- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
Unstable Fractures of Fifth Neck Metacarpal (Boxer Fracture): A New Classification System
Kastanis G1* and Pantouvaki A2
1Department of Orthopaedic, General Hospital of Heraklion -Venizeleio, Greece
2Department of Physiotherapy, General Hospital of Heraklion -Venizeleio, Greece
*Corresponding author: Grigorios Kastanis, Department of Orthopaedic, General Hospital of Heraklion -Venizeleio, Crete, Greece
Submission: March 22, 2021;Published: April 08, 2021

ISSN 2578-0069Volume2 Issue3
Abstract
The fifth metacarpal neck fractures or Boxer fracture is the most common injury of upper extremity fracture treated in the emergency department. It usually occurs in young population with aggressive conduct. The majority of them are stable and the conservative treatment is the gold standard while the unstable fractures need operative intervention, but an important hypothetical question is posed. Are all these fractures the same or do they differ? In literature there is not clear classification about the pattern or the type of fifth metacarpal neck fractures. The aim of this study is to present a classification system based on the type of fractures and the most appropriate method of fracture fixation, with the scope to achieve the goal of treatment which is the full range of motion and return to previous functional status.
Keywords: Metacarpal neck fractures; Boxer’s fracture; Classification system; Operative treatment
Introduction
Metacarpal fractures are common orthopaedic injuries treated in the emergency
department with an incidence of 18%-44% of all hand fractures and 23% of forearm fractures
[1]. Metacarpal neck fractures are present and account to 10% of all hand fractures and
25%-36% of all metacarpal fractures [2]. Index, middle and ring metacarpal neck fractures
account to 6%,2% and 5% respectively while little finger is the most commonly involved
and accounts to 25% of the overall total [1,3]. The Fifth Metacarpal Neck Fracture (FMNF) also
called “Boxer fracture” occurs usually in young population with aggressive conduct. The
paradox is that professional boxer’s present fracture of neck in the index finger and not in the
little finger of the hand.
Male individuals have five times higher incidence than females, while the mean male
age with the greater incidence ranges from 19 to 29 years old [4]. It occurs most commonly
after alcohol intake and violence and also at athletic events [2,5]. The main typical cause of this
fracture is fighting, following by sporting injury, a traffic accident and rarely falls [6]. During
direct blow to solid object or another person, an axial load is transmitted to metacarpal bone
through knuckle, resulting fracture at the metacarpal neck area with dorsal angulation in
apex, due to the forces exerted by the pull of the interosseous muscles [7,8]. Displaced FMNFs
lead to rotational malalignment, volar angulation, loss of extension range of motion, loss of
strength and cosmetic distortion with loss of prominence of fifth metacarpal [9].
Despite the fact that volar angulation lead to metacarpal shortening, the transition zone
between shaft and the distal segment has not been defined [10,11]. A thorough search was
carried out through the electronic databases of Pubmed, Cochrane libraries, Google Scholar
from January 2000 to December 2020 using the following keywords «fifth metacarpal neck
fractures ” AND “Boxer fractures” AND “Classification fifth neck metacarpal
fractures” and 1162 reviews or research articles were retrieved. Only one manuscript refers
a classification for the metacarpal fractures from the Orthopaedic Trauma Association
(OTA) according to which, metacarpal fractures are divided into distal, shaft and proximal
segments [12]. All these manuscripts report their aspects to the topic indirectly, presenting
results either by applying a therapeutic method (conservative or surgical) or comparing
implant interventions. No researcher actually mentions any clear fracture pattern so can anyone really draw safe conclusions about the proper treatment?
Kvernmo ok that the fact of unclear diagnostic fracture pattern
leads to erroneous conclusions comparing different studies, which
hypothetically referred to the same topic mentioned as the fifth
metacarpal neck fractures [10]. Sletten et al. [11] reported that
metacarpal neck area is defined as the squared distance between
the insertions of the collateral ligament in the metacarpal head.
We believe that the OTA classification is very general based on the
anatomical elements of the bone and does not define any type of
fracture which occurs in subcapital area of fifth metacarpal bone. In
the present article a new classification system is proposed based on
the fractures pattern observed and the most appropriate method of
these fractures fixation is also suggested with the scope to achieve
the goal of treatment which is the full range of motion and returning
to previous functional status.
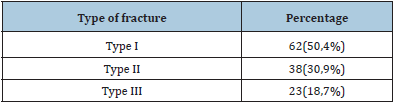
Classification System of 5th Neck Metacarpal Fracture
The study was performed at the Orthopaedic department of General Hospital of Heraklion- “Venizeleio” from January 2013 to December 2019. The Institutional Ethical Committee approved the study. Inclusion criteria were adults more than 18 years old with a traumatic unstable fracture of neck of fifth metacarpal (less than 10 days) and multiple fractures involving other metacarpals. Exclusion criteria included patients who had a history of metabolic bone disease, age <18 years with fracture of immature bone; old or operated fractures, neurologic involvement, or inability to return for follow-up care. One hundred twenty three patients were included in this study. One hundred twelve were males and eleven were females, with an average of 29 years old (range 20-54yrs old). The main cause of injury was punching a hard surface with a clenched fist, and the second statistical cause, was sport contact injuries. The right hand was involved in 100 and the left in 23 cases. In four cases the fracture was bilateral and caused by violent fight. In seven cases the fractures were open classified by Gustilo & Anderson in Grade 1(5 cases (4%)) and letter I (2 cases (1,6%)). Twelve patients were presented with a diaphyseal fracture of 4th metacarpal and fracture of neck of fifth (Table I).
Table 1:Demographic characteristics of patients.
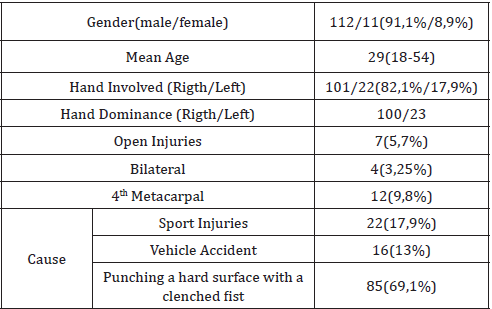
Figure 1:Type I fractures x-Rays (red arrow) AP (a,b), Oblique (c,d), (e) surgical evidence (dorsal comminution of neck - black arrow, head of metacarpal red arrow).
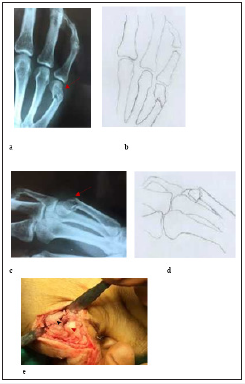
Initial radiographic examination with Anteroposterior (AP) and lateral radiographs were performed. With preoperative x-rays data and during surgical procedure findings, we noticed that all the fractures did not have the same type in terms of comminution, fracture line, and localization of fracture and seem different referring to the neck of fifth metacarpal. We classified all these fractures in three categories based on the fracture pattern mentioned above. We suggest as Type I, the fracture in which line extends obliquely from dorsal surface of the neck and expands proximally to diaphyses. In dorsal surface, there is comminution and in this area of metacarpal neck, the cancellous bone disappears (eggshell) while in volar surface there is more integrity respectively. In majority of cases the fracture presents also rotational deformity and a volar angulation (Figure 1). We suggest as Type II, the fracture in which line extends more proximally to diaphyses of metacarpal, without significant comminution and in the majority of fracture there is a volar angulation (Figure 2). We suggest as Type III, oblique fracture in which the proximal segment includes the head and neck of fifth metacarpal and presents shortening of the bone length and rotational deformity (Figure 3), (Table 2). In cases where simultaneous fractures of 4th diaphyseal metacarpal exist, the metacarpal neck fracture was type I.
Figure 2:Type II fracture, x-Rays (red arrow) AP (a,b), Oblique (c,d), surgical evidence (black arrow fracture, white arrow neck 5th metacarpal, grey arrow extensor digit minimi) (e).
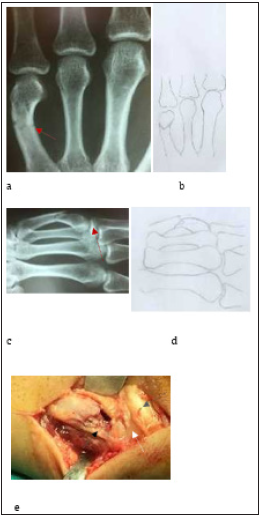
Figure 3:Type III fracture, x-Rays (red arrow) AP (a,b), Oblique (c, d), surgical evidence (black arrow oblique fracture of 5th metacarpal, white arrow head of metacarpal) (c).
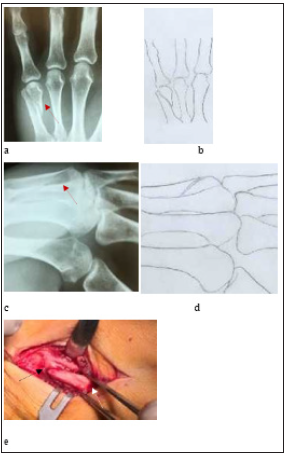
Table 2:Classification of fractures.
Author’s Surgical Treatment Option
All operations were performed by author and the indications
of surgical treatment were: angulation more than 40°, shortening
>3mm, rotational deformity and open injuries. After regional
anesthesia and tourniquet hemostasis control, all fractures were
operated with dorso-ulnar approach (except four cases with type
I fracture) with preservation of collateral ligament. In all cases
the internal fixation was provided with plates (locking and
convectional) and screws (Table 2). In “type I” fracture and in 32
cases the implants were blade plate convectional, while in rest
cases anatomical locking plate was used. In this group of fractures
the implant was applied in ulnar side of metacarpal in 56 cases and
in the rest cases the implant was applied on dorsal side of the bone
but with 3 screws on the neck area. In “type II” fractures a locking
plate in dorsal side of the metacarpal bone was applied in twelve
cases (with two or three locking screws in head of metacarpal),
while in the rest cases it was applied in ulnar side (in 11 patients
the plate was convectional and in 9 locking plate). In six cases from
this category of fractures a mini osteosynthesis is performed with
retrograde intramedullary headless cannulated screws.
In “Type III’ fracture a lag screw was applied in all cases which
compress the oblique fracture line and a plate was added to support
the fracture. In thirteen cases the screw applied separate (ulnar)
and the implant in dorsal side while in the rest cases, it was applied
threw the plate in ulnar side of the bone.
Postoperatively a palmar splint was worn for 5-7 days in order
to assist soft tissue healing while passive range of motion exercises
of the digits were initiated from the second postoperative day.
The sutures were removed in two weeks and functional support
was applied to protect the fixation until union. In this period all
the patients started a rehabilitation program which included scar
tissue management, edema control, continuous passive movement,
self-assisted and active exercises of fingers and home exercise
program. The median time of fracture union was 5,2 weeks.
In international literature the ideal management of boxer
fracture is still a matter of debate.14 In recent years as the surgical
technology progresses, implants are developed (low profile locking
plates) for these specific fractures. Internal fixation of FMNF is based
on the presumption that restoration of anatomy of metacarpal bone
and metacarpophalangeal joint with early mobilization of digits was
achieved and wrist will improve the ultimate functional outcomes.
Another reason for increased number of the internal fixation it was
the better understanding of biomechanical principles of internal
fixation.15 International literature presents many reports which
describe a wide range of surgical techniques for the treatment of FMNF: intramedullary K-wires, transverse K-wires, tension band,
locked intramedullary nailing, external fixation, and locking plate
fixation [13].
Zong et al. [14] report a meta- analysis of six studies and
suggest that locking plate is the first choice of surgical fixation of
FMNF [14]. These literature reviews compared all therapeutic
procedures based on criteria such as: complications (infection,
refracture, tendon injury, revision surgery, complex regional pain
syndrome), cost effective, time to healing and time to return in
daily activities [14-17]. The major complication is secondary
volar angulation post surgery which cause functional limitation
of 5th metacarpophalangeal joint [18]. Zhu et al. [18] compared
internal fixation of FMNF applied dorsal locking plates with two
and three locking screws in neck metacarpal area to determinate
the final angulation, and he suggested that “the fixation with
three distal locking screws could decrease the percentage of
secondary displacement and improve clinical outcomes”. It was also
recommended in order to achieve the three-screw fixation of distal
fragment, T-shaped plates (three distal holes) should be adopted
instead of Y-shaped (two distal holes) plates. In our series we have
posted operative volar angulation only in type I fractures and in
four cases, but the plate was applied in ulnar side of the bone and
the two locking screws were cut out. The paradox in this case was
that the patients have full range of motion [19,20].
Finally, our suggestion for the surgical treatment is in type I fracture condylar blade plate in ulnar side of the bone or dorsal locking plate with three distal screws in, to avoid postoperative angulation. In type II locking low profile plates or fracture antegrade intramedullary nail seems clinically to be an effective surgical procedure. The retrograde intramedullary headless cannulated screw is also a promising technique. In type III that the oblique line of the fracture must be restored to secure the initial length of bone a lag screw is obligatory to use for this reason and final a plate to secure the osteosynthesis must be performed. An alternative surgical procedure with antegrade intramedullary nail with two or three K-wires or an antegrade locking intramedullary nail is our surgical suggestion.
Conclusion
Fifth metacarpal neck fracture is the most common type of hand injury met in emergency department. It seems that every pattern of this fracture is not the same, so conclusively the therapeutic options should be different for best functional outcomes. In this article a new classification system is proposed which is based on the clearest definition of the main characteristics of fracture patterns in fifth metacarpal of the hand. The scope of this new suggested classification system is to define in details the type of fracture in order to choose the best surgical treatment achieving the goal of treatment which is the full range of motion and the regaining of previous functional mobility.
Conflict of Interest
The authors declare that have no conflict of interest.
Acknowledgments
We gratefully acknowledge the assistance of Miss Evagelia Kastani for her helpful sketching in this manuscript.
Ethical Approval
Our institution does not require ethical approval for reporting individual cases or case series.
References
- Padegimas EM, Warrender WJ, Jones CM, Ilyas AM (2016) Metacarpal neck fractures: a review of surgical indications and techniques. Arch Trauma Res 5(3): e32933.
- Gudmundsen TE, Borgen L (2009) Fractures of the fifth Acta Radiol 50(3): 296–300.
- Schadel Hopfner M, Wild M, Windolf J, Linhart W (2007) Antegrade intramedullary splinting or percutaneous retrograde crossed pinning for displaced neck fractures of the fifth metacarpal? Arch Orthop Trauma Surg 127(6): 435-440.
- Nakashian MN, Pointer L, Owens BD, Wolf JM (2012) Incidence of metacarpal fractures in US Hand (NY). 7(4): 426-430.
- Cotterell IH, Richard MJ (2015) Metacarpal and phalangeal fractures in athletes. Clin Sport Med 34(1): 69-98.
- Farag HE, Essawy OM (2015) Fifth metacarpal fractures: Treatment by low cost syringe Al – Azhar Assiut Medical Journal 13(Suppl 2): 134-138.
- Kamath JB, Harshvardhan, Naik EM, Bansal A (2011) Current concepts in managing fractures of metacarpal and Indian J Plast Surg 44(2): 203-211.
- Malik S, Herron T, Rosenberg N (2021) Fifth metacarpal fractures. Stat Pearls Publishing 29261999.
- Amsallem L, Pierrart J, Bihel T, Sekri J, Lafosse T, et al. (2018) Simplified internal fixation of fifth metacarpal neck fractures. Orthop Traumatol Surg Res 104(2): 257-260.
- Kvernmo HD (2018) Metacarpal neck In: Michel EH (edt.) Fractures of the hand and carpus. FESSH 2018 Instructional Course Book, Thieme E-Books, Algeria.
- Sletten IN, Hellund JC, Olsen B, Clementsen S, Kvernmo HD, et al. (2015) Conservative treatment has comparable outcomes with bouquet pinning of little finger metacarpal neck fractures: a multicentre randomized controlled study of 85 J Hand Surg Eur 40(1): 76-83.
- Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, et al. (2007) Facture and dislocation classification compendium 2007: Orthopaedic Trauma Association classification database and outcomes J Orthop Trauma 21(10 Suppl): S1-133.
- Zhu H, Bao B, Zheng X (2017) Three screws versus two screws fixation of distal fragment in fifth metacarpal neck fractures stabilized with locking Sci Rep 7(1): 12516.
- Zong SL, Zhao G, Su LX, Liang WD, Li LG, et al. (2016) Treatments for the Fifth Metacarpal Neck Fractures: A Network Meta-analysis of Randomized Controlled Medicine Baltimore 95(11): e3095.
- Corkum JP, Davison PG, Lalonde DH (2013) Systematic review of the best evidence in intramedullary fixation for metacarpal Hand (N Y) 8: 253–260.
- Facca S, Ramdhian R, Pelissier A, Diaconu M, Liverneaux P (2010) Fifth metacarpal neck fracture fixation: locking plate versus K-wire? Orthopaed Traumatol Surg Res 96(5): 506–512.
- Kollitz KM, Hammert WC, Vedder NB, Huang JL (2014) Metacarpal fractures: treatment and Hand (N Y). 9(1): 16–23.
- Zhu H, Xu Z, Wei H, Zheng X (2017) Locking plate alone versus in combination with two crossed Kirchner wires for fifth metacarpal neck fracture. Sci Rep 5(7): 46109.
- Sletten IN, Nordsletten L, Husby T, Ødegaard RA, Hellund JC, et al. (2012) Isolated, extra-articular neck and shaft fractures of the 4th and 5th metacarpals: a comparison of transverse and bouquet (intra-medullary) pinning in 67 patients. J Hand Surg Eur Vol 37(5): 387-395.
- Westbrook AP, Davis TR, Armstrong D, Burke FD (2008) The clinical significance of malunion of fractures of the neck and shaft of the little finger J Hand Surg Eur Vol 33(6): 732–739.
© 2021 Kastanis G. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






