- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
Outcomes Following Early Combined Nerve and Tendon Transfer for Foot Drop after Multi-ligamentous Knee Injury: Long Term Results of Two Patients
Andrew Maertens MD1, Jona Kerluku BS1*, Hayley Sacks MD4, Silvia Zanini MS3, Mark Drakos MD2, Scott Wolfe MD1, Sherry Backus PT DPT MA3, Duretti Fufa MD1
1Department of Hand and Upper Extremity Surgery, Hospital for Special Surgery, USA
2Department of Foot and Ankle Surgery, Hospital for Special Surgery, USA
3Motion Analysis Laboratory, Hospital for Special Surgery, USA
4NYU Langone Health Department of Orthopedic Surgery, USA
*Corresponding author: Jona Kerluku, Department of Hand and Upper Extremity Surgery, Hospital for Special Surgery, New York, USA
Submission: February 01, 2022;Published: April 14, 2022

ISSN 2578-0069Volume2 Issue4
Abstract
Introduction:Peroneal nerve injury resulting in foot drop is reported to occur in 14-40% of knee
dislocations, with severity ranging from neurapraxia to complete disruption. Operative interventions traditionally
considered for treatment include tendon transfer, nerve graft, or nerve transfer. Few reports
have presented comprehensive outcomes following combining these approaches. We report on functional
outcomes of two patients who underwent a combined nerve and tendon transfer for the treatment of
traumatic peroneal nerve palsy after multiligamentous knee injury.
Methods: Both presented with complete footdrop with sensory deficits after multiligamentous knee
injury with no signs of regeneration at <1 year by clinical and electrodiagnostic evaluation. Patients underwent
a combined nerve and tendon transfer with the same three Orthopaedic surgeons at a single
institution. Outcomes reported at least two-years from combined nerve and tendon transfer surgery include
physician reported measures, gait and strength analysis, and patient reported measures as compared
to the unaffected side.
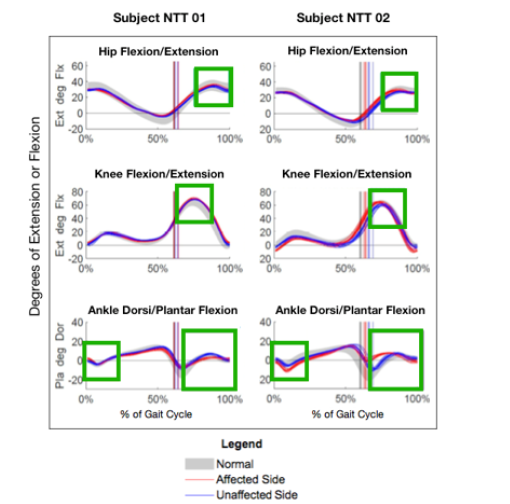
Result: Both patients were able to return to activity without functional bracing. Three-dimensional
lower extremity kinematics during self-selected level walking demonstrated controlled ankle dorsiflexion
and plantarflexion throughout a minimum of five gait cycles, in addition to symmetrical knee and hip-flexion
in these combined nerve and tendon transfer patients. On hand-held dynamometry, inversion and
eversion remain weak for both patients.
Conclusion: Long-term functional recovery can be achieved after combined nerve and tendon transfer
in patients following traumatic peroneal nerve palsy after a multiligamentous knee injury.
Keywords: Reconstructive surgery; Nerve transfer; Tendon transfer; Foot drop; Deep peroneal nerve
Abbreviations:AFO: Ankle-Foot Orthosis; PTT: Posterior Tibial Tendon; FDL: Flexor Digitorum Longus; PTT: Posterior Tibial Tendon; FDL: Flexor Digitorum Longus; ROM: Range of Motion; MARS: Marx Activity Rating Scale
Introduction
Peroneal nerve injury is reported in 14-40% of knee dislocations as a result of high impact motor vehicle accidents or sports injuries [1,2]. The peroneal nerve is prone to injury due to its superficial anatomical location, with injury severity ranging from neurapraxia to complete disruption in over 50% of presenting cases [2]. Injuries can result from several mechanisms, but are often secondary to compression or traction events, resulting in acute local ischemia to the nerve. Immediate surgical exploration and repair or reconstruction are indicated for patients with acute rupture and discontinuity of the nerve or identifiable cause of compression such as cyst or tumor. Multiple studies have shown that regeneration of axons and reinnervation of muscle fibers declines in a time-dependent fashion; therefore, early repair and exploration are indicated [3]. In cases where the nerve appears intact on initial exploration or imaging, the general consensus is close observation with electrodiagnostic studies performed at 12 weeks [4]. Tomaino et al. proposed a treatment algorithm with baseline electrodiagnostic studies performed between 4 and 6-weeks post-injury, followed by repeat studies at 12 weeks. If there is no significant improvement in nerve function, nerve exploration or reconstructive surgery should be considered.
Surgical intervention is recommended if non-surgical measures of physical therapy and Ankle-Foot Orthosis (AFO) fail to result in improved motor function at least three months after trauma [3]. Proper understanding of variability in presentation and treatment options in patients experiencing footdrop can help surgeons develop surgical plans and manage patient expectations longterm. The three operative interventions traditionally considered for the treatment of peroneal nerve injury are tendon transfer, nerve grafting, or nerve transfer [3,5]. Each has challenges with regard to achieving optimal clinical outcomes. For cases in which nerve injury is deemed too severe so that spontaneous recovery is unlikely, nerve grafting has been used and a shorter graft length is a predictor of improved functional outcomes [4,5]. In a small clinical series, when the nerve graft used was 6 centimeters or less, 44% of patients obtained useful foot dorsiflexion compared to 11% of patients using longer nerve grafts [4,5].
Aside from the somewhat poor outcomes following nerve grafting, patients treated with this strategy have a prolonged period of limited activity and AFO usage preventing a return to sports during the years while nerve recovery occurs. In failed spontaneous recovery or following failed nerve transfer, tendon transfers restore partial function while reliably eliminating the need for AFO post-operatively. Prior reports have shown up to 30 to 42% of mean ankle dorsiflexion strength after treatment with posterior tibial tendon transfer in comparison to their unaffected contralateral side [3,5]. However, impaired ankle strength and gait deviations persist in patients with a footdrop, specifically after a multiligamentous knee injury (MLKI) [3,5]. A combined approach using early tendon transfer and peroneal nerve grafting have shown slightly better outcomes than each technique alone, achieving up to 58% of dorsiflexion strength against gravity and allowing patients to return to running [6,7].
While published reports are limited, these patients still experience a prolonged period of AFO use during the time required to determine if nerve recovery is successful. Nerve transfers have shown success in upper extremity procedures but have only recently presented as a treatment strategy for lower extremity nerve injuries. Nerve transfer to footdrop patients report mixed results after tibial to peroneal nerve transfer for a more stable gait pattern, improved voluntary dorsiflexion, and increased ankle range of motion [7-9]. Again, prolonged recovery to allow for nerve recovery remains another drawback to this approach. At our institution, we have adopted a combined approach to management of footdrop following multiligamentous knee injury in young, active patients without clinical or electrodiagnostic evidence of return of function by six months from injury.
With the goal of
i. Earlier return to unbraced activity afforded by the early
tendon transfer
ii. For more meaningful strength and gait improvement
afforded by reinnervation of the anterior compartment, we combine
traditional tendon transfer with transfer of tibial nerve branches
to the anterior tibial nerve. This case series reports postoperative
functional outcomes in two such patients following early combined
nerve and tendon transfer for the treatment of traumatic peroneal
nerve palsy after multiligamentous knee injury.
Methods
Clinical series
Table 1:Demographics of nerve and tendon transfer patients.
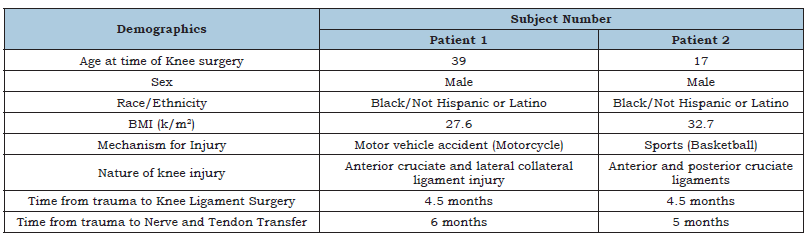
Patient demographics including mechanism of injury and time from injury to surgical intervention are included in (Table 1). In both cases, footdrop was present from time of injury, serial clinical as well as electrodiagnostic examination was consistent with complete peroneal sensory and motor palsy without evidence of return by 6 months from injury and were offered combined tendon and Nerve Transfer (NTT). Patients were contacted a minimum of two-years from NTT procedure to return for an IRB-approved follow-up physical exam, objective functional analysis and patient reported outcomes at a tertiary academic institution after obtaining informed consent.
Surgical approach
The two-part procedure is performed in the same operative setting by a board-certified Orthopaedic foot and ankle specialist (tendon transfer) and hand surgeon (nerve transfer). The Posterior Tibial Tendon (PTT) transfer is performed first through a posteromedial incision centered over the navicular. The tendinous insertion of the PTT is isolated and dissected distally off of the navicular in a subperiosteal fashion. The tendon is then tubularized using a heavy braided suture, and measured for appropriate interference screw size. The Flexor Digitorum Longus (FDL) is then identified and isolated in a lateral and plantar direction in relation to the PTT. Next, a second 3cm incision is made approximately 5cm proximal to the medial malleolus. Care is taken to identify and protect the saphenous nerve and vein, and the posterior compartment fascia is opened in a longitudinal manner.
The underlying PTT is identified adjacent to the tibia and delivered proximally through this incision. A third incision is then made on the anterior border of the fibula approximately 4cm proximal to the joint line. The syndesmosis is then exposed through this incision, which is then incised longitudinally to allow passage of the PTT graft. Finally, a fourth incision is then made in a longitudinal fashion over the border of the lateral cuneiform. The PTT is then shuttled using a nitinol wire to the opening of the incision, and the PTT graft is rigidly affixed to the lateral cuneiform using an appropriately sized Bio-Tenodesis screw (Arthrex, Naples, FL, USA). Simultaneous transfer of the FDL tendon is then performed to prevent the theoretical risk of iatrogenic flatfoot deformity with transfer of the PTT. The FDL is harvested proximally at the level of the Knot of Henry, and then affixed to the navicular bone with suture anchors or heavy braided suture.
Next, the nerve surgery involves an incision at the posterior border of the proximal tibia through which toe flexor branches of the posterior tibial nerve are identified using a nerve stimulator. A single nerve branch is harvested as close to its insertion into the muscle as possible and transfer through a window in the interosseous membrane to an anterior tibial motor branch of the peroneal nerve. Nerve coaptation is performed through a proximal incision over the lateral compartment in a tension free manner with use of the operating microscope. To ensure no tension, the ankle is taken through gentle range of motion. Post-operatively, the patient is maintained in a below-knee splint, then cast in maximal ankle dorsiflexion until 6 weeks post-operatively and then gentle therapy for range of motion and strengthening begins.
Physician and patient reported outcomes
At final follow up, physical examination included assessment for bilateral ankle Range of Motion (ROM) using a hand-held goniometer and bilateral testing of dorsiflexion, plantarflexion, inversion, and eversion strength with a hand-held dynamometer. Ankle ROM was measured with the knee in extension and knee in flexion with ankle at subtalar neutral for both knee positions. Tenderness to palpation, and sensation subjective to light touch asymmetric from contralateral side for testing of peroneal and tibial nerve distribution was also determined. Stanmore system questionnaires were completed, with excellent results between 100-85 points, and poor results of less than 55 points. Patient reported outcomes to assess knee injury recovery included Marx Activity Rating Scale (MARS) and the Lysholm Questionnaire. Patient satisfaction with surgery on a 4-point-Likert scale, 36- Item Short Form Health Survey (SF-36) to assess global health functioning, time from injury to return to unbraced activity, and pain levels were also collected.
Objective functional outcomes
Objective functional analysis included isokinetic testing, threedimensional (3D) motion capture gait analysis, and electrodiagnostic testing. Bilateral isokinetic ankle dorsiflexion torques were recorded seated with a Biodex System 4 Pro dynamometer (Biodex Medical Systems, Shirley, NY). Strength was measured for 5 trials at 60°/second (peak torque and maximum work) and endurance for 15 trials at 120°/second (measuring average power and total work). With the subject’s knee in 60° flexion, isokinetic ankle dorsiflexion strength (torque) was measured between 10° of dorsiflexion to 30° of plantarflexion. Peak values are reported in this study. 3D gait analysis of lower extremity kinematics during level walking at self-selected speed was recorded and calculated with 14 cameras (Cortex v8 and Orthotrak 6.64, Motion Analysis Corp., Santa Rosa, CA) for a minimum of 5 gait cycles. During swing, the following peak angles were recorded: ankle dorsiflexion, knee flexion, hip flexion, hip abduction, and hip external rotation. During stance, ankle dorsiflexion angle at initial contact was recorded. Electrodiagnostic testing included needle electromyography and nerve conduction study for the following seven muscles: anterior tibialis, peroneus longus, extensor hallicus longus, flexor digitorum longus, flexor hallicus longus, flexor digitorum brevis, and peroneus brevis. Recruitment pattern, percentages of motor units active, latency, conduction velocity, and amplitude were recorded. This case series has been reported in line with the process guideline.
Result
No major postoperative complications were reported in either case. Physician, patient and objective functional outcome data were collected at five years postoperatively for Patient’s 1 and 2. Neither patient reported ongoing pain at final follow up. Patient 1 reported some diminished sensation in the peroneal nerve distribution while patient 2 endorsed full sensation. Physical examination of bilateral ankle strength testing of dorsiflexion, plantarflexion, inversion, and eversion with a hand-held dynamometer are reported in (Table 2). Both patients demonstrated decreased strength compared to the unaffected limb in both the peroneal (dorsiflexion/eversion) and tibial (plantarflexion/inversion) distributions, however magnitude of strength difference was less in the peroneal nerve distribution. Biodex testing of ankle dorsiflexion strength and endurance revealed average decrease of 42.1% and 50.6%, compared to unaffected limb respectively (Table 3 & 4).
Finally, our suggestion for the surgical treatment is in type I fracture condylar blade plate in ulnar side of the bone or dorsal locking plate with three distal screws in, to avoid postoperative angulation. In type II locking low profile plates or fracture antegrade intramedullary nail seems clinically to be an effective surgical procedure. The retrograde intramedullary headless cannulated screw is also a promising technique. In type III that the oblique line of the fracture must be restored to secure the initial length of bone a lag screw is obligatory to use for this reason and final a plate to secure the osteosynthesis must be performed. An alternative surgical procedure with antegrade intramedullary nail with two or three K-wires or an antegrade locking intramedullary nail is our surgical suggestion.
In (Figure 1), analysis of gait compares affected (red) to unaffected (blue) limb as well as versus normative population gait data (gray). Both patients demonstrated ankle dorsiflexion during swing, with generally symmetrical knee and hip flexion during lower extremity gait analysis, consistent with a typical gait pattern with few compensatory movements. Additionally, during loading response, plantarflexion following ground heel strikes in NTT patients was generally completed in controlled eccentric movements of ankle dorsiflexors. The electrodiagnostic study at final follow-up showed motor unit function in tibialis anterior with no active denervation in either patient. Similarly, donor muscles (toe flexors) showed typical recruitment pattern suggesting minimal donor site morbidity. All patient-reported outcomes were generally good and are reported in (Table 5). Both patients were able to return to the highest unbraced activity by six months from the NTT procedure. Both patients reported limitations in activity due more to knee rather than ankle function.
Table 2:Physical exam assessing isokinetic strength with hand-held dynaomometer.
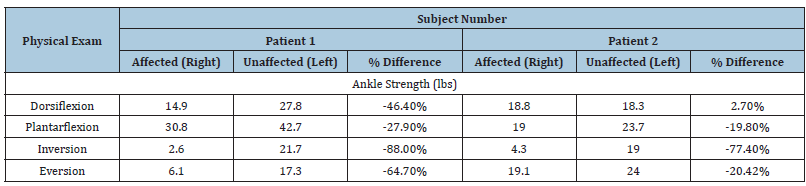
Table 3:Biodex strength testing.
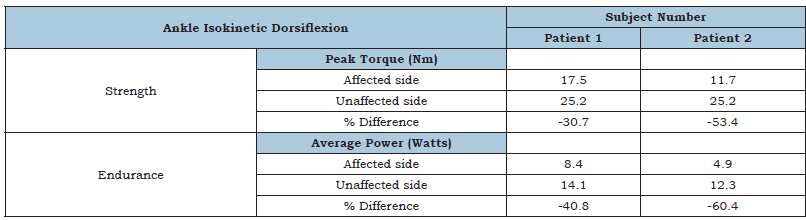
Table 4:Patient-Reported outcomes.
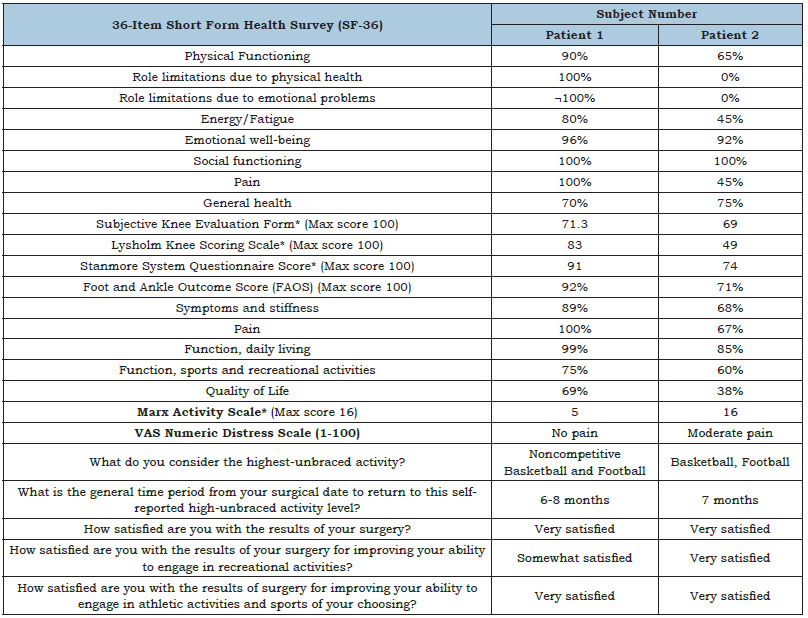
Source: *Higher score=Better level of function.
Figure 1:Gait Analysis Kinematics of Nerve and Tendon Transfer Patients.
Discussion
In this series, we report on two patients who underwent combined early tendon and nerve transfer for foot drop following multiligamentous knee injury and found no major complications, restoration of controlled ankle dorsiflexion through gait and return to maximum level of unbraced activity by 6 months from surgery. While ankle dorsiflexion strength and endurance remained substantially impaired compared to the contralateral limb (40- 50%), this approach appears safe with achievement of acceptable outcomes comparable to other approaches to management of footdrop, but with the advantage of earlier return to activity. The primary objective of reconstructive surgery following a peroneal nerve injury is restoration of muscle balance and function to allow for improved dorsiflexion with gait. The initial surgery is often nerve exploration with neurolysis. A prior study evaluating outcomes after peroneal nerve grafting showed only 28% achieving functionally acceptable results. The potential benefit of combining nerve and tendon surgery has been demonstrated. Ho et al, reported on their series of 12 patients that either underwent simultaneous peroneal nerve exploration and repair with tendon transfer surgery or repair with exploration alone. They found increased satisfaction scores (86% vs 60%) and improved dorsiflexion (100% vs 40%) in the simultaneous tendon transfer and nerve repair group, as compared to the control group of nerve exploration and repair alone15. Similarly, Ferraresi et al. reported on their series of 45 patients with traumatic common peroneal injuries that either received nerve repair alone or nerve repair with tendon transfer. They found a satisfactory reinnervation rate when nerve surgery was performed with simultaneous nerve surgery, whereas 100% (6/6) patients who elected for nerve surgery alone did not recover functional ankle dorsiflexion [10].
Due to limited reports, it is difficult to compare the present findings with prior literature on nerve transfer for foot drop [7]. reported on their series of 31 patients with common peroneal palsy treated with double nerve transfer surgery alone. They found motor recovery of M3 or M4 grade of tibialis anterior, extensor hallucis longus, and extensor digitorum longus was achieved in 38- 42% of patients [8]. In our small series targeting only the anterior tibial nerve, we achieved greater than antigravity strength in both patients. Additionally, and perhaps more importantly, isolated muscle testing and the detailed gait analysis performed of these patients suggested that NTT resulted in controlled ankle dorsiflexion through the gait cycle with few compensatory movements [11-13]./
Further, detailed patient-rated outcomes distinguish this series from prior reports and show good functional scores across multiple domains despite ongoing strength impairment. This study is limited by the limited number of patients, which is a result of the unique nature of the injury. Direct comparison of the same physical exam, strength, gait, and functional outcome testing in patients who underwent tendon transfer alone would help determine if the gait improvements are driven more by the tendon or nerve transfer and can be a topic for further investigation [14,15].
Conclusion
This study of two patients following early combined tendon and nerve transfer for footdrop showed no immediate complications or donor site morbidity with improved dorsiflexion, gait mechanics, and good patient-rated outcomes at minimum two years postoperatively [16]. This particular combined approach warrants further investigation of larger case series and comparison to other techniques for management of footdrop in the young, active patient.
Consent
Written informed consent was obtained from the patient for publication of this case series and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
References
- DY CJ, Inclan PM, Matava MJ, Mackinnon SE, Johnson JE (2021) Current concepts review: Common peroneal nerve palsy after knee dislocations. Foot Ankle Int 42(5): 658-668.
- Manske RC, Hosseinzadeh P, Giangarra CE (2008) Multiple ligament knee injury: Complications. N Am J Sports Phys Ther 3(4): 226-233.
- Fu SY, Gordon T (1995) Contributing factors to poor functional recovery after delayed nerve repair: Prolonged axotomy. J Neurosci 15(5 Pt 2): 3876-3885.
- Kim DH, Murovic JA, Tiel R, Kline DG (2004) Management and outcomes in 353 surgically treated sciatic nerve lesions. J Neurosurg 101(1): 8-17.
- Yeap JS, Birch R, Singh D (2001) Long-term results of tibialis posterior tendon transfer for drop-foot. Int Orthop 25(2): 114-118.
- Garozzo D, Ferraresi S, Buffatti P (2004) Surgical treatment of common peroneal nerve injuries: Indications and results. A series of 62 cases. J Neurosurg Sci 48(3): 105-112.
- Ho B, Khan Z, Switaj PJ (2014) Treatment of peroneal nerve injuries with simultaneous tendon transfer and nerve exploration. J Orthop Surg Res 9: 67.
- Nath RK, Lyons AB, Paizi M (2008) Successful management of foot drop by nerve transfers to the deep peroneal nerve. J Reconstr Microsurg 24(6): 419-427.
- Leclère FM, Badur N, Mathys L, Vögelin E (2015) Nerve Transfers for persistent traumatic peroneal nerve palsy: The inselspital bern experience. Neurosurgery 77(4): 572-580.
- Ferraresi S, Garozzo D, Buffatti P (2003) Common peroneal nerve injuries: Results with one-stage nerve repair and tendon transfer. Neurosurg Rev 26(3): 175-179.
- Wiesseman GJ (1981) Tendon transfers for peripheral nerve injuries of the lower extremity. Orthop Clin North Am 12(2): 459-467.
- Kadiyala RK, Ramirez A, Taylor AE, Saltzman CL, Cassell MD (2005) The blood supply of the common peroneal nerve in the popliteal fossa. J Bone Joint Surg Br 87(3): 337-342.
- Agha RA, Sohrabi C, Mathew (2020) The Process 2020 guideline: Updating consensus preferred reporting of caseseries in surgery (process) guidelines. Int J Surg 84: 231-235.
- Seidel JA, Koenig R, Antoniadis G, Richter HP, Kretschmer T (2008) Surgical treatment of traumatic peroneal nerve lesions. Neurosurgery 62(3): 664-673.
- Molund M, Engebretsen L, Hvaal K, Hellesnes J, Ellingsen E (2014) Posterior tibial tendon transfer improves function for foot drop after knee dislocation. Clin Orthop Relat Res 472(9): 2637-2643.
- Giuffre JL, Bishop AT, Spinner RJ, Levy BA, Shin AY (2012) Partial tibial nerve transfer to the tibialis anterior motor branch to treat peroneal nerve injury after knee trauma. Clin Orthop Relat Res 470(3): 779-790.
© 2022 Jona Kerluku BS. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






