- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
An Uncommon Etiology of a Limping Child: Rectus Femoris Avulsion Injury
Sancar Bakircioğlu* and Bülent Atilla
Department of Orthopaedics and Traumatology, Turkey
*Corresponding author: Sancar Bakircioğlu, Department of Orthopaedics and Traumatology, Ankara Turkey
Submission: February 21, 2022;Published: July 07, 2022

ISSN 2578-0069Volume2 Issue5
Abstract
It is common for a child to limp for a period of time after a minor injury. However, there are a multitude of diseases as the cause of limping ranging from infectious to metabolic or developmental acute or chronical pathologies and delays in diagnosis can result in significant morbidity and mortality. Because foot, leg, knee, hip and even spine related etiologies can cause limping, it can get very difficult to make a differential diagnosis of this commonly seen condition. The avulsion injuries, in especially adolescent, athlete patient population with hip pain and limping complaint, should be always kept in mind for unexplained etiology of limping. We report a proximal rectus femoris avulsion injury in a 12-years-old boy presenting with acute right hip pain and limping for 6 weeks which is remained undiagnosed. Pain and limping were started 2 weeks after his hospitalization due to acute pneumonia.
Keywords: Limping child; Rectus femoris; Avulsion injury; Halter; Adolescent
Abbreviations:HALTAR : The Hip Antero-Superior Labral Tear with Avulsion of Rectus Femoris; MRI: Magnetic Resonance Imaging; AIIS: Anterior Iliac Ischial Spine
Introduction
The evaluation of a limping child with hip pain is a commonly seen condition for orthopedic physicians and may be challenging to diagnose underlying etiology. However, the incidence of limping of children is not well-known. Previous studies have shown that atraumatic limping complaints of children younger than 14 years old is 1.8 per 1000 in emergency admittance [1]. The underlying pathology of a limping child can vary from simple muscle strain to critical or even life-threatening conditions such as septic arthritis or neoplastic process. Moreover, previous history or cofounding diseases may further complicate the clinical situation. Although rare, proximal rectal avulsion injuries may cause limping as well. Among all quadriceps injuries, isolated proximal rectus femoris injury is less than 1%. It may occur due to uncoordinated acute and muscular eccentric muscle contraction or acute tractions when the hip extends and the knee flexes [2]. Due to its anatomical proximity, avulsion injuries of reflected head of the quadriceps femoris may occur along with labral rupture, which is previously reported as HALTAR Syndrome (The Hip Antero-superior Labral Tear with Avulsion of Rectus femoris), which occurs with a mechanism similar to SLAP lesions on shoulder joint [3]. It is mainly seen in childhood as a painful cause of limping and challenging to diagnose due to subtle radiological signs. We report such a case in a 12-year-old boy who is remained undiagnosed for six weeks and further complicated by his recent history of hospitalization due to acute pneumonia. The parents were informed that data concerning the case would be submitted for publication, and they provided consent.
Case
A 12-year-old boy presented with a 6-week history of right hip pain, refusing to walk. His pain occurred after following discharge of a 7-days hospital stay due to acute bronchitis, where he received parenteral antibiotic treatment. Despite three different consultations and various diagnostic examinations such as plain radiography, surface ultrasonography and Magnetic Resonance Imaging (MRI), which were all reported as usual, his clinical condition was persisted and remained undiagnosed. By the thought of a possible underlying neurologic disease, the pediatric neurologist performed even a whole spine and brain MRI, but the results became normal. When he came to our clinic with persistent hip pain, further investigation with a detailed history of the initial symptoms revealed that the pain was started the night after playing football with his mates. He has attempted a series of hard strikes. His initial physical examination revealed moderate obesity, antalgic gait and an otherwise healthy boy. There was no palpable lesion but severe tenderness on the anterior region of the proximal thigh at the right side. He prefers a slightly flexed hip posture while there are no evident contractures and no restrictions on gentle passive hip motions. Active flexion and passive extensions beyond neutral were generating considerable groin pain.
Due to the recent history of hospital admission with acute bronchitis, laboratory tests were done to clarify septic etiology, but the results were normal (Sedimentation: 12mm/h, CRP: 1mg/L, afebrile, WBC: 10.200mm3).
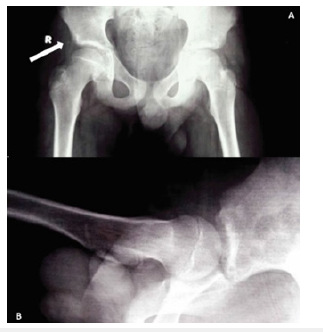
On the plain AP view of his pelvis, thickening and irregularity of the capsular attachment with a subtle periosteal reaction on the ilium were observed (Figure 1). When we evaluated the previous MRI images, there were no signs of hip joint effusion, synovitis, capsular distention, physeal or bony injury on the femoral head. There was only minimal capsular thickness on the anterosuperior aspect of the hip joint concomitant with limited edema at the adjacent acetabular ridge and Anterior Iliac Ischial Spine (AIIS) (Figure 2a). Therefore, we ordered a new follow-up MRI with gadolinium enhancement at our institution four weeks apart from the previous MRI to better demonstrate the situation of the rectus origin, the capsule, and labrum. Results became as increased T2A signal around AIIS, and even there wasn’t any aberrant labral tear concomitant to a proximal rectus femoris avulsion injury. Therefore, the patient was diagnosed with a proximal avulsion of the rectus femoris muscle. A decision was made to follow up the patient on crutches and administer 200mg Ibuprofen 2 times a day. With NSAID treatment, resting, activity modification, and proper physical therapy, a slow but steady improvement of the symptoms were observed. Active hip flexion and abduction exercises were encouraged after the 6th week. At the end of the 8th week, the patient had a significant degree of pain relief and could bear full weight on his right extremity, started his daily activity routine, and VAS score decreased from 8 to 3. At the end of week 9 of his initial visit, we performed a follow-up MRI again, and the result showed that the increased signal on the AIIS platform was disappeared (Figure 2b). On the follow-up of two years, he had no recurring episodes of pain. He was able to perform tasks related to his age and requirements of school attendance, including sports activity without restriction.
Figure 1:(A) AP pelvis view of a 12-year-old boy three days after the injury. There is subtle asymmetry due to pain-related right hip contracture. Shadow of the right hip capsule demonstrates discontinuity from the acetabular wall and has double-lucent rows (white arrow). This is due to the elevation of the periosteum over the acetabulum. (B) LAT projection revealed normal anatomy without any diagnostic sign.
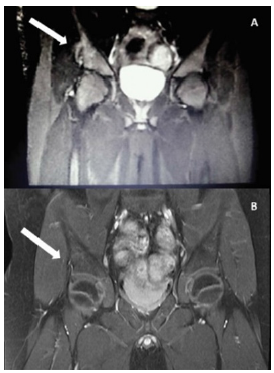
Figure 2:The patient’s initial MRI on T2 coronal view demonstrates periosteal elevation and tear at AIIS and related edema on the iliac bone (arrow) compared to the normal view on the left hip (A). The patient’s followup MRI performed after 8-week conservative treatment shows decreased edema and the minimal periosteal reaction (arrow) on the T2 fat-suppressed coronal section (B).
Discussion
Limping child is a common entity that all children have at least an episode of limping during childhood. The underlying etiology most commonly is traumatic in origin, but the diagnosis of atraumatic conditions may be more complicated [4]. In the atraumatic conditions, such as, slipped capital femoral epiphysis, Legg-Calve-Perthes Disease, transient synovitis, septic arthritis, reactive arthritis, osteomyelitis, overuse injuries, foreign body in the foot, meniscal pathologies, spine pathologies such as discitis, rheumatologic, neurologic or inflammatory processes, simple bone cysts and even underlying bone neoplasms could be the diagnosis [5-7]. Non-musculoskeletal pathologies should be thought of in suspicious conditions. The patients presenting with symptoms such as night sweating, fever, anorexia, malignancies and infective conditions should always be kept in mind [7]. There are some instances where the history of an overlying or recent disease may further complicate the presenting clinical picture, as it is in our case. Thus, the evaluation of a limping child should include a detailed history and physical examination. In our case, limping and hip pain were seen together, with a history of recent systemic infection. Differential diagnoses between acute septic and inflammatory and mechanical diseases should be performed first. When we examined the patient’s initial MRI, it almost consisted of normal intraarticular and surrounding structure findings except a subtle capsular thickening and limited edema around the superior aspect of the acetabular ridge,which gave us a clue about the rectus femoris proximal avulsion.
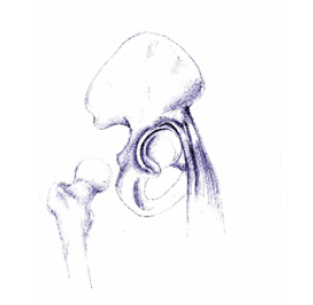
Rectus femoris avulsion injuries are relatively rare injuries and clinical presentation includes findings such as anterior localized hip pain, limping, restricted ROM, which may be confused with transient synovitis, SCFE, and septic arthritis of the hip joint. For this reason, MRI should be considered for early diagnosis in order to better assess structures such as soft tissue, articular and physical cartilage, subchondral bone, synovium, periosteum, and bone marrow in patients with persistent pain despite normal x-ray and laboratory findings [8,9]. Avulsion injuries are mostly seen in soccer players with a story of a hard kicking ball on the air, which makes detailed history crucial for managing limping. It is more common in children and adolescents than in adults and Rossi and colleagues reported that in the adolescents with 203 pelvic avulsions, 45 injuries were located on AIIS [10]. Both operative and non-operative treatments had favorable outcomes in avulsion injuries of AIIS. Generally, positive results are obtained between 3 weeks and 4 months with rest, ice, appropriate NSAID and physical therapy. The largest case series in the literature showed 11 American football players with proximal rectus femoris injuries had a favorable conservative treatment outcome [11]. Resection or reattachment of the rectus femoris muscle is an alternative surgical treatment method [12]. Previous studies described rectus femoris avulsion injury as HALTAR lesion (The Hip Antero-Superior Labral Tear with Avulsion of Rectus Femoris) [3], resembling a slap lesion in the shoulder joint (Figure 3). In our case, rectus femoris avulsion remained limited with the tendon and not extending into the labrum. We can evaluate such lesions as pre-HALTAR lesion or as the first stage of a HALTAR injury.
Figure 3:Illustration of the anatomic relationship between the reflected head of rectus femoris and labrum. The reflected head of the rectus femoris originates from a shallow groove just above the acetabulum and joint capsule, while direct head originates from AIIS. Due to its proximity to the labrum and reflected head of rectus femoris, avulsion injuries might be seen together with labral tears defined as HALTAR lesion in previous studies.
Conclusion
Our case highlights that proximal rectus femoris avulsion injuries and concomitant labral tears should be kept in mind while evaluating limping child with hip pain. The difficulty of diagnosis in such cases arises due to the absence of laboratory findings and demonstrative imaging. Additional existence of severe incapacitating pain of long duration extending up to 6 months in a significant number of cases makes this particular etiology important to be diagnosed properly in order to prevent anxiety of the patient and the family and to avoid unnecessary surgery where in majority of the cases conservative measures are helpful and it is possible to achieve complete cure without any residual consequences.
References
- Fischer S, Beattie T (1999) The limping child: Epidemiology, assessment and outcome. The Journal of Bone and Joint Surgery British 81(6): 1029-1034.
- Kary JM (2010) Diagnosis and management of quadriceps strains and contusions. Current Reviews in Musculoskeletal Medicine 3(1): 26-31.
- Hosalkar HS, Pennock AT, Zaps D, Schmitz MR, Bomar JD, et al. (2012) The Hip Antero-Superior Labral Tear with Avulsion of Rectus Femoris (HALTAR) lesion: Does the SLAP equivalent in the hip exist? Hip International 22(4): 391-396.
- Herman MJ, Martinek M (2015) The limping child. Pediatrics in Review 36(5): 184-197.
- Abbassian A (2007) The limping child: A clinical approach to diagnosis. British Journal of Hospital Medicine 68(5): 246-250.
- Mehmet E, Hasan C, Mehmet E, Kerem B (2015) Apophyseal avulsion fracture of the anterior inferior iliac spine due to a simple bone cyst. Acta Orthopaedica et Traumatologica Turcica 49(2): 213-216.
- Sawyer JR, Kapoor M (2009) The limping child: A systematic approach to diagnosis. American Family Physician 79(3): 215-224.
- Ouellette H, Thomas BJ, Nelson E, Torriani M (2006) MR imaging of rectus femoris origin injuries. Skeletal Radiology 35(9): 665-672.
- White P, Boyd J, Beattie T, Hurst M, Hendry G (2001) Magnetic resonance imaging as the primary imaging modality in children presenting with acute non-traumatic hip pain. Emergency Medicine Journal 18(1): 25-29.
- Rossi F, Dragoni S (2001) Acute avulsion fractures of the pelvis in adolescent competitive athletes: Prevalence, location and sports distribution of 203 cases collected. Skeletal Radiology 30(3): 127-131.
- Gamradt SC, Brophy RH, Barnes R, Warren RF, Byrd JT, et al. (2009) Nonoperative treatment for proximal avulsion of the rectus femoris in professional American football. The American Journal of Sports Medicine 37(7): 1370-1374.
- Houghton KM (2009) Review for the generalist: Evaluation of pediatric hip pain. Pediatric Rheumatology 7(1): 1-10.
© 2022 Sancar Bakircioğlu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






