- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
Optimization of Approaches to Surgical Treatment of Patients with Acetabulum Fractures Interim Results of the Study
Donchenko SV1, Kolesnik AI2*, Surikov VV1,3, Solodilov IM4, Ivanov DA5 and Yarmamedov DM6
1City Clinical Hospital named after S. P. Botkin, Russia
2Priorov Central Institute for Trauma and Orthopaedics, Russia
3Russian Medical Academy of Continuing Postgraduate Education, Russia
4Regional budgetary health care institution “Kursk city clinical hospital No. 4», Russia
5Lytkarino City Hospital, Russia
6Kursk State Medical University, Russia
*Corresponding author: Kolesnik AI, Priorov Central Institute for Trauma and Orthopaedics, Russia
Submission: February 23, 2022;Published: May 16, 2023

ISSN 2578-0069Volume3 Issue1
Abstract
Background: Dislocated BB fractures and multi-plane fractures are subject to surgical treatment. Open reduction and internal fixation (in foreign literature, the abbreviation ORIF is used-open reduction and internal fixation) remain the standard method of treating fractures of the BB to date. Many authors, in cases of fractures that are predictors of poor results of ORIF use, recommend performing “acute” PE TBS, which, according to the authors, is a “viable long-term solution” to the problem of fracture treatment, especially in elderly patients. Aim. To carry out anatomical and radiological characterization of fractures in order to optimize approaches to surgical treatment of patients and improve its results. Material and methods. For the period from 2009 to 2019 and the hospital treated 53 patients who are diagnosed with 54 fractures of Explosives. The age of the patients ranged from 18 to 71 years. Men predominated-60.4%. All patients received a high-energy injury. Fractures of the front column (29.2%) and both columns (20.4%) prevailed. In patients with BB fractures, fractures of the anterior column (29.2%) and both columns (20.4%) prevailed. Transverse, T-shaped, T-shaped with central dislocation of the hip, anterior column, anterior wall, semi-transverse fracture of the posterior column, fracture of both columns with central dislocation of the hip were detected with approximately equal frequency. Dislocation of the femur was diagnosed in 12 cases (22.2%), half of them had posterior dislocation. GBC damage was detected in 12 cases. Results and discussion. The analysis of the results of X-ray and CT examination of patients allowed us to detail the anatomical and morphological nature of fractures and injuries of the BB and GBC. Patients with BB fractures were divided into two clinical groups, taking into account the nature of anatomical and morphological injuries of the BB and femoral head. Criteria for inclusion and exclusion of patients in clinical groups have been developed. Indications for the choice of the most optimal variant of the surgical treatment method for each individual patient in each clinical group are determined. In the first group of patients, ORIF was performed using standard surgical approaches and submerged fixators or performing percutaneous minimally invasive fracture fixation. In the second group of patients, CHP is indicated. In older patients, preference should be given to performing “acute” PE TBS. Conclusion. The detailing of anatomical and morphological injuries and fractures of the BB and GBC allowed us to identify the features of these injuries, which contributed to the formation of two clinical groups of patients with different types of BB fractures. Criteria for inclusion and exclusion of patients in clinical groups were developed. Hikes have been developed for each clinical group and indications for choosing the most optimal variant of the surgical treatment method have been determined.
Abbreviations:Acetabulum fractures and their classification; Open reposition and internal fixation; Acute primary hip replacement
Introduction
The urgency of the problem of treatment of acetabulum fractures is due to the increase in road injuries, the increased severity of this injury, the complexity of surgical treatment complications arising both in the pre- and postoperative periods [1- 6], at the same time, the frequency of BB fractures ranges from 2% [5] to 22% [1] with a tendency to increase the number of fractures [5,7]. Butterwick et al. [8] It is noted that geriatric patients are the fastest growing subgroup of patients with BB fractures, while the frequency of its fractures in patients over sixty years of age has increased 2.4 times over the past quarter century [8]. It is believed that dislocated BB fractures and multi-plane fractures are subject to surgical treatment [1,9-12]. Open reduction and internal fixation (the abbreviation ORIF is used in foreign literature-open reduction and internal fixation) remain the standard method of treatment of BB fractures to date [12-16]. Letournel [9], wrote that the ideal open reposition is the method of choice for the treatment of dislocated BB fractures [9]. In their research, the authors note that to date, the principle of direct anatomical reposition of columns and fragments of explosives with fixing screws and neutralizing plates remains the leading one in the treatment of fractures of explosives [9,15-19]. Achieving anatomical reposition and stable fixation when performing ORIF provides the patient with the possibility of early rehabilitation [17]. It is known that the typical pattern of a BB fracture in younger patients is damage to the posterior column and the posterior wall. For persons 50 years and older, fractures of the anterior column involving a quadrangular (quadrolateral) plate (surface) with a central dislocation of the femoral head are more often diagnosed [19-24]. The peculiarities of the nature of BB fractures, making changes in approaches to surgical treatment, pose new challenges for the effective solution of the problem when performing ORIF [25-30]. Poor results the outcomes of the use of ORIF (Open Reduction & Internal Fixation) in elderly patients incline researchers to consider the use of a combination of ORIF and Primary Endoprosthetics (PE) TBS-an approach called “combined hip procedure” (Combined Hip Procedure-(CHP) [18,21-24]. Currently, there is a growing interest in performing PE TBS, since this treatment provides advantages in qualitative stabilization of the fracture and while minimizing damage to soft tissue formations, rapid and significant reduction of pain syndrome, the possibility of early mobilization of the patient [7,17,25,26,31-41]. Goal To carry out anatomical and radiological characterization of fractures in order to optimize approaches to surgical treatment of patients and improve its results.
Material and Methods
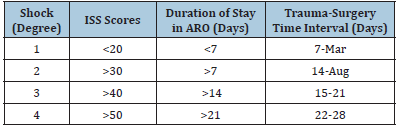
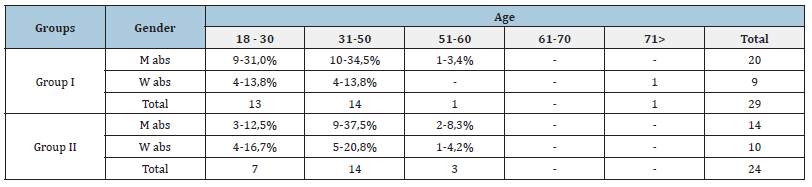
The work was performed in the department of Traumatology of the Botkin City Clinical Hospital (hereinafter referred to as the LPU). For the period from 2009 to 2019 and the hospital treated 53 patients who are diagnosed with 54 fractures of explosives. The age of the patients ranged from 18 to 71 years (Table 1), while most of the victims were aged from 18 to 50 years. Men predominated-60.4%. There were no BB fractures in patients in the age range from 61 to 70 years. In our work, we used the “Patient Database” of the Botkin City Clinical Hospital, which has been maintained on an ongoing basis since its establishment in 2015. Clinical data such as gender, age, date of injury and hospitalization, mechanism of injury, classification of BB fractures and associated injuries (hip dislocation) are recorded during admission and examination of patients included in the study. All patients received high-energy trauma in road traffic accidents-37 cases fell from a height-16. First day of LPU 47 hospitalized patients, of which 21 patients were taken to hospitals by ambulance, 17-ambulance (emergency hospital), 9-by passing cars, and 6 patients transferred from other institutions or emergency hospital by ambulance. The vast majority of patients (47) were taken to the institution in a state of shock: (I degree-21, II degree-18, III degree-5, IV degree-3) (Table 2).
Table 1:Distribution of patients with fractures in B by gender and age.
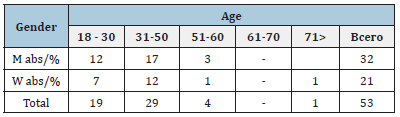
Table 2:Characteristics of the condition of patients with fractures in the V at admission to the medical center.
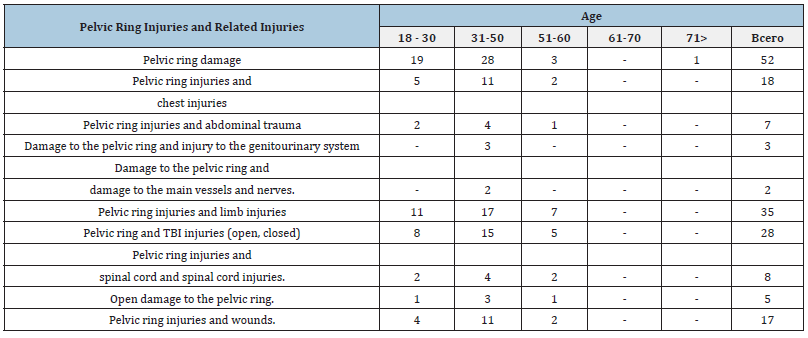
Concomitant injuries in persons with pelvic fractures are presented in Table 3. In accordance with the set goals and objectives of the study, we conducted a comprehensive examination of 53 patients with fractures of the BB treated in the hospital of the institution. Standard X-ray examination was carried out as soon as possible. All patients underwent an overview image in two or 3 projections. Antero-posterior projection with the direction of the tube to the entrance to the pelvis (inlet), and the direction of the tube to the exit from the pelvis (outlet) Oblique locking and iliac projections were also performed at an angle of 45 degrees. To identify damage to the load zone of explosives, the arched angle was determined on radiographs in a straight line and two oblique projections. According to JM Matta [42], with a value of less than 45 degrees, surgical treatment is indicated in case of congruence violation in TBS [32,42]. Intraoperative control was performed using an electron-optical converter. Postoperative quality control of the performed reposition and fixation of fractures of the BB was carried out using X-ray and CT examination on the 7th-12th day after the operation. When performing control studies, the following indicators were evaluated: the number of residual dislocations of fragments, the correctness of the position of plates and screws, the presence of foreign bodies (bone fragments, screws) in the joint cavity. The reposition was considered anatomical in cases when the magnitude of all residual displacements on radiographs in three standard projections and on CT did not exceed 0-1mm. In order to determine the quality of the performed reposition of the performed osteosynthesis of acetabulum fractures, we used the main criteria for the satisfactory position of the fragments:
Table 3:Concomitant injuries diagnosed in victims with pelvic ring damage.
a) The value of the residual displacement of fragments on any of
the three projections for simple types of fractures is no more
than 1mm, and for complex types no more than 2-3mm.
b) The residual displacement of fragments within the load zone
does not exceed 1mm.
c) The distance between the lower edge of the femoral head and
the figure of the tear on both sides is the same, which indicates
the absence of a dislocation of the head.
d) The articular surfaces of the femoral head and the roof section
of the acetabulum within the 45o arch angle in all three
projections should be strictly parallel.
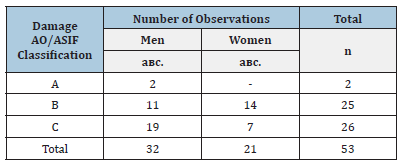
To assess the correctness of the position of the fixing plates and screws, the radiographic method was not absolutely reliable (the presence of a possible error in the patient’s laying during the examination). In cases when the screw did not cross the joint gap in any of the three projections, the position of the screw was considered correct. The analysis of primary radiographs made it possible to predict the tactics of treatment of patients in the first minutes, to clarify the need and timing of CT with 3D reconstruction of the pelvis and TBS, and the subsequent need for MRI of TBS. For convenience, the distribution of pelvic fractures of patients was carried out according to the AO/ASIF classification (Table 4).
Table 4:Pelvic ring injuries detected in hospitalized victims.
Research and Result
Based on the analysis of X-ray and CT examination of patients BB fractures were interpreted taking into account the classification according to R. Judet, J. Judet, 1964 [34], and Letournelle E [9], included 5 elementary and five associated fractures, as described by Letournel [9], distributed as follows (Table 5). Fractures of the anterior column (25.5%) and fractures of the anterior column +/ or anterior wall/ semi-transverse fracture of the posterior column (12.7%) prevailed. With approximately equal frequency (7.3- 9.1%), transverse, T-shaped, T-shaped with central hip dislocation, fracture of both columns with central hip dislocation were detected. Dislocation of the femur was diagnosed in 12 cases (21.8%), and only in 2 cases posterior dislocation was noted. Femoral head fracture was detected in two cases (3.6%).
Table 5:BB fractures classified by E Letournel [9].
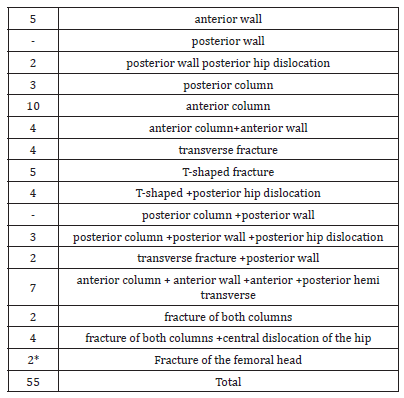
*- *- femoral head fractures are not included in the number of BB fractures.
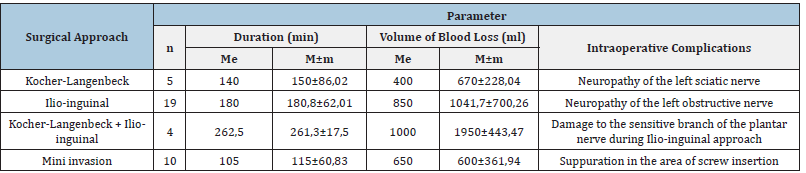
All patients underwent surgical treatment-open reposition and internal fixation of ORIF, which remains to date the “gold standard” for the treatment of fractures of the BB [33,34], which was carried out using various plates: neutralizing, neutralizing with angular stability, or reconstructive pelvic. Surgical access depended on the nature of the diagnosed fracture. With fractures of the posterior column, the posterior wall of the BB, or with their combined damage, the Kocher-Langenbeck access was used, with transverse fractures of the BB and its anterior column, the ilioinguinal access and its modifications were used. The results of ORIF execution are presented in Table 6. We have accumulated our own extensive experience in surgical treatment of BB fractures and performing ORIF. Attention is drawn to the features of BB fractures encountered in the analysis of X-ray and CT data in the preoperative period and during surgical interventions, namely, the presence of different variants of fractures of the tetrahedral plate (surface) of the BB, GBC, and posterior wall. The revealed features of BB fractures, as practice has shown, caused certain technological difficulties, both when performing an operative manual and in the selection of implants for fixing fractures, which is consistent with the data of the literature studied [35,36].
Table 6:Results of ORIF execution.
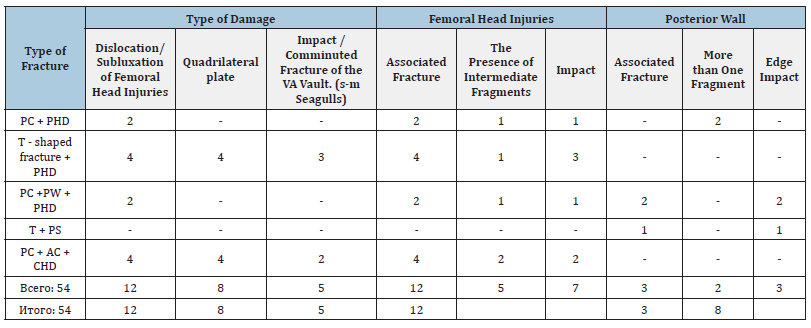
A more thorough anatomical and morphological analysis of the data of X-ray and CT examination of BB and GBC injuries of patients was carried out, which revealed the nature and features of these injuries (Table 7). Table 7 presents the radiological features of BB fractures, which we considered criteria for inclusion of patients in the second clinical group. The results of the analysis of the X-ray and CT examination of the anatomical and morphological characteristics of fractures of BB and GBC were an objective basis for the identification of two clinical groups of patients differing in anatomical and morphological characteristics of the identified fractures. Taking into account the revealed anatomical and morphological characteristics of fractures. In the course of the study, the diagnosed fractures of BB and GBC were developed inclusion and exclusion criteria for the formation of two clinical groups (Table 7).
Table 7:Revealed radiological features of BB and GB fractures.
The purpose of distinguishing two clinical groups was the
need for a more in-depth understanding of the identified features
of anatomical and morphological characteristics of BB and GBC
fractures for subsequent clarification of indications for choosing
the most optimal, individually selected variant of the surgical
treatment method for each individual patient with BB and GBC
fractures in each clinical group to improve early, medium-term and
long-term results of surgical treatment and social adaptation of
patients.
Inclusion criteria for the formation of the first clinical group:
A. The age of patients from 18 to 70 years and older.
B. Closed fractures of the acetabulum with displacement.
C. The time between injury and surgery is from 1 to 2, but not
more than 3 weeks.
D. The patient’s consent to participate in a strict protocol of
observation and rehabilitation.
Inclusion criteria for the formation of the second clinical group:
a) The age of patients from 18 to 70 years and older.
b) Closed fractures of the acetabulum. Fractures of the BB and
GBC, which are prognostically bad signs for performing ORIF.
c) Closed comminuted/multi-comminuted fractures of explosives
with a significant displacement of fragments.
d) The presence of radiological symptoms of a complex fracture
of the BB as a “Seagull symptom (Gull sign), fracture of the
quadrangular plate (surface) BB with displacement, the impact
of the walls of the BB.
e) Closed comminuted/multi-comminuted fractures with
significant displacement of fragments and defects in the walls
of explosives.
f) Fractures and impaction of the femoral head.
g) Damage to the cartilage of the BB and the femoral head (with
and without impact of the subchondral zone).
h) The time between injury and surgery is from 1 to 2, but not
more than 3 weeks.
i) The patient’s consent to participate in a strict protocol of
observation and rehabilitation.
Exclusion criteria for the formation of the first and second
clinical groups:
A. Conservative treatment of patients (skeletal traction).
B. Existing chronic infection in remission or exacerbation.
C. Severe comorbid pathology.
D. Polyvalent intolerance to antibiotics.
E. Open fractures of the acetabulum.
F. Pathological fractures of the acetabulum.
G. Patients who refused surgery.
A targeted comprehensive clinical and instrumental study of 53 patients allowed the formation of two clinical groups, the first-the main group and the second-the comparison group (Table 8).
Table 8:Distribution of patients with BB fractures by gender and age in the first and second clinical groups.
Statistical analysis. Statistical processing of the results of the study was carried out by calculating the values of the arithmetic mean (M), the mean square deviation (δ), the standard error of the arithmetic mean (m). The presence of deviations from the Gaussian distribution was detected using the Kolmogorov criterion. In the absence of deviations from the Gaussian distribution curve, the presence of statistically significant differences was calculated using the student’s criterion (p≤0.05).
Discussion of the Results
It is necessary to note the following important points of our research. In order to obtain reliable data on BB fractures during the procedure, which are poor prognostic signs (factors, predictors) in obtaining unfavorable results of surgical treatment using ORIF, we excluded from the study patients whose X-ray examination did not include three pelvic projections and there were no CT examination data. The obtained X-ray and CT images of 53 patients were evaluated by both specialists in radiation diagnostics and an orthopedic traumatologist specializing in the treatment of BB fractures.
All radiographs and CT sections with 3D reconstruction of each patient were carefully studied to identify the features of the nature of fractures, which are prognostically bad signs for performing ORIF. In addition, experts assessed the direction of displacement/ dislocation of the GBC, the presence or absence of a single or several fragments of a fracture of the quadrangular plate (surface) of the BB. Based on the performed anatomical and radiological analysis, the features of the nature of BB and GBC fractures were studied with the identification of a separate group of fractures that are prognostically poor predictors/signs in obtaining unfavorable results of surgical treatment using ORIF [37-39]. All analyzed fractures of BB and GBC (Table 5), including fractures that are prognostically poor predictors/signs in obtaining unfavorable results of surgical treatment of patients using ORIF (Table 7), formed the basis for the development of criteria for inclusion and exclusion of patients for the formation of 2 clinical groups (Table 8). The criteria for inclusion in the first group include elementary and associated fractures of the BB, classified according to Letournelle [9], (Table 5). The criteria for inclusion in the second group include fractures that are prognostically poor predictors in obtaining unfavorable results of surgical treatment of patients using ORIF (Table 7). The exclusion criteria for both groups were the same. In both groups (Table 5), there were no significant differences in the mechanism of injury, age, severity of the condition at admission and the timing of hospitalization.
The first clinical group included patients with fractures of EXPLOSIVES, classified by Letournel [9] with five simple and five associated fractures, which are presented in (Table 5). The second group included patients with more complex fractures associated BB GBK-fractures, which are prognostically poor predictors of the receipt of the adverse results of surgical treatment of patients with the use of ORIF (Table 7). The presence of formed 2 clinical groups with different types of fractures of BB and GBC dictated the need to clarify the indications for choosing the most optimal surgical treatment option for each patient in each clinical group. In this regard, we have developed and justified approaches to the surgical treatment of patients of each group aimed at improving the anatomical and functional results of treatment.
Thus, in the first group of patients, BB fractures classified according to Letournel [9] with five simple and five associated fractures, presented in (Table 5), are indications for performing ORIF using standard surgical approaches and immersion fixators, taking into account the clinical condition of each patient individually [40-43]. In patients of this group, fixation of fractures can be performed by means of a skin mini-invasive technique, taking into account a strictly individual approach [44]. Treatment of BB fractures with ORIF should be a priority and be the first in the list of methods of surgical treatment of the attending physician (operating traumatologist-orthopedist) of the patient [32,45,46]. However, the characterization of the nature of fractures of the BB and GBC, the identification of unfavorable prognostic signs of the outcome of surgical treatment obliges the attending physician (operating traumatologist-orthopedist) in the need to revise approaches in the selection of surgical treatment and consideration of alternative methods of treatment [20,32,45,47]. As practice and literature data show, there is a subgroup of patients in whom combined internal fixation with acute hip replacement (CHP) may be a more appropriate treatment option. Thus, in the second group of patients in whom fractures are poor prognostic signs (factors), CHP may be preferred for the use of ORIF. This is directly related to the patient’s factors (including age, osteoporosis, obesity), the nature of fractures, which often include a comminuted and depressed fracture of the dome or posterior wall, a depressed subchondral fracture of the GBC, as well as external factors that include prolonged dislocation of the femur, or not the effectiveness of conservative treatment with persistent displacement of fragments [21-23,44,48]. Eg, Ortega et al. [24] indicate that CHP is the only way to treat patients, especially the elderly [24]. Many authors hold the same opinion [26,44,46,49-51]. At the same time, [52] indicates that a complex CHP procedure is best performed by a surgical team with significant experience in both the surgical treatment of BB fractures and TBS Endo-prosthetics [53,54].
In older patients with existing concomitant diseases, preference should be given to performing “acute” PE TBS [51]. Belch et al. [34], indications for “acute” PE include closed unstable fractures of the posterior and anterior columns, in combination with wall fractures, multi-splintered fractures with the inability to reconstruct, GBC fractures, while the authors emphasize that it is the nature of the BB fracture that is the main indication for “acute” PE [33]. Other authors also adhere to similar indications for performing “acute” PE [29,31,32,36,38,52]. It is necessary to pay attention to the emphasis made by Sierra et al. [55], with regard to the age of patients, that in cases of a comminuted fracture with incomplete reposition of BB fragments, “acute” PE is shown in patients older than 40 years [54]. In a recent paper by Antell et al. [54], the authors noted that the indications for “acute” PE TBS are based on the nature of the fracture of the BB and are not limited to the age of the patient [53].
Ortega et al. [24] recommend performing “acute” PE TB, which, according to the authors, is a “viable long-term solution” to the problem of fracture treatment, especially in elderly patients. At the same time, the authors draw attention to the need for preliminary stabilization of the columns of explosives [24].
In approaches to the surgical treatment of patients of the 2nd clinical group, and in particular, with regard to the implementation of “acute” PE TB, we adhere to the following requirements and conditions, namely: 1-a Collective Optimal strategy for the treatment of the patient should be developed, where “acute” PE TB should be determined as the most beneficial method of surgical treatment for a particular patient, the key principle of which is to achieve maximum reposition of columns and fragments of explosives and to ensure the primary stability of the acetabulum component of the endoprosthesis; 2-The patient must: consent (in writing) to this operation, know why this particular operation is proposed, know about the advantages and disadvantages of the proposed operation; 3-Consent to participate in further ongoing research (periodic examinations to assess the results of treatment in dynamics, filling out questionnaires, working with questionnaires); 4-An orthopedic traumatologist with experience in surgical treatment of BB fractures and TBS endo prosthetics should be part of the surgical team (this may be one specialist); 5-The team’s specialists should be ready: to perform the replacement of BB defects, to make the right choice of the implant in a specific situation of damage and the nature of the fracture; 6-In the arsenal of the surgical team, in addition to the “line” of TBS implants, there should be implants for fixing fractures and fragments of BB columns, augments and material for replacing BB defects; 7-the risk of complications from the surgical aid used should not exceed the expected effectiveness of surgical treatment [55].
By definition, the indications for the choice of one or another method of surgical treatment should be strictly individual with maximum minimization of the grammaticity of the surgical aid, aimed at reducing the risk of a threat to the patient’s life, with mandatory consideration of the biological age of the patient, the presence of concomitant diseases, the patient’s consent to a specific surgical treatment and the patient’s subsequent participation in the study. It is known that the choice of surgical access directly depends on the nature of the fracture of the BB, while taking into account the preferences of the surgeon and his practical experience. The ilio inguinal access, Kocher-Lange beck access, Stop, modified Stop, less often ilio-femoral and Harding access have been widely used in the practice of surgical treatment of BB fractures [9,15,18,34,40,41].
According to Hanschen et al. [26] and Anglen [56], stable fixation of the BB is achieved using reinforcing rings, cups with a large number of holes, and augments without internal fixation of the fracture, or, with preliminary reposition and internal fixation of the columns of the BB without restoring its articular surface, followed by fixation of the acetabulum component to the restored pelvic anatomy [17,55]. Butterwick et al. [8] argue that it is possible to achieve stable fixation of columns and fragments of explosives only by using reinforcing rings that are attached directly to the intact part of the ilium [8]. Other authors hold the same view [17,25,57,58].
Conclusion
A. In all patients, BB fractures were the result of a high-energy
injury received: as a result of road accidents in 37 cases,
when falling from a height-in 16 cases. The vast majority of
patients (47) were taken to the institution in a state of shock:
(I degree-21, II degree-18, III degree-5, IV degree-3).
B. The main number of patients (47) were hospitalized on the
first day, of which 21 patients were taken to the medical facility
by a reanimobile, 17 by an ambulance team (BSMP), 9 by
passing transport and 6 patients were taken from other BSMP
institutions or by a reanimobile.
C. Fractures of the anterior column (29.2%) and both columns
(20.4%) prevailed among the fractures of the BB. Transverse,
T-shaped, T-shaped with central dislocation of the hip,
anterior column, anterior wall, semi-transverse fracture of
the posterior column, fracture of both columns with central
dislocation of the hip were detected with approximately equal
frequency. Dislocation of the femur was diagnosed in 12 cases
(22.2%), half of them had posterior dislocation. GBC damage
was detected in 12 cases.
D. The anatomical and morphological detailing of the data of the
results of X-ray and CT examination of the injuries of the BB
and GBK patients revealed the peculiarities of the nature of
the fractures of the BB: variants of fractures of the tetrahedral
plate-14.8%, impact/comminuted fracture of the vault of the BB
(s-m Seagull)-9.3%, impact and different variants of fractures
of the GBK-22.2%, poly fragmentary fracture and impact of the
posterior edge of the BB-9.3%, which are predictors of poor
results of surgical treatment with the use of ORIF.
E. The development and implementation of inclusion and
exclusion criteria contributed to the formation of two clinical
groups of patients with different types of BB fractures was an
objective justification for the development of indications for
choosing the most optimal option for surgical treatment for
each individual patient in each clinical group.
F. For the first group of patients, the anatomical and morphological
nature of BB fractures is an indication for performing ORIF
using standard surgical approaches and immersion fixators or
performing percutaneous minimally invasive fracture fixation.
In the second group of patients, the presence of fractures with
poor prognostic signs dictates the use of either CHP, including
ORIF with “acute” PE TB, or only the implementation of “acute”
PE TB.
Factors Affecting Success
Late or delayed PJI treated with DAIR are significantly associated with failures [21]. Poor general condition of patients, high preoperative C-reactive protein level, repeated joint surgeries and Methicillin-resistant Staphylococcus aureus (MRSA) infections are associated with lower DAIR success rate. On the other hand, early surgery, radical debridement, exchange of removable components, wash with iodine and vacuum dressing may improve success rate of DAIR [22]..
Conclusion
DAIR procedure can be a successful treatment option for PJI. It can achieve infection eradication in the majority of patients. The most important factors influencing success are timing of DAIR from onset of symptoms and exchange of modular components at the time of debridement surgery. The studies reporting on outcomes of DAIR in PJI are mostly retrospective in nature with small cohorts. Prospective studies are necessary for better understanding of the role of DAIR in the management of PJI.
References
- Grin AA, Runkov AV, Shlykov IL (2014) The choice of surgical access in the treatment of two-column fractures of the acetabulum. Traumatology and Orthopedics of Russia 1(71): 92-97.
- Lazarev AF, Solod EI, Gudushauri YG, Kakabadze MG, Stoyukhin SS, et al. (2013) Problems of treatment of acetabulum fractures. Vestn Traumatology and Orthopedics 4: 81-85.
- Bondarenko BA, Kruglykhin V, Plotnikov A, Voitenko N, Zhmurkov A (2014) Features of treatment of pelvic injuries in polytrauma. Polytrauma 3: 46-57.
- Beletskiy AV, Voronovich AI, Murzich AE (2010) Determination of indications to surgical treatment and choice of surgical approaches in complicated complex acetabular fractures. Nn Priorov Journal of Traumatology and Orthopedics 17(4): 30-37.
- Borrelli J, Anglen JO (2018) Endoprosthetics for the treatment of fractures in elderly patients. ©Springer Nature, Switzerland.
- Solod EI, Lazarev AF, Lazarev AA, Gudushauri YG, Kakabadze MG, et al. (2009) Possibilities of surgical treatment of acetabulum fractures using minimally invasive technologies. Vestn Traumatology and Orthopedics 2: 3-9.
- Cecil A, Yu JU, Rodriguez VA, Sima A, Torbert J, et al. (2020) Outcomes of acetabulum fractures with high and low energy in old age. Geriatric Orthopedic Surgery and Rehabilitation, p. 11.
- Butterwick D, Papp S, Gofton W, Lew A, Beaulieu PE (2015) Acetabulum fractures in the elderly: Assessment and treatment. Joint Surgery J 97(9): 758-768.
- Letournelle E (1980) Acetabulum fractures: Classification and treatment. Clin Orthop Relat Res 151: 81-106.
- Meisters AML, Kraima J, Banyerink H, Spad KH, Vries JPM, et al. (2019) Introduction of a three-dimensional computed tomography method for measuring acetabulum fractures. Plos One 14(6): e0218612.
- Tsai L, Lu Yu, Guo H, Wang I (2017) Surgical treatment of unstable pelvic fractures with concomitant acetabulum fractures. International Orthopedics 41(9): 1803-1811.
- Magu NK, Gogna P, Singh A, Singla R, Rohilla R, et al. (2014) Long-term results after surgical treatment of fractures of the posterior wall of the acetabulum. Journal of Orthopedics and Traumatology 15(3): 173-179.
- Chegurov OK, Menshchikov IN (2018) Treatment of acetabulum injuries and their consequences (literature review). Genij Ortopedii 24(1): 95-101.
- Wally KS, Appleton PT, Rodriguez EK (2017) Comparison of outcomes of operative versus non-operative treatment of acetabular fractures in the elderly and severely comorbid patient. Eur J Orthopedic Surgical Traumatology 27(5): 689-694.
- Wang P, Zhu H, Xu P, Zhang Y, Wang L, et al. (2016) Modified ilioinguinal approach in combined surgical exposures for displaced acetabular fractures involving two columns. Springer Plus 5(1): 1602.
- Solod EI, Lazarev AF, Gudushaury YG, Kakabadze MG, Stoyukhin SS, et al. (2014) Modern possibilities of acetabulum osteosynthesis. Vestn Traumatology and Orthopedics 2: 25-32.
- Resch H, Krappinger D, Moroder P, Auffart A, Blout MA, et al. (2017) Treatment of acetabulum fractures in elderly patients- introduction of a new implant for primary total hip replacement. Archives of Orthopedic and Traumatological Surgery 137(4): 549-556.
- Zagorodny NV, Kolesnik AI, Lazarev AF, Solod EI, Ochkurenko AA, et al. (2020) Modern trends in surgical treatment of patients with pelvic and acetabulum injuries (literature review). The Genius of Orthopedics 26(2): 266-274.
- Voloshin VP, Onoprienko GA, Zubikov VS, Martynenko DV (2008) Surgical treatment of trans vertebral fractures of the pelvic bone. Almanac of Clinical Medicine 19: 37-42.
- Tile M, Helfet DL, Kellam JF, Vrahas M (2015) Fractures of the pelvis and acetabulum: Principles and methods of management. In: (4th edn), JSC Fund Stuttgart: Georg Tim Verlag, Georgia, USA.
- Borg T, Hernefalk B, Heiler NP (2019) Acute total hip replacement in combination with internal fixation in fractures with displacement of the acetabulum in the elderly: a short-term comparison with internal fixation alone in at least two years. Bone Joint J 101-B(4): 478-483.
- Herskovichi DJ, Lindwall E, Bolhofner B, Scaduto JM (2010) The combined hip procedure: Open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthopedic Trauma 24(5): 291-296.
- Rickman M, Young J, Bircher M, Pierce R, Hamilton M (2012) Treatment of complex acetabulum fractures in elderly people with fracture fixation and primary total hip replacement. Eur J Trauma Surgery 38(5): 511-516.
- Ortega Briones A, Smith S, Rickman M (2017) Acetabulum fractures in the elderly: Medium-term results of spinal stabilization and primary endo prosthetics. International Organization for Biomedical Research, pp. 1-6.
- Lont T, Nieminen J, Reito A, Pakarinen TK, Payamaki I, et al. (2019) Total hip replacement in combination with a strengthening ring and a covering of the posterior column for acetabulum fractures in elderly patients: A good result in 34 patients. Acta Orthopaedica, pp. 1-10.
- Hanschen M, Wagner PH, Bibertaler P (2017) Treatment of acetabulum fractures in elderly patients. SICOT-J 3: 37.
- Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD (2014) Acetabulum fractures in patients aged > 55 years: A systematic review of the literature. Bones and Joints Journal 96-B(2): 157-163.
- Salar N, Bilgen MS, Bilgen OF, Ermutlu S, Eken G, et al. (2017) Total hip replacement in acetabulum fractures: Early application. Ulus Acyl Injury Serrahi Derg 23(4): 337-342.
- Helfet DL, Borrelli J, DiPasquale T, Sanders R (1992) Stabilization of acetabulum fractures in elderly patients. J Bone Joint Surgery 74(5): 753-765.
- Salama U, Musa S, Khalefa A, Slim A, Kenavi M, et al. (2017) Simultaneous open reduction and internal fixation and total hip replacement for the treatment of osteoporotic fractures of the acetabulum. Int Orthop 41(1): 181-189.
- Tempelere S, Devine P, Bege T (2019) Early simultaneous bilateral total hip arthroplasty for the management of bilateral acetabular fracture in an elderly patient. Arthroplast Today 5(2): 139-144.
- Saxer F, Studer P, Jacob M (2011) Open stabilization and primary hip arthroplasty in geriatric patients with acetabular fractures: combination of minimally invasive techniques. Unfallchirurg 114(12): 1122-1127.
- Manson TT (2020) Open reduction and internal fixation plus total hip arthroplasty for the acute treatment of older patients with acetabular fracture: Surgical techniques. Orthop Clin North Am 51(1): 13-26.
- Belch SP, Jordan MS, Meffert RH, Jansen H (2017) Comparison of open reduction and internal fixation and primary total hip replacement for osteoporotic acetabular fractures: A retrospective clinical study. Int Orthop 41(9): 1831-1837.
- Negrin LL, Seligson D (2017) Results of 167 consecutive cases of acetabulum fractures using the Kocher-Langenbeck approach: A series of cases. J Orthop Surg Res 12(1): 66.
- Anglen JO, Bird TA, Hendricks KJ, Harrison P (2003) The "Gull Sign": A harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthopedic Trauma 17(9): 625-634.
- Kreder HY, Rosen N, Borhoff SM, Laflamme YG, McKee MD, et al. (2006) Factors determining the functional outcome after simple and complex acetabulum fractures involving the posterior wall. J Bone Joint Surgery 88(6): 776-782.
- Ferguson TA, Patel R, Bhandari M, Matta JM (2010) Fractures of the acetabulum in patients aged 60 years and older: An epidemiological and radiological study. J Bone Joint Surg Br 92(2): 250-257.
- Mears DK, Shirahama M (1998) Stabilization of an acetabular fracture with cables for acute total hip arthroplasty. J Arthroplasty 13(1): 104.
- Tannast M, Najibi S, Matta JM (2012) Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. The Journal of Bone and Joint Surgery American 94(17): 1559-1567.
- Letournel E (1993) The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res (292): 62-76.
- Matta JM (1996) Fractures of the acetabulum: Accuracy of reduction and clinical results in patients managed operatively within three weeks after injury. J Bone Joint Surg Am 78(11): 1632-1645.
- Harris AM, Althausen P, Kellam JF, Bosse MJ (2008) Simultaneous anterior and posterior approaches for complex acetabular fractures. J Orthop Trauma 22(7): 494-497.
- Xue Z, Qin H, Ding H, An Z (2016) A novel approach for treatment of acetabular fractures. Medical Science Monitor 22: 3680-3688.
- Ward AJ, Chesser TJ (2010) The role of acute total hip arthroplasty in the treatment of acetabular fractures. Injury 41(8): 777-779.
- Bhandari M, Matta J, Ferguson T, Matthys G (2006) Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br 88(12): 1618-1624.
- Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD (2014) Acetabular fractures in patients aged >55 years: A systematic review of the literature. The Bone & Joint Journal 96-B(2): 157-163.
- Ziran N, Soles GLS, Matta JM (2019) Outcomes after surgical treatment of acetabular fractures: A review. Patient Safety in Surgery 13: 16.
- Boraiah S, Ragsdale M, Achor T, Zelicof S, Asprinio DE (2009) Open reduction internal fixation and primary total hip arthroplasty of selected acetabular fractures. Journal of Orthopaedic Trauma 23(4): 243-248.
- Pagenkopf E, Grosse A, Partal G, Helfet DL (2006) Acetabular fractures in the elderly: Treatment recommendations. HSS J 2(2): 161-171.
- Sermon A, Broos P, Vanderschot P (2008) Total hip replacement for acetabular fractures. results in 121 patients operated between 1983 and 2003. Injury 39(8): 914-921.
- Mears DC, Velyvis JH, Chang CP (2003) Displaced acetabular fractures managed operatively: Indicators of outcome. Clinical Orthopaedics and Related Research 407: 173-186.
- Yang Z, Röhrl S, Nordsletten L (2019) Displaced acetabular fracture in elderly patients: Is acute arthroplasty an effective option? Z Orthop Unfall 157(6): 676-683.
- Antell NB, Switzer JA, Schmidt AH (2017) Management of acetabular fractures in the elderly. J Am Acad Orthop Surg 25(8): 577-585.
- Sierra RJ, Mabry TM, Sems SA, Berry DJ (2013) Acetabular fractures: The role of total hip replacement. The Bone & Joint Journal 95-B(11_Supple_A): 11-16.
- Anglen JO (2018) Arthroplasty for the treatment of fractures in the older patient. In: Anglen JO, Borrelli J (Eds.), J Arthroplasty for the Treatment of Fractures in the Older Patient. ©Springer Nature, Switzerland.
- (2020) Patent 2723765. Bull. 17, 24.c
- Harding K (1982) The direct lateral approach to the hip. J Bone Joint Surg 64(1): 17-19.
© 2023 Kolesnik AI. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






