an improvement of 9° (SD 27°). In the Salter group, the mean postoperative ADR was 38° (SD 4°), with a total improvement of 9.5° (SD 6°). Finally, when comparing the mean pre- and postoperative change in the ADR between groups, no statistically significant difference was found (p = 0.9) (Graph 1). In the Salter group, mean preoperative AI was 37° (SD 4°), while in the immediate postoperative period mean AI was 24° (SD 4°). In the Pemberton group, the mean preoperative AI was 42° (SD 4°) and the mean early postoperative AI was 19° (SD 3°) (Graph 2).
Figure 3:Comparison of pre- and postsurgical CE in both groups.
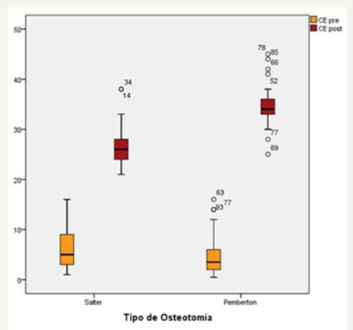
Table 3:Pre and postoperative features of the patients overall and divided according to osteotomy technique into the Salter or Pemberton groups (n=97).
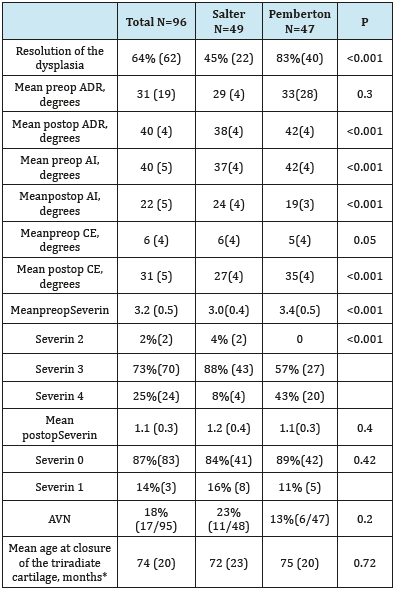
On evaluation of the final X-rays, the mean CE angle of Wiberg was found to measure 34.6° (IQR 25°- 45°) in the Pemberton and 26.7° (IQR 21°-38°) in the Salter group (Graph 3). A statistically significant difference was found in the final measurement of the CE angle between the groups (P< 0.001). Significant differences in pre-and postoperative changes in AI, CE, and Severin between the Pemberton and Salter groups were also found; however, no significant differences were observed in pre- and postop changes in ADI between groups (P > 0.05) (Table 3 & Figure 1). Correction of the dysplasia with normal values (AI: 20°; CE: 25° from 9 -12 years and 26-30° from 13-20 years, and ADI: 60%) was achieved in 40 hips (83%) in the Pemberton group and in 22 hips (45%) in the Salter group, a difference that was statistically significant (P< 0.001- odds ratio 2.17).
The odds ratio shows that the probability of non-correction of the dysplasia was twice as high in the Salter group than in the Pemberton group (Table 3). Premature closure of the tri radiate cartilage occurred in 52% of the hips treated with Pemberton osteotomy compared to 19% of the hips treated with Salter osteotomy seen only in the earliest innominate osteotomies, when a wide exposure of the inner surface of the pelvic bone was used. In these cases, a bony bridge can be observed on the anteroposterior radiograph or on an oblique view at 2 years post-surgery. This observed epiphysiodesis is probably only partial and has as its main consequence a growth disturbance of the obturator for a men.
Table 4:Intra- and interobserver reliability was evaluated using the kappa coefficient.
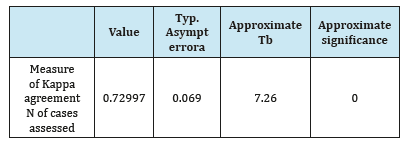
Intra- and interobserver reliability was assessed using the kappa coefficient, which showed it to be good (0.92). For agreement on the definition of cartilage closure a kappa of 0.73 was found (p 0.001) (Table 4). Avascular necrosis (in its different stages) was not present before operation. Therefore, avascular necrosis was observed principally (23%) in the Salter osteotomy group, related to the group without femoral shortening when compared with the Pemberton osteotomy group (13%). Only two patients in the Salter group required triple osteotomy in the final follow-up.
Discussion
Dysplasia of the hip is a public health burden in South America [14]. Early detection of developmental dysplasia of the hip is important in daily practice. Different factors are involved in the disease, such as the availability of physicians, political interest, as well as cultural and demographic factors. The patients in our series are the result of a failure of early identification of the disease and flaws in the health system in the country, which may be explained my multiple factors: The lack of availability of medical doctors in some regions of the country. The lack of clinical examination by a specialized orthopedic surgeon including muscle relaxation or unawareness of clinical signs such as those observed in the Barlow and Ortolani tests, asymmetry of the thigh or gluteal folds, abductor tension, or the late Galeazzi sign.
According to Seringe [13] failure of surgical reduction is due to lack of primary stability. In our series the type of particular osteotomy was defined in the stage in which intraarticular shortening and femoral derotation were performed to correct any excessive anteversion if necessary. Thereby the peri-articular soft tissues relax, allowing joint reduction with adequate tension while reducing the incidence and severity of osteochondritis [14]. After femoral reorientation, it is possible to improve coverage of the femoral head by pelvic osteotomy. Femoral shortening with derotation may facilitate the reduction due to the better alignment and the remodelling of the acetabulum. Nevertheless, we only found a significant difference in the AI in the Pemberton osteotomy, which was even more marked in the subgroup that underwent Pemberton osteotomy combined with femoral shortening.
In this study, we used the acetabular depth to width ratio described by Heymanand [12]. According to Le Damany [10] at birth the ADI is 41%, increasing to approximately 50% at 8 years of age, and to 60-70% in adulthood. In the Pemberton osteotomy, the upper edge of the acetabulum is folded downward, to diminish the acetabular width. The acetabular depth to width ratio changes because of the change in height and depth. Although the depth of the semicircle increases, the width diminishes when Pemberton osteotomy is performed [15]. The main concept here is that the measures of the final proportions in the ratio remain the same. Cummings [16] reported that the Pemberton osteotomy did not alter the acetabular volume, but did improve femoral head coverage through reorientation of the acetabulum rather than changing its shape. Our results agree with this finding. Consequently, the Pemberton osteotomy does not create increased depth, but reorients the acetabular entry hole thereby changing its diameter.
Thus, the Pemberton osteotomy is not indicated when the acetabulum is small in relation to the size of the femoral head. Sankar et al. [1] reported failure of the technique when the femoral head is abnormally large in seven of 22 patients with DDH who underwent open reduction. It is well known that the distal fragment of the iliac bone may exert pressure on the femoral head after Pemberton osteotomy, increasing the risk of osteonecrosis [2]. Conversely, the formation of the acetabular roof in the Salter procedure covers the femoral head shifting the acetabulum forwards, downwards, and outwards to create lateral and anterior head coverage [17] leaving the posterior femoral head uncovered, which is one of the main disadvantages of the technique.
In a review article, Pekmezci [2] reported that if the acetabular insufficiency is mainly supero-lateral or posterior, and the Salter technique is used, the requirements for a well-balanced femoral head containment are not met, anterior coverage is exaggerated, and insufficiency of the supero-posterior coverage will increase. Additionally, recent studies assessing the presence of femoro acetabular impingement (FAI) after performing an innominate osteotomy, found an incidence of around 12% of clinically relevant FAI [3]. A change of more than 20° in the ADI was an independent risk factor for developing FAI after innominate osteotomy for acetabular dysplasia. One of the limitations of our study was that the data were obtained retrospectively from a non-randomized patient sample; however, randomization of patients to obtain more robust results would be extremely complicated in a condition such as DDH.
In conclusion, in the present study comparing two groups of patients treated with either the Pemberton or the Salter osteotomy for DDH, significant differences were found in pre and postoperative changes of AI, CE, and Severin criteria in favor of the former technique after a mean follow-up of 6 years. Iatrogenic damage to the triradiate cartilage is the most disappointing complication of the procedure, possibly leading to a loss of its good results. Several authors reported premature closure of the triradiate cartilage after different types of pelvic osteotomies with satisfactory results [19]. In our series, radiographs showing premature closure of the cartilage were more common in patients who underwent Pemberton osteotomy. Therefore our question was why in spite of this presentation the acetabular coverage was adequate. Acetabular remodelling may occur beyond 10 years of age or after skeletal maturation. Nevertheless, several authors have stated that potential for acetabular remodelling is already minimal at 8 years of age [20]. This would imply that the main cause of a greater dysplasia is not only the iatrogenic damage to the tri radiate cartilage, but also that, after 4 years of age, the wide exposition needed to visualize the surgical field and manipulate the osteotome, reduced flexibility and decreased capacity for remodelling of the iliac bone, as reported by Bohmand Brzuske, may mark the difference in the final results [21]. Dysplasia or osteoarthritis may develop even in patients that underwent these two types of surgeries. Therefore; we are still searching for an ideal solution for DDH [22-24].
Conflict of Interest
Author Dra. Bibiana Dello Russo declares that she has no conflict of interest. Author Candia Tapia Jaime Gregorio declares that he has no conflict of interest. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Sankar WN, Young CR, Lin AG, Crow SA, Baldwin KD, et al. (2011) Risk factors for failure after open reduction for DDH: a matched cohort analysis. J Pediatr Orthop 31(3): 232-239.
- Pekmezci M, Yazici M (2007) Salter osteotomy: an overview. Acta OrthopTraumatolTurc 41(Suppl 1): 37-46.
- Ponseti IV (1978) Growth and development of the acetabulum in the normal child. Anatomical, histological, and roentgenographic studies. J Bone Joint Surg Am 60(5): 575-585.
- Cohen JA (1960) Coefficient of agreement for nominal scales. Educational and psychological measurement 20: 37-46.
- Cummings R (2004) How the Pemberton innominate osteotomy really works: an animal study. J Surg Orthop Adv 13(3): 166-169.
- Mac Ewen GD (1987) Treatment of congenital dislocation of the hip in older children. Clin Orthop Relat Res 225: 86-92.
- Herring JA (2008) Developmental dysplasia of the hip. In: Herring JA (Eds.), Tachdjian’s pediatric orthopaedics. (4th edn.), Philadelphia: WB Saunders pp. 637-770.
- Tonnis D (1987) Congenital dysplasia and dislocation of the hip in children and adults. Berlin: Springer-Verlag pp. 100-142.
- Plaster RL, Schoenecker PL, Capelli AM (1991) Premature closure of the triradiate cartilage: a potential complication of pericapsular acetabuloplasty. J Pediatr Orthop 11(5): 676-678.
- Le Damany P (1904) Le cavité cotylöide. Evolution ontoguenique compare de saaprofondeur chez l homme et les animaux J Anat Physiol 40: 387-413.
- Landis J, Koch G (1977) The measurement of observer agreement for categorical data. Biometrics 33: 159-174.
- Heyman CH, Herndon CH (1950) Legg-Perthes disease: a method for the measurement of them roentgenographic results. J Bone Joint Surg Am 32A(4): 767-778.
- Jacobsen S, Sonne HS, Søballe K, Gebuhr P, Lund B (2005) Hip dysplasia and osteoarthrosis: a survey of 4151 subjects from the Osteoarthrosis Sub study of the Copenhagen City Heart Study. Acta Orthop 76(2): 149- 158.
- Bohm P, Brzuske A (2002) Salter Innominate Osteotomy for the Treatment of Developmental Dysplasia of the Hip in Children: Results of Seventy-Three Consecutive Osteotomies after Twenty-Six to Thirty-Five Years of Follow-Up. J Bone Joint Surg Am 84-A(2): 178-186
- Castañeda P, Vidal RC, Méndez A, et al. (2016) How Often Does Femoroacetabular Impingement Occur After an Innominate Osteotomy for Acetabular Dysplasia? Clin Orthop Relat Res 474(5): 1209-1215.
- Wang CW, Wu KW, Wang TM, Huang SC, Kuo KN (2014) Comparison of Acetabular Anterior Coverage after Salter Osteotomy and Pemberton Acetabuloplasty: a Long-term Follow-up. Clin Orthop Relat Res 472(3): 1001-1009.
- Günal T, Muratli HH, Hapa O, Celebi L, Gülcek S, et al. (2007) Residual axial plane deformities after hip reconstruction for developmental dysplasia of the hip after walking age. J Pediatr Orthop B 16(2): 84-89.
- Mladenov K, Dora C, Wicart P, Seringe R (2002) Natural History of Hips With Borderline Acetabular Index and Acetabular Dysplasia in Infants. J Pediatr Orthop 22(5): 607-612.
- Morin C, Rabay G, Morel G (1998) Retrospective review at skeletal maturity of the factors affecting the efficacy of Salter’s innominate osteotomy in congenital dislocated, subluxed and dysplastic hips. J Pediatr Orthop 18(2): 246-253.
- Pauwels F (1976) Biomechanics of the normal and diseased hip. New York: Springer-Verlag p. 130.
- Pemberton PA (1965) Pericapsular osteotomy of the ilium for treatment of congenital subluxation and dislocation of the hip. J Bone Joint Surg 47: 65-68.
- Raimann A (1961) Enfermedad Luxante de Cadera, Santiago, Editorial iku 2003 pág.13 Salter R.B Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg 43B: 518.
- Staheli LT (1991) Surgical management of acetabulardysplasia. Clin Orthop Relat Res 264: 111-121.
- Severin E (1941) Contribution to the knowledge of congenital dislocation of the hip joint. Late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scandinavica (Suppl 63).
© 2018 Dello Russo Bibiana. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






