- Submissions

Full Text
Orthoplastic Surgery & Orthopedic Care International Journal
Comparison of Minimal Invasive Subvastal Approach with Standard Medial Parapatellar Approach in Total Knee Replacement
Mohamed Nabil*
Orthopedic Surgery Department, Suez Canal University, Egypt
*Corresponding author: Mohamed Nabil, Orthopedic Surgery Department, Suez Canal University, Egypt
Submission: January 22, 2018;Published: February 23, 2018

ISSN: 2578-0069Volume1 Issue3
Abstract
Background: Although the long-term results of knee arthroplasty have proven to be excellent, the rehabilitation period often is long and painful. In order to improve the patient’s well-being in the immediate postoperative period, other less traumatic exposures have been introduced, including the mini subvastus approach. The purpose of this study is to evaluate the short-term functional results of MIS-TKA (mini-subvastus approach) compared with a traditional TKA using a medial parapatellar exposure.
Patients and methods:
The study population was divided into two groups of patients who underwent surgery with the same surgeon in 2014- 2015: 16 MIS-TKA and 18 medial parapatellar TKA, following the same arthroplasty model (nexgen) and similar pre and postoperative procedures.Results: In the immediate postoperative results, the subvastus group showed significant decrease in blood loss, significant decrease in hospital stay, significantly shorter length of incision, and significant increase in duration of surgery. After one year follow up, KSS scores were 86.6±7.0 for the MIS Group and 86.7±5.9 for the standard technique Group. This difference was not statistically significant.
Conclusion: this study asserts that the MIS technique does offer some advantages for the immediate post-operative period, including a lesser blood loss, and a shorter hospital stay. However, results at one year after surgery are similar, both in functional assessment and in quality of life for the patient.
Introduction
Total knee arthroplasty (TKA) is a very successful procedure in the treatment of end-stage arthritis of the knee. Long-term results for pain relief and functional improvement have been excellent. The procedure, however, traditionally requires an extensile approach. The medial parapatellar arthrotomy is the most common method used to expose the knee. This exposure involves patella eversion and generally is done through large incisions of approximately 20 to 30cm. Although the long-term results of knee arthroplasty have proven to be excellent, the rehabilitation period often is long and painful [1]. In order to improve the patient’s well-being in the immediate postoperative period, other less traumatic exposures (MIS-TKA) have been introduced, including the subvastus, midvastus, and lateral arthrotomy. The mini subvastus approach extends from the tibial tubercle to the superior patella and then to the muscle of the vastus medial is, and the muscle fibers are not cut [2]. Although recommendations for the use of this technique are not precisely defined yet, the exclusion criteria for patients to receive the MIS-TKA were rheumatoid arthritis, obesity, severe osteoporosis, valgus-varus deformity greater than 10°, previous arthrotomy on the knee and preoperative knee flexion lessthan 100°. These techniques aim for a faster recovery of mobility, a shorter postoperative period, a reduction in blood loss, less pain throughout the postoperative period, a lessened aesthetic impact, and to reduce the amount of health resources required by resorting to a smaller incision and a less aggressive technique for soft tissues; they will not, however, impair the good results this procedure achieves [3].
Objectives
The purpose of this study is to evaluate the short-term functional and health-related quality of life results of MIS-TKA (mini-subvastus approach) compared with a traditional TKA using a medial parapatellar exposure. Additionally, this study examines the effect of MIS-TKA on operative time, blood loss, size of incision, duration of hospital stayand postoperative well-being.
Methods
This is a prospective comparative and randomized study. Data were collected before surgery, at immediate follow-up and at one year of follow-up. All patients suffered from knee osteoarthritis, which had not improved with medical treatment and which presented a less than 10° deformity in the coronal and sagittal radiographic projections Patients who already had gone through previous knee surgery other than arthroscopy were excluded. The study population was divided into two groups of patients who underwent surgery with the same surgeon in 2014-2015: 16 MIS-TKA and 18 medial parapatellar TKA, following the same arthroplasty model (nexgen) and similar pre and postoperative protocol. Using a table of random numbers, patients would be allocated to either the minimally invasive group (MIS-TKA) (group A) or the standard group (group B) prior to surgery. The type of surgery was explained to the patient in the moment of random assignment. Written informed consent was obtained from all patients. Demographic, clinical, and radiographic data were collected and measured by the author. Preoperative data were similar in both groups (Table 1). All knee prosthesis were Nexgen mobile bearing as primary surgery. All the implants used in this study were cemented, and all patients had patella debridement. A third-generation cephalosphorins antibiotic prophylaxis was used during perioperative care, and low-molecular-weight subcutaneous heparins were administered as antithrombotic treatment for three weeks after surgery.
Table 1: Preoperative data.
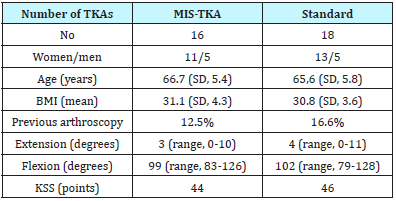
Preoperative data
A specific questionnaire was filled in, and the KSS scale was filled in at one year after the intervention. Data were processed with Microsoft Excel 2007. Man-Whitney U test was used to measure significance of variables and Significant p-value (2-tailed) was at <0.01. A computerized SPSS program was used for data statistical analysis and graphs formulation.
Data collected
1-Surgery duration (min)
2-Size of incision (cm).
3-Length of post-operative hospital stays (days).
4- Suction draining (cc).
5- Complications.
Approach and Technique
Standard medial parapatellar approach
The prosthesis will be inserted via a mid-line skin incision beginning over the medial portion of the quadriceps tendon, four inches above the upper border of the patella. The incision will continue in a gentle curve following the medial margin of the quadriceps tendon, patella and patella tendon. It will then cross the upper end of the tibia and end inferior to the tubercle of the tibia. A straight incision will be made through the three layers of fascia over the quadriceps and the patella tendons. The synovia and deep aponeurosis will be divided medial to the patella and the quadriceps tendon will be separated in the line of its fibers just lateral to the insertion of the vastus medialis. The patella tendon will be freed along its medial border to the level of the tibia tubercle, exposing the infrapatellar bursa. The patellar will be dislocated laterally [4- 7].
Sub-vastus approach
The skin incision in the mini sub-vastus Group was made along the medial aspect of the patella and from 0.5-1cm proximal to the superior pole of the patella to approximately 2-4cm beyond the medial extent of the tibial tubercle. The distal insertion of the vastus medialisobliqus (VMO) on the patella is exposed. The fascia overlying the VMO is released sharply, taking care not to injure any underlying muscle fibers. The fascia is released posteriorly towards the attachment of the VMO on the medial inter muscular septum. This exposes the entire distal extent of the VMO. Using blunt dissection, a finger can be placed underneath the VMO at its inferior border. The VMO is then retracted proximally and laterally while maintaining its attachment to the patella. AZ-retractor is inserted anterior to the distal femur and deep to the muscle to maintain retraction. Distally, the medial para patellar retinaculum was incised and the incision was continued medial to the patellar tendon to the tibia approximately 5mm medial to the tubercle. The knee was flexed and the patella was subluxed, but not everted, and the technique “mobile windows” was carried out so as to better visualize the femorotibial compartments. The femoral and tibial incisions are performed with the specific equipment. In the standard group, intramedullary guides were used for the distal femoral cut, with a target alignment of 5° of valgus with 3° of flexion. The proximal tibia was cut using extra medullary guides at right angles in the coronal plane and at 3° of posterior slope. After these cuts were made, all remaining posterior osteophytes and meniscal remnants were removed. Ligament balancing was accomplished using either spacer blocks or a tension/balancer. Final preparation was performed with a 4-in-1 cutting block. The wound was closed routinely with 1 drain. A tourniquet was used in all cases and deflated routinely before the wound closure [1,8].
Assessment of outcome
The primary outcome measure for this study will be the Knee Society Score [9] at one year postoperative, and will be carried out by a trained independent assessor (physiotherapist) who will be blinded to the surgical approach taken.
Secondary outcomes -patient based
a) Operative duration.
b) Operative incision.
c) Postoperative blood loss.
d) Duration of hospital stay.
Results
Surgery
Figure 1: The duration of operation in minutes.

Figure 1 shows the Mean duration of the surgery for Group B was 99.4 minutes (SD 4.46), while the mean time for Group A was 114.9 minutes (SD 6.2). This means applying the MIS technique required more time (p < 0.0001).
Figure 2: The mean size of the length of the cutaneous incision.
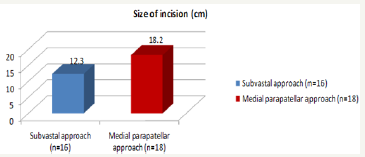
Figure 2 shows the mean size of the length of the cutaneous incision was 12.3 cm (11-14) for the MIS-TKA group and 18.2 cm (16-21) for the group using the traditional method.
Immediate Post-operative Period
Figure 3: The hospital stays duration.

Figure 4: Postoperative blood loss.
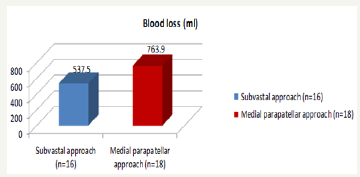
Figure 3 shows the hospital stay duration is noticeably shorter (P=0.0014) for the MIS group patients (mean: 7±0.73) than for the standard group (mean: 7.9±0.76).
Figure 4 shows the drainage volume collected after surgery for group A has a mean of 537.5±80.6cc , whereas the figure for the traditional technique is significantly higher (P<0.0001), with a mean of 763.9±44.7cc.
Evaluation at one year
Regarding the observed mobility at one year after surgery, no significant differences were observed between both groups. Extension in the MIS Group was -0.5° (SD 2.23), and -0.6° (SD 2.14) in the standard Group. Mean flexion for the MIS Group was 107.4° (SD 9.45), whereas it was 105.23° (SD 10.3) in the standard group. There were no severe complications which might have altered the clinical or radiographic results. KSS scores were 86.6 for the MIS Group and 86.7 for the standard technique Group. This difference was not statistically significant (Figure 5, Figure 6a & 6b).
Figure 5: KSS score after 12 months.
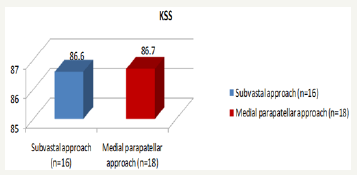
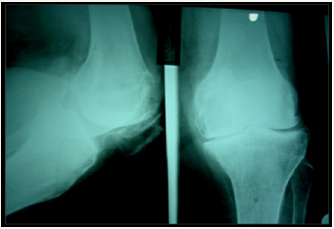
Figure 6: Preoperative X- ray.
Discussion
There have been many studies which have determined the effectiveness of TKA in reducing pain and deformity and improving function. Standard TKA has led to consistent, reproducible, and enduring results. Long term success at 10 years or more encompasses survivorship of greater than 90% for many studies, and more than of 80% of patients were satisfied [5-7]. For many years, clinicians relied exclusively on objective and physical measures of disability in order to assess orthopedic surgical outcomes [10,11]. Most have assessed outcomes using standardized knee scoring systems such as KSS.
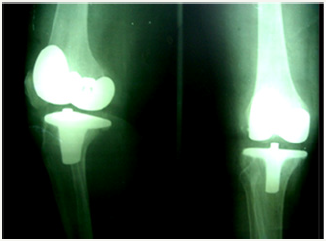
Figure 7: Postoperative X- ray.
Few studies exist which have compared prospectively two groups of patients [2-4], one with MIS, one with the standard technique and, it compares both groups via functional scales, which is important to assess a technique proposed to enhance patient’s satisfaction and cosmetic benefits. Furthermore, it is a prospective, randomized study in which the same type of prostheses were implanted by the same surgeon [11,12].
The mean operative duration was significantly longer in group MIS-TKA; this was already referred to in other studies on MIS [13,14]. Hospital stay for patients in Group A was significantly less than that of patients who underwent the traditional technique. Other authors agree with this [14] which helps to make good use of health resources. Blood loss was significantly lower in the MIS Group. These data are also in keeping with other studies [2-4] and are supposedly related to the less aggressive surgery. In any case, none of the patients needed to get a blood transfusion.
We encountered no major perioperative complications in either group. It is possible that being more meticulous with the soft tissues may have avoided the high number of cutaneous complications. At one year of follow-up, results for both groups are similar, and there are no statistically significant differences in KSS score. The range of motion in both groups is good at one year; these data are in keeping with other authors, [2-4,14] where the minimally invasive technique positively contributes to the early restoration of quadriceps strength and a speedy return to normal functioning. In other studies, manipulation was necessary in 14% of the traditional group compared with 2% in the minimal incision group [14] but there was no significant difference in range of motion or functional outcome at 1 year after surgery nor was no significant difference in component position or complication rates.
Both groups reported a good quality of life at one year. On the KSS scale, both groups achieved high scores, but there were no statistically significant differences between them. It is usual that studies appear showing better short-term outcomes for MIS-TKA [13] regarding the patient’s well-being and hospital stay. However, in order to properly gauge the scientific evidence on MIS techniques, it should be noted that those results have frequently been obtained from expert centers or from surgeons devoted to such techniques [14]. This fact may distort the results, since any complications and the follow-up of TKAs implanted via MIS in general hospitals or non-specialized centers are not analyzed. It is possible then that, presently, the MIS technique is more a personal choice of the patient or a commercial demand than a true advancement in TKA placement. The surgeon should look for the minimum size necessary for him to correctly implant a TKA, and look away from showing off he is able to implant arthroplasties with ever smaller incisions. Therefore we recommend the use of a standard arthrotomy with the shortest possible invasion and skin incision. MIS-TKA demands an effort on the part of the surgeon [2,4], the learning curve may be unacceptably long for a low-volume arthroplasty surgeon, [13,14] it takes more intervention length, require longer tourniquet time and special tools are needed to insert the implant.
Conclusion
This study declares that the MIS technique does offer some advantages for the immediate post-operative period, including a lesser blood loss, and a shorter hospital stay. However, results at one year after surgery are similar, both in functional assessment and in quality of life for the patient.
References
- Hofmann AA, Plaster RL, Murdock LE (1991) Subvastus (southern) approach for primary total knee arthroplasty. Clinical Orthopaedics 269: 70-77.
- Fauré BT, Benjamin JB, Lindsey B, Volz RG, Schutte D (1993) Comparison of the subvastus and paramedian surgical approaches in bilateral knee arthroplasty. J Arthroplasty 8(5): 511-516.
- Maric Z, Ott DM, Karpman RR (1991) The standard versus the sub-vastus (southern) approach for total knee arthroplasty: a randomised prospective study. Orthop Trans 15: 43.
- Bindelglass DF, Vince KG (1996) Patellar tilt and subluxation following subvastus and parapatellar approach in total knee replacement. J Arthroplasty 11(5): 507-511.
- Ogata K, Ishinishi T, Hara M (1997) Evaluation of patellar retinacular tension during total knee arthroplasty. Special emphasis on lateral retinacular release. J Arthroplasty 12(6): 651-656.
- Cameron HU, Fedorkow DM (1982) The patella in total knee arthroplasty. Clinical Orthopaedics 165: 197-199.
- Wetzner SM, Bezreh JS, Scott RD, Bierbaum BE, Newberg AH (1985) Bone scanning in the assessment of patellar viability following total knee replacement. Clin Orthop Relat Res 199: 215-219.
- Smigielski M, Gustke K (1989) Southern approach for total knee replacement. Florida Orthopaedic Society, USA.
- Insall JN, Dorr LD, Scott RD, Scott NW (1989) Rationale for the knee society clinical rating system. Clin Orthop Relat Res 248: 13-14.
- Barrack RL (1997) Resurfacing of the patella in total knee arthroplasty. Journal of Bone and Joint Surgery 79(8): 1120-1121.
- Pocock SJ (1991) Clinical trials a practical approach. Ed John Wiley and Sons, USA, pp. 1-278.
- Engh GA (2002) Subvastus approach in surgical techniques in total knee arthroplasty. In: Scuderi GR, Tria AJ (Eds.), Springer-Verlag, New York, USA, pp. 127-130.
- Roysam GS, Oakley MJ (2001) Subvastus approach for total knee artroplasty. A prospective, randomised and observer-blinded trial. J Arthroplasty 16(4): 454-457.
- Bridgman S, Walley G, MacKenzie G, Clement D, Griffiths D, et al. (2006) Sub-vastus approach versus the medial parapatellar approach in primary total knee: a randomised controlled trial. Trials 7: 23.
© 2018 Mohamed Nabil. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






