- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
Assessment of Typical Trochanteric Fracture Line of the Femur by Three- Dimensional Computed Tomography
Takashi Hisatome* and Kazuyoshi Nakanishi
Department of Orthopedic Surgery, Nihon University Hospital, Japan
*Corresponding author: Takashi Hisatome, Department of Orthopedic Surgery, Nihon University Hospital, Tokyo, Japan
Submission: September 21, 2022;Published: October 06, 2022

ISSN 2578-0069Volume3 Issue1
Abstract
Purpose: The purpose of this study is to consider the complicated fracture line in trochanteric fractures
of the femur by three-dimensional computed tomography (3DCT).
Methods: 80 cases of trochanteric fracture of the femur, Type 1 according to the Evans Classification were
targeted and the fracture line of 80 joints was considered in detail by 3DCT.
Results: The fracture line of a trochanteric fracture is comprised of a primary fracture line which is considered
to be the standard fracture line and a secondary fracture line which occurs afterwards. The anterior
section of the primary fracture line runs from the trochanteric fossa in the frontward direction, passing
through the lateral intertrochanteric eminence and then inward and downward along the intertrochanteric
line. The posterior section of the primary fracture line occurs at the insertion of the ischiofemoral
ligament adjacent to the trochanteric fossa and goes in the upward direction of the lesser trochanter along
the intertrochanteric groove and connects to the anterior fracture line. In most cases of a secondary fracture
line, the fracture runs from upper edge of the lateral intertrochanteric eminence outwardly, traveling
from upper front of the greater trochanter towards the lesser trochanter, causing a greater trochanter
fracture or lesser trochanter bone fragment.
Conclusion: The primary fracture line occurred along the attached area of the capsular ligaments. The
posterior section of the primary fracture line is especially characteristic and is a very important factor in
differentiating between a neck fracture and a subtrochanteric fracture.
Abbreviations:Trochanteric fracture of the femur; Fracture line; 3Dct
Introduction
Trochanteric fractures of the femur show a complicated fracture line and determining the type of fracture by plain X-ray is difficult. In recent years, understanding fracture configuration has become easier with the popularization of 3DCT, and observation of the correlation between the location of the fracture line and insertion of capsular ligaments has become possible [1]. Trochanteric fractures were mainly categorized into Type I and Type II in 1949 by Evans [2]. This classification is based on the degree of damage to the medial cortical bone of the femur, and the difficulty level in maintaining reduction, and by dividing cases into a stable type where reduction is easier, and an unstable type where maintaining reduction is difficult. In 2006, Nakano proposed classification by 3DCT and pointed out that both the anterior and posterior fracture lines of a standard fracture line basically occur in the same place in many trochanteric fractures and designated this as the primary fracture line [3]. Furthermore, a secondary fracture line occurs near the intertrochanteric crest region and is sub-classified according to the combination of occurring bone fragments. The purpose of this study is to report the detailed consideration of the fracture line for typical trochanteric fractures of femur except for reverse oblique fractures which are classified as Type I by the Evans Classification, using 3DCT.
Materials and Method
80 joints in 80 cases (10 men, 70 women) of trochanteric fracture of the femur, Evans Classification Type I according to 3DCT imaging on one side, and a normal healthy femur on the other side were targeted. Average age was 82.3 years (range 77-103 years). The primary fracture line was considered by dividing it into an anterior section and a posterior section. Definitions of the name of bone protrusions and depressions used as indicators to describe the course of fracture line are needed. Well-known anatomical names of parts of the proximal femur include the intertrochanteric line, trochanteric fossa, and intertrochanteric crest. The iliofemoral ligament is attached on the intertrochanteric line and is divided into the lateral band and the medial band and is called the Y ligament [4-7]. Matching bony protrusions exist on the insertion of lateral band and insertion of the medial band and are named the lateral intertrochanteric eminence and medial intertrochanteric eminence, respectively (Figure1a,b). The trochanteric fossa is the region of insertion of the conjoined tendon and obturator externus. A depression in the boundary of the neck and intertrochanteric crest exists distal from the trochanteric fossa [8,9]. This trough-like depression area does not have an appropriate name and is called the intertrochanteric groove.
Figure 1A:View from the front Black arrowhead: lateral intertrochanteric eminence, black arrow: medial intertrochanteric eminence.
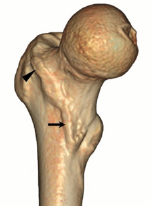
Figure 1B:View from the back white arrowhead: trochanteric fossa, white arrow: intertrochanteric groove.

Since the femoral head fragment of a trochanteric fracture of the femur is often tilted backward, observation of the posterior section of the primary fracture line by normal 3DCT is insufficient. Consequently, a 3DCT image was prepared where the femoral head section that blocks observation of the fracture line was removed and the fracture could be observed from various angles. Furthermore, the obturator internus and obturator externus were computed on the horizontal margin on the healthy side, depressions of each muscle insertion were identified, and the image was horizontally flipped to compare with the affected side. Correlation between the fracture line of the trochanteric fossa on the affected side and insertion of the obturator internus/externus was considered [10,11].In addition to the primary fracture line, a secondary fracture line runs outside the greater trochanter near the lateral intertrochanteric eminence, and travels from the upper front of the greater trochanter toward the lesser trochanter. In this study, the running of the secondary fracture line and connection of the primary and secondary fracture lines near the lateral intertrochanteric eminence were considered.
Results
The anterior section of the primary fracture line runs downward along the intertrochanteric line from the lateral intertrochanteric eminence to lesser trochanter. In many cases, the fracture reaches the lower section of lesser trochanter, then reverses and slightly rises to connect with the posterior lower fracture line (Figure 2a,b). In 27 cases 34% the frontal fracture line ran lateral rather than through the lateral intertrochanteric eminence, 39 cases 48% went through the medial, 12 cases 15% through the lateral intertrochanteric eminence, and 2 cases 3% ran through both the lateral and medial.
Figure 2A:Anterior section of the primary fracture line. The fracture line runs through the lateral intertrochanteric eminence in the downward direction and along the intertrochanteric line. In many cases, it reaches the lower section of the lesser trochanter, then reverses and slightly rises to connect with the posterior lower fracture line.
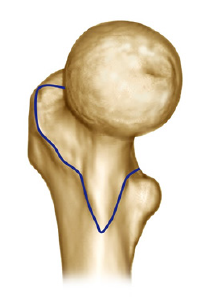
Figure 2B:Posterior section of the primary fracture line. The fracture runs from trochanteric fossa to the upper part of lesser trochanter through the intertrochanteric groove to connect with the anterior fracture line.
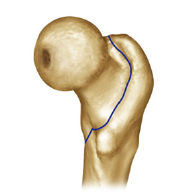
In all cases, the posterior section of the primary fracture line occurred consistently at the insertion of ischiofemoral ligament, close to the insertion of conjoined tendon and obturator externus of trochanteric fossa (Figure 3). That fracture line continued running along the intertrochanteric groove, then through upper lesser trochanter and connecting to the frontal fracture line. Morphology of avulsion fractures varied, with 68 cases 85% accompanied with avulsion fracture of the conjoined tendon or obturator externus tendon. The secondary fracture line occurs midway through the primary fracture line. The fracture runs from upper edge of the lateral intertrochanteric eminence outwardly, traveling from upper front of the greater trochanter towards the lesser trochanter, causing a greater trochanter fracture or lesser trochanter bone fragment. It is subclassified as either a greater trochanter fracture or lesser trochanter fracture, according to site of occurrence.
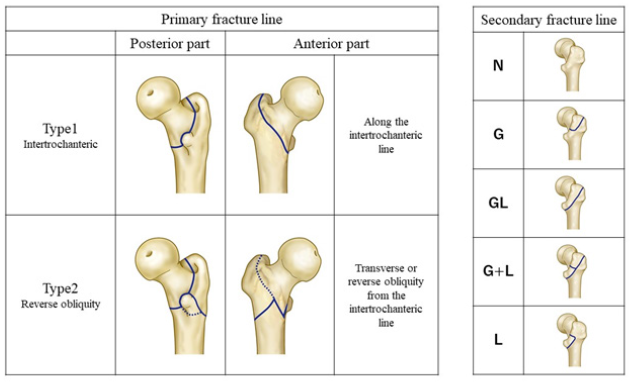
Figure 3:The fracture line occurs at the insertion of ischiofemoral ligament adjacent to the conjoined tendon and obturator extermus tendon, in all cases.
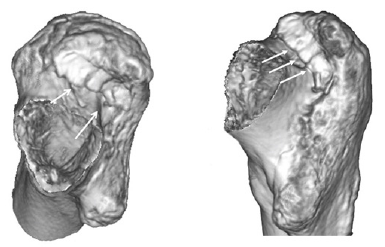
In 72 cases, a secondary fracture line was observed. Among these, 65 cases 90% showed a fracture running along the upper border of lateral intertrochanteric eminence and were most frequent, and 7 cases 10% showed a crushed lateral intertrochanteric eminence (Figure 4). There were 8 cases without a secondary fracture line (N type), 26 cases with only a greater trochanter fragment (G type), 1 case with lesser trochanter fragment (L type), 14 cases with a combined greater trochanter fragment and a lesser trochanter fragment (GL type), and 31 cases with greater trochanter fragment and lesser trochanter fragment (G+L type) (Figure 5). The anterior section of the primary fracture line, Type 1 runs along the intertrochanteric line. Type 2 as reverse obliquity runs from one location of the intertrochanteric line, on the lateral diaphyseal region in the transverse or reverse oblique direction, and then joins the posterior section of the primary fracture line by running in the front and back symmetrical direction. Furthermore, It is sub-classified according to a greater trochanter and/or a lesser trochanter fragment caused by the secondary fracture line. The connection of the primary fracture line and the secondary fracture line exists in the proximal end of the lateral intertrochanteric eminence. This area is the boundary line between the lateral intertrochanteric eminence and piriformis fossa inserted by the piriformis and is the transition area of iliofemoral ligament and ischiofemoral ligament in the anteroposterior direction.
Figure 4:Image of a typical trochanteric fracture. Black arrow: The primary fracture line and secondary fracture line join in the area corresponding to the transition between the iliofemoral ligament and the ischiofemoral ligament.
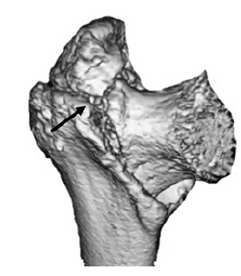
Figure 5:Classification of trochanteric fracture of the femur by 3DCT
Discussion
Classifications of trochanteric fractures of the femur are varied [2,12,13]. Evans classification (1949) has long been the most frequently used and is based on the degree of damage to the medial cortical bone of the femur as observed by a simple X-ray, and the difficulty level in maintaining reduction [2]. Trochanteric fractures were mainly categorized into Type I and Type II. Type I is fracture where the main fracture line runs from near the lesser trochanter towards the greater trochanter, and Type II is fracture where the main fracture line runs in the reverse obliquity from near the lesser trochanter in the distal outer direction [14-17]. However, this classification is determined by two-dimensional evaluation according to simple X-ray image. Due to analysis in 3DCT diagnosis, application of a fracture line observed by a simple X-ray has become insufficient. Nakano reported that both the anterior and posterior fracture lines of the primary fracture lines basically occur in the same place in many trochanteric fractures, and the anterior matched the intertrochanteric line, which is the insertion of the iliofemoral ligament. Shoda [18] classified the femoral trochanteric fractures as two, three or four parts fractures using combinations of the head, greater trochanter, lesser trochanter, and shaft using three dimensional CT [18]. However, they did not consider the site of travel of the principal fracture line and secondary fracture line.
Due to improvement in image analysis of 3DCT and related devices, accurate evaluation of the positional relationship of the insertion of capsular ligaments and the fracture line has become possible, which is impossible by simple X-ray images alone. In particular, the posterior section of the primary fracture line was easily hidden by bone fragments and could not be clearly described accurately. However, in this study, by removing the femoral head part which blocks the line of view, the fracture line from the trochanteric fossa to the intertrochanteric groove can be observed in detail. As a result, all fracture lines in the trochanteric fossa were found to occur identically at the insertion of the ischiofemoral ligament, which is close to the femoral head side of the conjoined tendon or obturator externus tendon. All cases showed a fracture line at the insertion of ischiofemoral ligament (Figure 6a,b).
Figure 6A:Axial representation of osseous and capsular anatomy at the trochanteric fossa. *ishiofemoral ligament, **conjoined tendon.
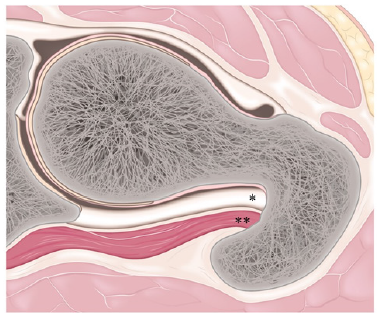
Figure 6B:Insertion of ishiofemoral ligament.
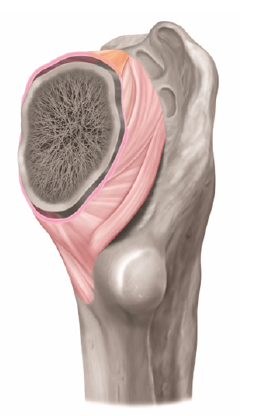
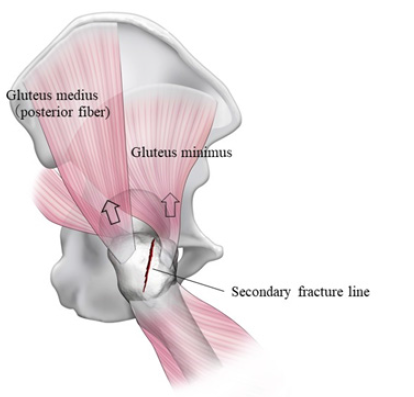
They matched the pattern of running downward from the site along the intertrochanteric groove, then through the upper edge of the lesser trochanter and connecting with the fracture line from the anterior side. The anterior fracture line also runs downward from lateral intertrochanteric eminence, along intertrochanteric line, in other words, the insertion of iliofemoral ligament and connected to the primary fracture line from the posterior side. The hip joint that connects the lower limbs to the torso, is attached by a strong capsular ligament. The anterior side is called the iliofemoral ligament and occurs from the anterior inferior iliac spine and the upper margin of the acetabulum. This is a strong triangular ligament which spreads like a fan and ends at the intertrochanteric line. [4-7]. The thick iliofemoral ligament is attached on the intertrochanteric line at a width of approximately 1.5cm. The center part is relatively thin and weak while the two borders are reinforced by two strong fiber bundles [19]. In particular, the inferior runs wide and long in the downward direction in spike form to the anterior of the lesser trochanter, then ends. In some trochanteric fractures, the proximal bone fragment is a spike-like fracture and is largely displaced towards the front. This is caused by the attachment of this ligament. On the other hand, on the posterior side, the ischiofemoral ligament occurs from posteroinferior region of the acetabulum and stops to the femoral side. [10,11,19, 20]. Actually, this insertion of ischiofemoral ligament located on the femoral head side of the insertion of the conjoined tendon or obturator externus tendon and is proximally adjacent to the trochanteric fossa. Fibers of the ischiofemoral ligament cross the posterior aspect of the femoral neck and join directly with the zona orbicularis, which is free end, then connect to the anterior capsule at the upper lesser trochanter [4]. In other words, the primary fracture of trochanteric fracture occurs along the capsular ligaments for both the anterior and posterior, and in the site where the capsule is partially freeend, it runs along the intertrochanteric groove which has less bone strength and joins to form a complete circuit. The primary fracture line and the secondary fracture line join in the proximal end of the lateral intertrochanteric eminence. The site is corresponding to the transition area of iliofemoral ligament and the ischiofemoral ligament. A difference in development course of the primary fracture line and secondary fracture line is hypothesized. First, compressive stress is applied to the depressed area of the posterior side, and the fracture occurs along the insertion of iliofemoral ligament at a symmetrical position. The posterior fiber of the gluteus medius is attached to tip of the greater trochanter. The gluteus minimus is attached to the anterior aspect of the greater trochanter [21-25] (Figure 7). The secondary fracture line develops as these muscles pull, and various types of greater trochanter fragment or lesser trochanter fragment occur.
Figure 7:The secondary fracture line on a greater trochanter.
In cases where only a greater trochanter fragment occurs, secondary fracture line merges with the posterior primary fracture line and joins at the upper lesser trochanter. In cases with a lesser trochanter fragment, it passes through the lower end of lesser trochanter and connects to the anterior fracture line (Figure 8). Depending on the direction and size of displacement, an anterior wall fracture may occur, or the lesser trochanter is broken into finely comminuted pieces. The medial femoral circumflex artery supplies most of the blood flow of the femoral head, and its terminal branches pierce the superolateral capsule and run deep into the synovial reflection before centering the femoral head just distal to the articular junction [15].
Figure 8:Connection between the primary fracture line and the secondary fracture line in the trochanteric fracture of the femur. Blue line: The primary fracture line, Red line: The secondary fracture line.
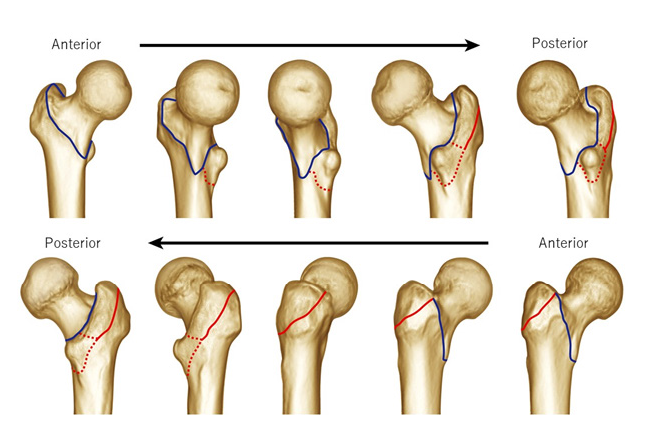
Figure 9A:Blood flow of the femoral head. Blood supply from the medial circumflex artery is preserved in trochanteric fractures.
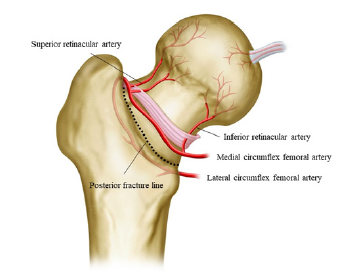
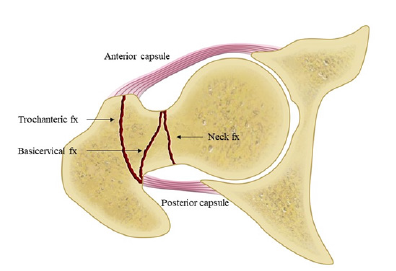
An anatomical characteristic of trochanteric fractures is that blood circulation of the femoral head is preserved since the posterior fracture line breaks at the insertion of ischiofemoral ligament located distally in the synovial retinaculum. In contrast, since neck fractures occur proximal to the synovial retinaculum, the nutrient carrying vessels to the femoral head are blocked, and avascular necrosis of the femoral head easily occurs. Difference in the disturbance due to blood blockage to the femoral head in neck fractures and trochanteric fractures is determined by the location of the fracture line of the posterior femoral neck. In other words, if the primary fracture line in the posterior section occurs from the insertion of the ischiofemoral ligament to the intertrochanteric groove, it can be defined as a trochanteric fracture, and is clearly classified as a neck fracture or subtrochanteric fracture. In this way, classifying trochanteric fractures according to the position of the fracture line is also very important to determine the difference of not only neck fractures and subtrochanteric fractures, but also Basi cervical fractures (Figure 9a,b). In cases of an unstable pattern (for example: fractures with posteromedial comminution, reverse oblique, intertrochanteric fractures with subtrochanteric extension, or lateral wall blow out), 3DCT can be an effective aid in evaluating the fracture type and in the selection of a fixation device [26]. By this study, understanding the pattern of a typical intertrochanteric fracture line could be clarified, which is a helpful in understanding fracture lines observed by simple X-ray.
Figure 9B:The fracture line in the neck fracture, the basicervical fracture and the trochanteric fracture.
Conclusion
“A trochanteric fracture of the femur consists of a primary fracture line and secondary fracture line. The primary fracture line occurs from the insertion of ischiofemoral ligament to the intertrochanteric groove in the posterior section, and in the anterior section, it occurs following along the intertrochanteric line which is the insertion of the iliofemoral ligament. In other words, this is a fracture where the primary fracture line occurs along the insertion of capsular ligaments.” The secondary fracture line occurs midway through the primary fracture line, runs from upper front of the greater trochanter towards the lesser trochanter, causing a greater trochanter fracture or lesser trochanter bone fragment. They are sub-classified according to whether a greater trochanter fracture or lesser trochanter fracture occurs.
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study. Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Han SK, Lee BY, Kim YS, Choi NY (2010) Usefulness of multi-detector CT in Boyd-Griffin type2 intertrochanteric fractures with clinical correlation. Skeletal Radiol 39(6): 543-549.
- Evans EM (1949) The treatment of trochanteric fractures of the femur. JBJS [Br] 31(2): 190-203.
- Nakano T (2006) Understanding of trochanteric fracture of the femur and classification assessed by three-dimensional computed tomography. MB Orthop 19: 39-45.
- Hewitt JD, Glisson RR, Guilak F, Vail TP (2002) The mechanical properties of the human hip capsule ligaments. J Arthroplasty 17(1): 82-89.
- Ito H, Song Y, Lindsey DP, Safran MR, Giori NJ (2009) The proximal hip joint capsule and the zona orbicularis contribute to hip joint stability in distraction. J Orthop Res 27(8): 989-995.
- Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, et al. (2008) The function of the hip capsular ligaments: A quantitative report. Arthroscopy 24(2): 188-195.
- Wagnar FV, Negrao JR, Campos J, Ward SR, Haghighi P, et al. (2012) Capsular ligaments of the hip: Anatomic, histologic, and positional study in cadaveric specimens with MR arthroplasty. Radiology 263(1): 189-198
- Hidaka E, Aoki M, Izumi T, Suzuki D, Fujiwara M (2014) Ligament strain on the iliofemoral, pubofemoral, and ischiofemoral ligaments in cadaver specimens: Biomechanical measurement and anatomical observation. Clin Anat 27(7): 1068-1075.
- Walters BL, Cooper JH, Rodriguez JA (2014) New findings in hip capsular anatomy: Dimensions of capsular thickness and pericapsular contributions. Arthroscopy 30(10): 1235-1245.
- Ito Y, Matsushita I, Watanabe H, Kimura T (2012) Anatomic mapping of short external rotators shows the limit of their preservation during total hip arthroplasty. Clin Orthop Relat Res 470(6):1690-1695.
- Tamaki T, Nimura A, Oinuma K, Shiratsuchi H, Iida S, et al. (2014) An anatomic study of the impressions on the greater trochanter: Bony geometry indicates the alignment of the short external rotator muscles. J Arthroplasty 29(12): 2473-2477.
- Jensen JS (1980) Classification of trochanteric fractures. Acta Orthop Scand 51(5); 803-810.
- Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, et al. (2007) Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 21(Suppl 10): S1-133.
- Brammar TJ, Kendrew J, Khan RJK, Parker MJ (2005) Reverse obliquity and transverse fractures of the trochanteric region of the femur; a review of 101 cases. Injury 36(7): 851-857.
- Koval KJ, Zuckerman JD (2001) Intertrochanteric fractures. In: Bucholz RW, Heckman JD (Eds.), Rockwood and Green’s fractures in adults. (5th edn). Philadelphia, Lippincott Williams & Wilkins, USA, pp. 1635-1663.
- Kregor PJ, Obremskey WT, KrederHJ, Swiontkowski MF (2005) Unstable per-trochanteric femoral fractures. J Orthop Trauma 19(1):63-6.
- Wright LT (1947) Oblique sub-cervical (reverse intertrochanteric) fractures of the femur. J Bone J Surg 29: 707-710.
- Shoda E, Kitada S, Hirase H, Sasaki Y, Niikura T, et al. (2017) Proposal of new classification of femoral trochanteric fracture by three-dimensional computed tomography and relationship to usual plain X-ray classification. J Orthop Surg 25(1).
- Kapandji IA (1987) The hip. In: The physiology of the joints annotated diagrams of the mechanics of the human joints-lower limb. (5th edn), 2, pp. 24-33.
- Solomon LB, Lee YC, Callary SA, Beck M, Howie DW (2010) Anatomy of piriformis, obturator interrnus and obturator externus. J Bone Joint Surg [Br] 92(9): 1317-1324.
- Beck M, Sledge JB, Gautier E, Dora CF, Ganz R (2000) The anatomy and function of the gluteus minimus muscle. J Bone J Surg [Br] 82(3): 358-363.
- Flack NAMS, Nicholson HD, Woodley SJ (2014) The anatomy of the abductor muscles. Clin Anat 27(2): 214-253.
- Gardner MJ, Robertson WJ, Boraiah S, Barker JU, Lorich DG (2008) Anatomy of the greater trochanteric ‘bald spot’ A potential portal for abductor sparing femoral nailing? Clin Orthop Relat Res 466(9): 2196-2200.
- Gottschalk F, Kourosh S, Leveau B (1989) The functional anatomy of tensor fascia latae and gluteus medius and minimus. J. Anat 166: 179-189.
- Robertson WJ, Gardnar MJ, Barker JU, Boraiah S, Lorich DGet al. (2008) Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy 24(2): 130-136.
- Tawari AA, Kempegowda H, Suk M, Horwitz DS (2015) What makes an intertrochanteric fracture unstable in 2015? Does the lateral wall play a role in the decision matrix? J Orthop Trauma 29 (Suppl 4): S4-S9.
© 2022 Takashi Hisatome. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






