- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
New Devices of Old Gold Ideas: Batbridge and DIF
Concetto Battiato1* and Massimo Berdini2
1Department of Orthopedics and Traumatology, Mazzoni Hospital, Italy
2Department of Clinical and Molecular Sciences, Università Politecnica delle Marche, Italy
*Corresponding author: Concetto Battiato, MD PhD, Department of Orthopedics and Traumatology, ASUR Marche Area Vasta 5 Ascoli Piceno, Italy
Submission: May 04, 2021;Published: June 01, 2021

ISSN 2578-0069Volume2 Issue3
Background
The femur fractures of the elderly, in particular in the two varieties subtrochanteric and of the distal femur, remain nowadays one of the most important challenges in surgical fracture treatment as they are often complicated, with an oblique or a spiral shape, intra-articular and with a comminuted nature [1-4]. With the increasing of population age and increasing number of periprosthetic fractures, complex fractures of the distal or subtrochanteric femur are expected to increase, although they represent a low percentage of all femoral fractures [5-7].
Plate osteosynthesis and retrograde nailing are almost the unique options for the treatment of femur fractures indicated below. The use of plating technologies was intended to limit the disruption of the blood supply to the bones to improve healing, but locked plating can result in overly stiff constructs and thereby suppress interfragmentary motion preventing callus formation. Construct stiffness has been cited as a factor linked to non-unions [8-11]. Malunion and implant failure are relatively common in elderly due to the wide medullary canal and osteoporosis [12-14].
For an adequate bone healing one of crucial aspect is the maintenance of mechanical stimulus on the fracture site and to grant the right conditions under which healing can progress, such as the definition of interfragmentary strain beneficial for secondary bone healing. The use of Minimally Invasive Plate Osteosynthesis (MIPO), have further enhanced the biological capability for repair by minimizing trauma to the periosteum and surrounding soft tissues. Nowadays developments in locked plating surgical approach have addressed one main aspect for successful healing: the biology; but the resulting mechanical environment can vary substantially depending on the fracture structure and on the subsequent configuration of the implant [15].
Introduction
Looking at the history of the use of orthopaedic implants, many solutions have been sought to try to solve the problems related to bone healing. Only considering the aspect regarding stiffness of orthopaedic devices, many attempts have been made to solve the problem in other body districts or for other surgical solutions such as external fixators or intramedullary nails. With these devices it is possible to grant a first static phase of osteosynthesis, followed by a dynamic phase due to the modification of the implant itself, which should allow a better bone distribution of the strain forces on fractures to ensure reduction reduction of nonunion rate stimulating the bona callus fracture.
A simple technique that has found a wide use since the advent of surgical treatment of fractures is Cerclage wiring. In literature a lot of works have reported the use of various cerclage technologies with a wide range of results and clinical applications: in fact, it may have been the first internal fixation technique. There are four methods of cerclage wiring usage: tension band, cerclage, hemi-cerclage and interfragmentary wires [16].
Cerclage wire can be applied surgically in two different ways: as a temporarily device for reduction during surgery, which is removed when synthesis is obtained, and can be used long term as an implant. When cerclage wires are used as implants, they may be used alone or in combination with another synthesis device (such as plates, nails, stems of prosthesis or a combination of thereof). The increasing numbers of periprosthetic fractures have led to a revival of interest for this simple technique so much to lead to the design of plates suitable for this specific purpose that had housings already prepared for the cerclage itself [17].
If we take a look at the solutions found in orthopedic surgery for the reduction and stabilization of complex fractures within the panorama of the plates, a particular type of plate stands out which has the possibility of performing a dual function: The Dynamic Internal Fixator (DIF). The DIF system is a plate with an angular stability which covers the principles of “internal fixator” and that can be modified to became dynamic if and when necessary, without having to remove it. In this way the most important limit of the internal fixators is overcome thanks to the possibility of allowing the compression at the fracture site by acting on the plate itself and allowing the patient to load during the healing process. Furthermore, the possibility of using a sliding plate, such as the DIF, reduce the potentially harmful angular bending forces by converting them into a sliding and axial compression movement at the fracture site [18-20].
The theory that different mechanical moments and variable mechanical stress during the healing process are necessary finds its basis in the fact that every single fracture has peculiar characteristics (such as fracture line, bone stock, number of fragments, comminution, etc.). Forces acting on the fracture site cause a biochemical reaction of the cells involved and a subsequent release of chemical mediators, growth factors, and hormones that work not only at the fracture site but also on a systemic level, as well as the alteration/deprivation of neuronal signals negatively affects the bone healing process. On the basis of this concepts there are many possible advantages in the complex process that leads to bone repair that can derive from a device of synthesis that can vary from static to dynamic [21-24]. These devices showed in literature encouraging results in terms of surgical technique, operating time, safety, and functional outcomes, though the complications rate was comparable to that of other complex reconstructions [18].
Cerclage
Femoral fractures, mostly spiral fractures or those occurring after total hip or knee replacement, often need cerclage wire fixation to optimize the reduction. These devices could be placed percutaneously, with mini-open or through widely open approaches. In literature is reported that cerclage wiring is an effective extramedullary instrument that provides circumferential force across the fracture surfaces when tension is applied allowing a good reduction and fixation when used alone in combination with other implants [25].
Subtrochanteric or distal femur fractures, in the presence of a long oblique or a complex multifragmentary rime of fracture, can be hardly cannulated with a guidewire without an open reduction. The use of cerclage wires as a first approach to reducing the fracture allows to immediately obtain the reconstitution of the normal anatomical profile, to have a reference for the reconstruction of the length and sometimes also to restore the correct rotational axis of the bone segment prior to nailing, making the intramedullary cannulation easier and faster [26-28].
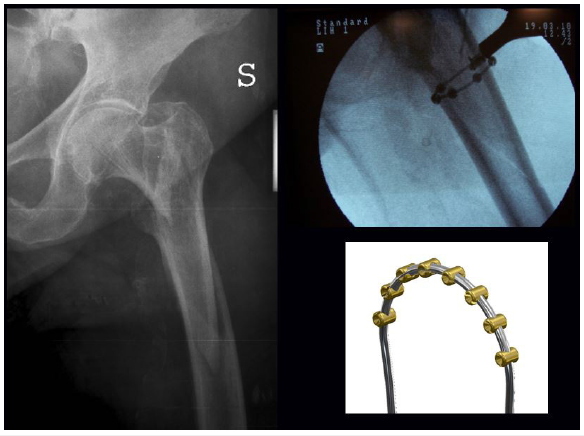
Periprosthetic femoral fracture is one potential complication of total hip arthroplasty (THA). Modern osteosynthesis techniques are facing the treatment of these fractures also developing increasingly interesting devices. Nevertheless, a combination of locking plate and cerclage is considered by some authors as the more suitable strategy of treatment, eventually with the addition of strut allografts which should allow for better healing and fewer complications [29-34] (Figure 1).
Figure 1:

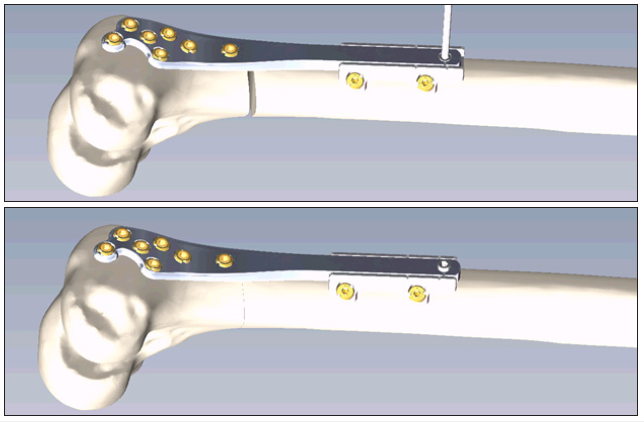
Locking plate technology offers by its nature increased angular stability and, theoretically, better fixation in osteoporotic bone, even if for the correct positioning, which must not be too rigid, the skill of the surgeon remains crucial, and the sacrifice of soft tissues is still high. On the other hand, the evolution of percutaneous cerclage wiring and MIPO techniques have allowed to reduce the complications associated with extensive exposures [8]. In a 2016 study were reported the results of a cerclage wiring elevated from the bone surface with protrusions or spheres than cables or conventional wires, a low contact version (Batbridge), and was demonstrated used in four periprosthetic fractures as an exclusive implant for reduction and fixation, whereas in 50 other cases it was combined with internal devices (hip stem of THA, intramedullary nail, DIF, antibiotic spacers). The results show non-union and delayed union which appear to be less than the complication rate seen with conventional open reduction and internal fixation. The average time to union (3 months) was comparable to other method of indirect reduction or mini-open reduction and fixation for such difficult fractures. The limitation of the cerclage is that it can be used in the most long oblique fracture, spiral fracture, and some wedge fractures, whereas it should be avoided for transverse or short oblique fractures [35] (Figure 2).
Figure 2:
The use of cerclage wiring was recommended in these cases for the advantages of minimally invasive reduction and fixation technique, low costs, soft tissue sparing especially with percutaneous approach with almost the same or better outcomes in the management for displaced subtrochanteric fractures, fractures of the distal femur and peri-prosthetic fractures [25,35]. Traditionally, the use of cerclages in fracture has been considered potentially dangerous because there was a theory that these devices led to a strangulation of periosteal vascularization which can led to bone necrosis and non-union. Some evidence in literature have shown that the blood flow of the bone cortex is constituted by centrifugal, circumferential way, and in addition large longitudinal vessels, not only in the periosteum but also in the medullary canal, which are not destroyed using the cerclage wires [16,29,35,36].
Periosteal devascularization may occurs in the surgical dissection due to stripping to expose and reduce the fracture, causing potentially bone necrosis and other complications. A possible disastrous complication is neurovascular injury, such as charge of the superficial femoral artery and sciatic nerve, because it travels from the femur midshaft to the distal third often close to the fractures site or near the surgical site of cerclages [37-39].
DIF
In literature could be find many studies that have dealt with the issue of fracture fixation by internal or external fixation in an increasingly innovative way. Many factors have significantly influence in bone healing (biology, macro and microscopic loading forces, implant-bone interface, force loading and unloading axes) and often they are not exactly predictable variables in the preoperative phase, so it makes extremely difficult to formulate an exact prognosis or predict the evolution of a certain fracture after surgical treatment [40].
This problem has been tackled over time first with static systems that guarantee a high stiffness to the construct set up for fracture treatment. Subsequently, the approach was modified (ex. intramedullary nailing) introducing technical measures that guarantee not only stability of the construct, but also the possibility of stimulating bone regeneration through the application of the forces necessary to stimulate the biology of the bone itself through the normal anatomical axis [41]. Consolidation delays, non-union and implants ruptures are often caused by the rigidity of the implants that do not allow a correct load transfer on the fractures fragments. Another described problem was the asymmetric formation of the bone callus often due to the total stiffness in the bone segments underlying the plate. The use of a longer plate that correctly cover the site of the fracture optimizes the distribution of mechanical stress, but only the possibility of changing the load vector forces on the fracture and on the plate from static to dynamic can allow the protection of the reliability of the plate and the stabilization in compression of the fracture with lesser bending and non-axial loads [18,42].
In literature is described an interesting solution with these characteristics: The Dynamic Internal Fixator. The theory underlying the development of the Dynamic Internal Fixator (DIF) plate: it is a plate with angular stability with the possibility of ongoing dynamization, as already possible, without needing to remove it. Unlocking the sliding movement, the distalization of the fulcrum modified the bending forces into translatory ones, compressing the fracture ends and shifting resistances from the plate to the bone itself [18] (Figure 3).
Figure 3:The DIF system.
Thanks to the possibility of dynamization, the DIF plate allows
the load to be transferred to the fracture site in a controlled manner
during the healing process. Moreover, the characteristics of a plate
“slide” system allows the bending movement to be converted into
a sliding movement and then into axial compression. This system
could be used for fixation of femoral fractures in the following cases:
I. Fractures of the middle/distal diaphysis
II. Supracondylar fractures
III. Distal intra-articular fractures
IV. Consolidation delays and non-union
V. Growing bone segments (pediatrics)
VI. Failure of implants.
Foreseen advantages include using of self-locking screws with a conical head that avoids the loss of reduction even in osteoporotic bones, the possibility of early functional load thanks to the correct transfer of forces on the fracture fragments, the reduction of failure rate or breakage of the implants and a potential reduction of functional healing times. Encouraging results were reported on 26 cases treated with this device. Fracture healing with complete bony consolidation and without secondary loss of reduction evaluated at 6 months from the first surgery was achieved in 96% [18] (Figures 4-6).
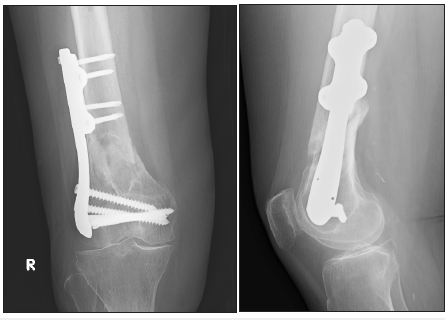
Figure 4:Fracture of the distal femur before treatment.
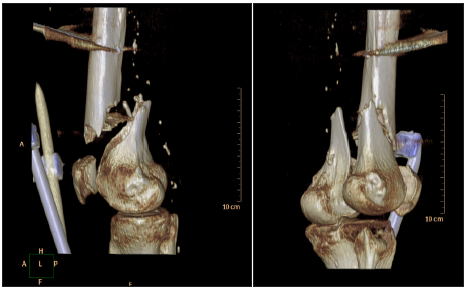
Figure 5:Fracture of the distal femur after treatment with DIF system.
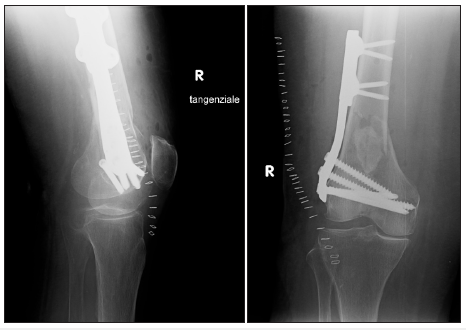
Figure 6:Fracture of the distal femur (3 months dynamization) after a year from surgical treatment.
Conclusion
These simple techniques DIF and cerclage are still used and can represent solutions that are often little used or even misunderstood, but easy to apply, for a weighted approach between surgical risks and benefits for the patient for many of the cases described in literature.
References
- Gangavalli AK, Nwachuku CO (2016) Management of distal femur fractures in adults: An overview of options. Orthop Clin North Am 47(1): 85-96.
- Keudell AV, Shoji K, Nasr M, Lucas R, Dolan R, et al. (2016) Treatment options for distal femur fractures. J Orthop Trauma 30(Suppl 2): S25-S27.
- Hake ME, Davis ME, Perdue AM, Goulet JA (2019) Modern implant options for the treatment of distal femur fractures. J Am Acad Orthop Surg 27(19): e867-875.
- Salminen S, Pihlajamäki H, Avikainen V, Kyrö A, Böstman O (1997) Specific features associated with femoral shaft fractures caused by low-energy trauma. J Trauma 43(1): 117-122.
- Court Brown CM, Caesar B (2006) Epidemiology of adult fractures: A review. Injury 37(8): 691-697.
- Court-Brown CM, Duckworth AD, Clement ND, McQueen MM (2018) Fractures in older adults. A view of the future? Injury 49(12): 2161-2166.
- Gwathmey FW, Quaidoo SMJ, Kahler D, Hurwitz S, Q Cui (2010) Distal femoral fractures: current concepts. J Am Acad Orthop Surg 18(10): 597-607.
- Bottlang M, Doornink J, Lujan TJ, Fitzpatrick DC, Marsh JL, et al. (2010) Effects of construct stiffness on healing of fractures stabilized with locking plates. J Bone Joint Surg Am 92 Suppl 2(Suppl 2): 12-22.
- Henderson CE, Lujan TJ, Kuhl LL, Bottlang M, Fitzpatrick DC, et al. (2011) 2010 mid-America Orthopaedic Association Physician in Training Award: healing complications are common after locked plating for distal femur fractures. Clin Orthop Relat Res 469(6): 1757-1765.
- Lujan TJ, Henderson CE, Madey SM, Fitzpatrick DC, Marsh JL, et al. (2010) Locked plating of distal femur fractures leads to inconsistent and asymmetric callus formation. J Orthop Trauma 24(3): 156-162.
- Wang MT, An VVG, Sivakumar BS (2019) Non-union in lateral locked plating for distal femoral fractures: A systematic review. Injury 50(11): 1790-1794.
- Perren SM (1991) The concept of biological plating using the limited contact-dynamic compression plate (LC-DCP). Scientific background, design and application. Injury 22(Suppl 1): 1-41.
- Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL (2011) Locking plates for distal femur fractures: is there a problem with fracture healing? J Orthop Trauma 25(Suppl 1): S8-S14.
- Collinge CA, Gardner MJ, Crist BD (2011) Pitfalls in the application of distal femur plates for fractures. J Orthop Trauma 25(11): 695-706.
- Stoffel K, Dieter U, Stachowiak G, Gächter A, Kuster MS (2003) Biomechanical testing of the LCP--how can stability in locked internal fixators be controlled? Injury 34(Suppl 2): B11-B19.
- Angelini A, Battiato C (2015) Past and present of the use of cerclage wires in orthopedics. Eur J Orthop Surg Traumatol 25(4): 623-635.
- Lever JP, Zdero R, Nousiainen MT, Waddell JP, Schemitsch EH (2010) The biomechanical analysis of three plating fixation systems for periprosthetic femoral fracture near the tip of a total hip arthroplasty. J Orthop Surg Res 5: 45.
- Battiato C, Angelini A, Giovannini F, Sirabella FS, Ruggieri P (2019) Effectiveness of the dynamic internal fixator system in metaphyseal and epiphyseal femoral fractures: 10 years of experience and future expectations. J Long Term Eff Med Implants 29(2): 151-158.
- Lunsjö K, Ceder L, Stigsson L, Hauggaard A (1996) Two-way compression along the shaft and the neck of the femur with the Medoff sliding plate: one-year follow-up of 108 intertrochanteric fractures. J Bone Joint Surg Br 78(3): 387-390.
- Ehlinger M, Dujardin F, Pidhorz L, Bonnevialle P, Pietu G, et al. (2014) Locked plating for internal fixation of the adult distal femur: influence of the type of construct and hardware on the clinical and radiological outcomes. Orthop Traumatol Surg Res 100(5): 549-554.
- Ueno M, Urabe K, Naruse K, Uchida K, Minehara H, et al. (2011) Influence of internal fixator stiffness on murine fracture healing: two types of fracture healing lead to two distinct cellular events and FGF-2 expressions. Exp Anim 60(1): 79-87.
- Hietaniemi K, Peltonen J, Paavolainen P (1995) An experimental model for non-union in rats. Injury 26(10): 681-686.
- Simpson AHRW, Tsang STJ (2018) Non-union after plate fixation. Injury 49(Suppl 1): S78-S82.
- Epari DR, Gurung R, Fliri LH, Schwyn R, Schuetz M, et al. (2021) Biphasic plating improves the mechanical performance of locked plating for distal femur fractures. J Biomech 115: 110192.
- Lee JH, Park KC, Lim SJ, Kwon KB, Kim JW (2020) Surgical outcomes of simple distal femur fractures in elderly patients treated with the minimally invasive plate osteosynthesis technique: can percutaneous cerclage wiring reduce the fracture healing time? Arch Orthop Trauma Surg 140(10): 1403-1412.
- Kennedy MT, Mitra A, Hierlihy TG, Harty JA, Reidy D, et al. (2011) Subtrochanteric hip fractures treated with cerclage cables and long cephalomedullary nails: a review of 17 consecutive cases over 2 years. Injury 42(11): 1317-1321.
- Zickel RE (1980) Subtrochanteric femoral fractures. The Orthopedic clinics of North America 11(3): 555-568.
- Shukla S, Johnston P, Ahmad MA, Jones HW, Patel AD, et al. (2007) Outcome of traumatic subtrochanteric femoral fractures fixed using cephalo-medullary nails. Injury 38(11): 1286-1293.
- Apivatthakakul T, Phornphutkul C, Bunmaprasert T, Sananpanich K, Oca AFD (2012) Percutaneous cerclage wiring and Minimally Invasive Plate Osteosynthesis (MIPO): A percutaneous reduction technique in the treatment of Vancouver type B1 periprosthetic femoral shaft fractures. Arch Orthop Trauma Surg 132(6): 813-822.
- Tsiridis E, Pavlou G, Venkatesh R, Bobak P, Gie G (2009) Periprosthetic femoral fractures around hip arthroplasty: current concepts in their management. Hip Int 19(2): 75-86.
- Dennis MG, Simon JA, Kummer FJ, Koval KJ, DiCesare PE (2000) Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: a biomechanical study of 5 techniques. J Arthroplasty 15(4): 523-538.
- Buttaro MA, Farfalli G, Núñez MP, Comba F, Piccaluga F (2007) Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint Surg Am 89(9): 1964-1969.
- Baum C, Leimbacher M, Kriechling P, Platz A, Cadosch D (2019) Treatment of periprosthetic femoral fractures vancouver type B2: Revision arthroplasty versus open reduction and internal fixation with locking compression Plate. Geriatr Orthop Surg Rehabil 10: 2151459319876859.
- Ricci WM, Borrelli J (2007) Operative management of periprosthetic femur fractures in the elderly using biological fracture reduction and fixation techniques. Injury 38(Suppl 3): S53-S58.
- Angelini A, Battiato C (2016) Combination of low-contact cerclage wiring and osteosynthesis in the treatment of femoral fractures. Eur J Orthop Surg Traumatol 26(4): 397-406.
- Perren SM, Oca AFD, Lenz M, Windolf M (2011) Cerclage, evolution and potential of a Cinderella technology. An overview with reference to periprosthetic fractures. Acta Chir Orthop Traumatol Cech 78(3): 190-199.
- Aleto T, Ritter MA, Berend ME (2008) Case report: superficial femoral artery injury resulting from cerclage wiring during revision THA. Clin Orthop Relat Res 466(3): 749-753.
- Devendra A, Avinash M, Chidambaram D, Dheenadhayalan J, Rajasekaran S (2018) Vascular injuries due to cerclage passer: Relevant anatomy and note of caution. J Orthop Surg (Hong Kong) 26(1): 2309499018762616.
- Kelly BA, Hambright DS, Rodriguez EK (2017) Risk of injury to neurovascular structures during open cerclage wiring of the femur: A Cadaveric Study. J Surg Orthop Adv 26(1): 1-6.
- Krappinger D, Wolf B, Dammerer D, Thaler M, Schwendinger P, et al. (2019) Risk factors for nonunion after intramedullary nailing of subtrochanteric femoral fractures. Arch Orthop Trauma Surg 139(6): 769-777.
- Fontenot PB, Diaz M, Stoops K, Barrick B, Santoni B, et al. (2019) Supplementation of Lateral Locked Plating for Distal Femur Fractures: A Biomechanical Study. J Orthop Trauma 33(12): 642-648.
- Kandemir U (2018) Distal femur: dynamization of plating. Injury 49(Suppl 1): S44-S48.
© 2021 Concetto Battiato. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






