- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
Paraspinal and Pelvic Psoas Abscess Spreading from Septic Facet Joint after Trochanteric Bursa Steroid Injection
Cameron Crasto*, Dominic Ruwe, Richy Charls and Hossein Elgafy
Department of Orthopaedic Surgery, University of Toledo Medical Center, USA
*Corresponding author: Cameron Crasto, Department of Orthopaedic Surgery, University of Toledo Medical Center, USA
Submission: August 04, 2022;Published: August 19, 2022

ISSN 2578-0069Volume2 Issue5
Abstract
Case: A 52-year-old diabetic woman presented with progressive low back pain and left lower extremity
weakness, which started two weeks after receiving a steroid injection into the greater trochanteric bursa.
Magnetic resonance image (MRI) lumbar spine demonstrated left L4-L5 facet joint involvement. Her hospital
course was significant for a large left iliopsoas abscess, left knee prosthetic joint infection, a small
epidural abscess and sepsis. Patient underwent multiple debridement of the paraspinal and pelvic iliopsoas
abscess with wound vacuum exchanges and a staged revision knee arthroplasty. At the last follow up
6 months after initial presentation, the low back pain and left hip flexor weakness improved, the lumbar
spine and pelvic wounds healed and was awaiting second stage left knee revision.
Conclusion: To the authors best knowledge, this is the first report in the literature of a psoas abscess
spreading from a septic facet joint following local greater trochanteric bursa glucocorticoid injection and
without an inciting spine corticosteroid injection.
Abbreviations: MRI: Magnetic resonance image; CT: Computed Tomography; ID: Infectious Disease; MSSA: Methicillin-Susceptible Staphylococcus Aureus; VRE: Vancomycin Resistant Enterococcus; TP: Transverse Process; VRE : Vancomycin Resistant Enterococcus
Introduction
Lower back pain is one of the most common presenting complaints from middle aged and elderly adults to their general practitioners’ office [1]. There are a variety of different causes of low back pain including Musculo skeletal degenerative changes, vascular, neurologic, malignant and infectious. When dealing with an infectious etiology, prompt diagnosis and imaging should be obtained so that culture specific antibiotic treatment can be initiated [2]. Clinically, infectious etiology of back pain should be suspected in a patient with a fever, localized spinal tenderness and neurological deficits [3]. If an infectious cause of back pain is not treated appropriately, it can spread to surrounding structures. One of the most common origins of secondary psoas abscess is from pyogenic spondylitis [4]. The majority of spine infection originates at the vertebra endplate and spreads to the adjacent disc, epidural space, and psoas muscle. The authors present a case of psoas abscess that originated from the facet joint instead of the vertebral body and disc space. To the best of our knowledge, a psoas abscess occurring after contiguous spread from the facet joint without an inciting epidural steroid injection has not been reported elsewhere in the literature.
Case Presentation
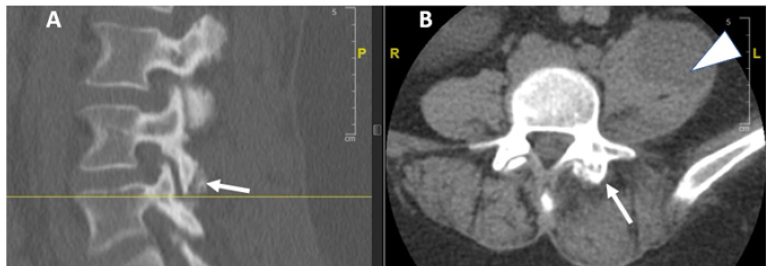
A 52-year-old female presented first to the orthopedic clinic for the atraumatic onset of left hip pain. Physical exam elicited localized tenderness over the greater trochanteric bursa with pertinent medical history including type II Diabetes mellitus, hyperlipidemia, and hypertension. Surgical history included bilateral knee arthroscopy and a primary left total knee arthroplasty. MRI of the hip revealed possible tendinopathy of the gluteus minimus and medius. Patient was diagnosed with greater trochanteric bursitis and received a local glucocorticoid injection. Two weeks following the injection, the patient reported a sudden onset of low back pain after bending over and denie any previous low back pain or recent trauma. Patient was seen by the primary care physician, diagnosed with slipped disc and prescribed short course of oral prednisone. The patient presented to the authors’ Emergency Department with worsening low back pain, progressive weakness in the left lower extremity, numbness over anterior left thigh and several episodes of stress urinary incontinence. The spine service was consulted to consider spinal cord pathology as a cause for her current symptoms. On physical examination, patient was afebrile, normotensive, had a normal heart rate and no increased work of breathing with regular respirations. Patient demonstrated left hip flexor weakness (2/5), intact motor function on the right side and normal sensation bilaterally. Lab values at this time demonstrated, hyperglycemia, leukocytosis, malnutrition with low transferrin 129 (168-348), albumin 2.3(3.5-5.7), elevated ESR (115) and CRP (373). A Computed Tomography (CT) scan of the lumbar spine demonstrated a large abscess in the left iliopsoas and significant bony destruction of the left L4-L5 facet joint (Figure1).
Figure 1:CT scan lumbar spine left parasagittal (A) and axial (B) views showed left L4-5 facet joint enlargement, some erosion (arrows) and left psoas muscle abscess (arrowhead).
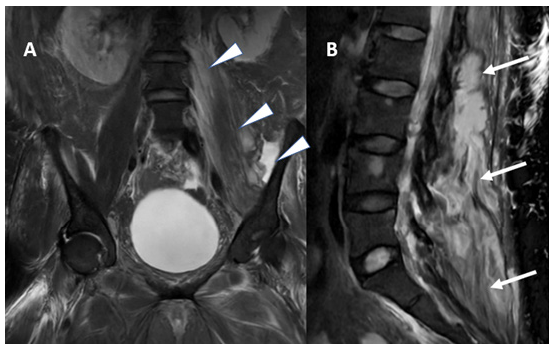
MRI of the lumbar spine revealed a left L4-5 facet joint fluid collection, left paraspinal psoas abscess extending down to the pelvis and subcutaneous abscess extending from L2 to sacrum (Figures 2-4). Patient was admitted to the hospital for treatment of her psoas abscess and was initially started on Cefepime, Vancomycin and Flagyl per Infectious Disease (ID) recommendation for systemic sepsis that required antibiotic therapy prior to obtaining cultures.
Figure 2:MRI lumbar spine T2 weighted images left parasagittal (A) and axial (B) views showed left L4-5 facet joint fluid collection (arrows) and left psoas muscle abscess (arrowhead).
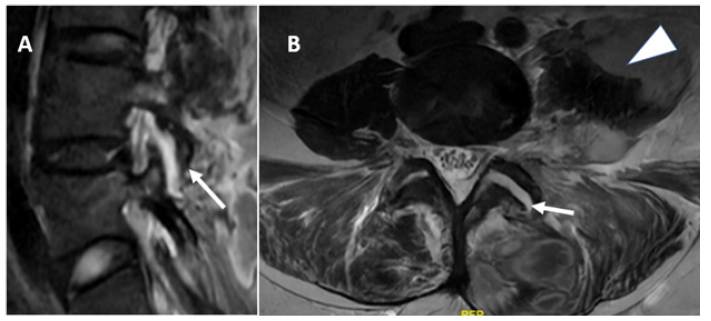
Figure 3:MRI pelvis T2 weighted images axial view showed left psoas abscess in the pelvis (arrowhead).
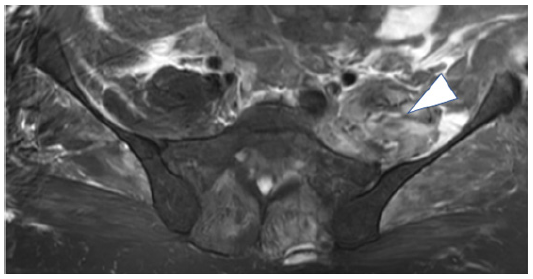
Figure 4:MRI lumbar spine T2 weighted images coronal (A) and left parasagittal (B) views showed left psoas muscle abscess extending cephalad to the pelvis (arrowhead) and subcutaneous abscess extending from L2 to sacrum (arrow).
A CT-guided aspiration and biopsy of the left iliopsoas was performed and revealed Methicillin-Susceptible Staphylococcus Aureus (MSSA). This was in line with positive blood cultures that were also consistent with MSSA bacteremia. Patient’s antibiotics were switched to Nafcillin and Flagyl per ID recommendation and then narrowed to Nafcillin. Later, during the course of treatment, multiple wound cultures were taken at time of debridement and antibiotic management was adjusted by ID team such as adding Daptomycin to cover for Vancomycin Resistant Enterococcus (VRE), fluconazole to cover for Candida albicans, and Ceftriaxone for added gram negative coverage. In addition to culture specific intravenous antibiotics, patient received oral nutrition supplements. The patient required multiple irrigation and debridement procedures through two separate incisions. The first was posterior lumbar where debridement of the left L4-5 facet joint and drainage of the left psoas abscess by excision the left Transverse Process (TP) of L4 and L5 and incising the transverse membrane between the two TP. The epidural abscess was small and did not require surgical drainage.
Ilioinguinal approach was then performed of the left pelvis where an incision was made directly over the iliac crest down to the level of the abdominal fascia. The fascia was incised and subperiosteal dissection was carried out down to iliacus muscle. Blunt dissection was done to retract the peritoneal cavity medially off the iliacus muscle and immediately upon palpation of the muscle frank pus was noted to extrude from the iliacus muscle that was drained. Wound vacuum was applied to each wound and both subsequently healed by secondary intention. Patient was also having left knee pain with concern for possible prosthetic joint infection of total knee arthroplasty given her current infectious state. A left knee arthrocentesis was performed, and culture was positive for Staph Aureus and underwent a staged revision knee arthroplasty. At the last follow up 6 months after initial presentation, the low back pain and left hip flexor weakness improved, the lumbar spine and pelvic wounds healed and was awaiting second stage left knee revision.
Discussion
Facet joints are synovial joints that connect the posterior arch between adjacent levels of the vertebral spine. Lumbar facet joint arthropathy is a common cause of lower back pain that is responsible for around 45% of those reported [5]. Facet joint pain can arise from causes such as degenerative, inflammatory arthritis, segmental instability, and infection [6]. Treatment of lumbar facet joint pain includes local steroid injections and radiofrequency denervation of the medial branches innervating the joints [7]. The most common route of spinal infection is through a hematogenous spread followed by direct inoculation with spine injections such as epidural steroid injection and lumbar facet block [8]. The majority of spine infection originates at the vertebra endplate and spreads to the adjacent disc, epidural space and psoas muscle [9]. In the case reported, the patient developed spine infection in left L4-5 facet joint rather than the more common vertebra endplate site. Further, the infection was hematogenous spread following trochanteric bursa steroid injection rather than spine injection.
The most common causative organism in spinal infection is Staphylococcus aureus [10]. Other organisms that commonly contribute to spinal infections are Enterococcus, Pneumococcus, Salmonella, E. coli and Klebsiella [10]. Granulomatous infections of the spine often originate from Mycobacterium tuberculosis, Brucellosis, fungi, and parasites [10]. In the case reported, the causative organism was Methicillin-Susceptible Staphylococcus Aureus (MSSA) confirmed with blood and wound cultures. Later, during the course of treatment, multiple wound swabs were taken at time of debridement and cultures were positive for Vancomycin Resistant Enterococcus (VRE) and Candida albicans. Psoas abscess drainage can be achieved by either percutaneously CT guided or by open surgical through posterior midline or Wiltse paraspinal approach and Ilioinguinal approach if the infection spread down to the pelvis. In the case reported, initial attempted percutaneous CT guided drainage was inadequate and open surgical drainage was done through two incisions. Posterior midline incision performed for debridement of the left L4-5 facet joint and drainage of the left psoas abscess by excision L4 and L5 left transverse process and incising the transverse membrane between the two TP to get into the paraspinal psoas abscess. That was followed by ilioinguinal approach of the left pelvis to drain iliacus muscle abscess. The two incisions were indicated due to the large size of the abscesses.
Pyogenic facet joint infections with secondary spread to the psoas muscle are rare. A literature review yielded only one other instance of a psoas infection secondary to a facet joint infection. This infection arose from a bilateral facet joint injection [11]. There are several unique features in the case reported. The infection affected the facet joint rather than the more common vertebral endplate and the disc space. Also, the infection occurred by hematogenous spread after trochanteric bursa steroid injection rather than the more common cause of direct inoculation after facet joint and epidural injection. Further, the large size of the psoas abscess that failed to be percutaneously drained and extended down to the pelvis and that required two incisions; midline to drain the paraspinal and ilioinguinal to drain the pelvic abscess. This case emphasizes the need for diligence to ascertain alternative causes for disease when common sources are not the culprit and the importance of interdisciplinary communication for optimal patient treatment.
Conclusion
Secondary spread of a facet joint infection to the psoas muscle without an inciting facet joint injection has not been reported in the literature. Debridement of the muscle and the facet joint are necessary to eradicate the infection, in addition to culture specific antibiotic, optimizing nutrition and interdisciplinary team approach.
References
- Kjeldsberg M, Tschudi-Madsen H, Mdala I, Bruusgaard D, Natvig B (2021) Patients in general practice share a common pattern of symptoms that is partly independent of the diagnosis. Scandinavian Journal of Primary Health Care 39(2): 184-193.
- Gilligan CJ, Cohen SP, Fischetti VA, Hirsch JA, Czaplewski LG (2021) Chronic low back pain, bacterial infection and treatment with antibiotics. Spine Journal 21(6): 903-914.
- Tamir E, Mirovsky Y, Halperin N (1999) Epidural spinal abscess. Harefuah 136(2): 120-122.
- Sato T, Kudo D, Kushimoto S (2021) Epidemiological features and outcomes of patients with psoas abscess: A retrospective cohort study. Annals of Medicine and Surgery 62: 114-118.
- Perolat R, Kastler A, Nicot B, Pellat JM, Tahon F, et al. (2018) Facet joint syndrome: From diagnosis to interventional management. Insights into imaging 5: 773-789.
- Le DT (2021) Facet joint injection. Stat Pearls Publishing, USA, pp. 1-16.
- Cohen SP, Raja SN (2007) Pathogenesis, diagnosis, and treatment of Lumbar Zygapophysial (facet) joint pain. Anesthesiologists 106(3): 591-614.
- Babic M, Simpfendorfer CS (2017) Infections of the spine. Infectious Disease Clinics of North America 31(2): 279-297.
- David WC, Patrick WS, David M, Michael GF (2012) A systematic review of spinal fMRI research: Outlining the elements of experimental design 17(1): 102-18.
- Balériaux DL, Neugroschl C (2004) Spinal and spinal cord infection. European radiology supplements 14(3): 72-83.
- Ballestero MFM, Carneiro V, Lima JPL, Oliveira RSde (2020). Psoas abscess after lumbar facet joint injection: Case report and literature review. Cureus 12(8):9559.
© 2022 Cameron Crasto. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






