- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
An Unusual Case of Tako Tsubo Cardiomyopathy and Complete Atrioventricular Block
Alberto Hidalgo Mateos*, Ester Galiana Talavera, Amparo Valls Serral, Paula Gramage Sanchis and Juan Geraldo Martinez
Department of Cardiology of Hospital Doctor Peset, Av. de Gaspar Aguilar, 90, 46017 València, Valencia, Spain
*Corresponding author: Alberto Hidalgo Mateos, Department of Cardiology of Hospital Doctor Peset, Av. de Gaspar Aguilar, 90, 46017 València, Valencia, Spain
Submission: September 11, 2023;Published: November 16, 2023

ISSN 2578-0204Volume4 Issue3
Abstract
We introduce a case of a 71-year-old patient with Tako-tsubo syndrome with an atypical initial presentation of complete atrioventricular block that led to rethink therapeutic management because of the unusual manifestation of this pathology. We emphasize any event that has happened as both entities can be concomitantly, and it is important to determine which entity precipitates the other to evaluate the therapeutic orientation.
Keywords:Takotsubo syndrome; Obstructive coronary artery disease; Atrioventricular block
Introduction
Takotsubo syndrome (TS), is a reversible form of left ventricular systolic dysfunction resembling acute coronary syndrome, in the absence of obstructive coronary artery disease. It is usually caused by a stressful situation and it is frequent in postmenopausal women. Prognosis is often good but severe complications can occur, especially in the acute phase. Complete atrioventricular block (CHB) has been described accompanying TS although few cases have been reported [1]. We present a case of concurrent TS and CHB to highlight management strategies in this situation.
Case Presentation
A 71 years old woman was evaluated for weakness and exertional dyspnea during the last 48 hours. She denied chest pain. Electrocardiography (ECG) showed sinus rhythm with CHB (Figure 1A). On examination she had pulmonary rales. NT-pro BNP was 2130pg/ml and serum troponin I US was 1503,2pg/ml. X ray showed interstitial edema and cardiomegaly. She was admitted in intensive care unit and treated with isoprotenerol and furosemide, recovering atrioventricular conduction. Transtoracic echocardiogram (TTE) showed akinesia of middle and apical anterior, lateral and septum segments with a left ventricular ejection fraction (LVEF) of 30%. On the second day, a coronary angiogram was performed showing normal epicardial coronary arteries. A cardiac magnetic resonance imaging was performed excluding necrosis areas and confirming a LVEF of 30%. On third day, the patient developed again CHB with a left bundle branch block (LBBB) and depressed LVEF persisted, so that a diagnosis of dilated cardiomyopathy with CHB was presumed and placement of an implantable cardioverter defibrillator (ICD)/biventricular pacemaker was decided. ECG showed deep T-wave inversions in precordial leads and prolonged QTc (Figure 1B).
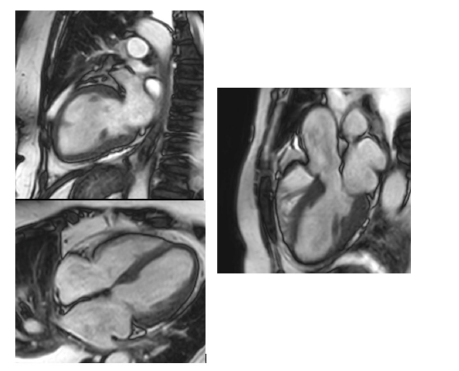
Due to anatomical problems the implantation of biventricular pacemaker was not possible and an ICD/conventional pacemaker was placed instead. After clinical improvement, diuretic treatment was withdrawn and beta-blockers and angiotensin-converting enzyme inhibitors were started. A TTE was repeated after 12 days, showing resolution of the contractility abnormalities with a LVEF of 50%. ECG showed sinus rhythm with paced ventricular complexes and normal QTc interval and T waves (Figure 1C). The diagnosis was then reconsidered to a TS and the patient was discharged without medical treatment. After eight weeks, interrogation of pacemaker revealed underlying Wenckebach blockage and a TTE showed a normal LVEF (Figure 2).
Figure 1:A: ECG on admission: Sinus rhythm and complete atrioventricular block. B: ECG on 5th day showing deep T-wave inversions in the lateral leads. C: ECG after device placement: Sinus rhythm with paced ventricular complexes and normal QTc interval and T waves.

Figure 2:Results of cardiac magnetic resonance: hypokinesia of the middle, apical and apex segments of the left ventricle.
Discussion
Our patient was presented with CHB and acute heart failure. TTE showed low LVEF that lead to the diagnosis of dilated cardiomyopathy and TS diagnosis was missed until later on. CHB has been reported in 1,3-3% of TS patients [2,3]. Most of them had both CHB and TS at initial presentation and it can be difficult to determine which entity triggers the other. The damaged segment in TS is away from the atrium and bundle of His, thus TS is not likely to cause the CHB. The stress induced by the CHB might induce TS. On the other hand, the prevalence of TS is increased in elderly woman, a population in which conduction can be damaged by aging. In our case we think the block precipitated TS since it persisted eight weeks after the event.
Stiermaier et al. [3] report that TS patients who underwent pacemaker continued to be in CHB on long-term follow-up. Besides, patients who had CHB or ventricular asystole at presentation but did not undergo pacemaker implantation had sudden deaths on follow-up.
Our patient certainly had an indication of a pacemaker, since the conduction abnormality in most of cases of TS and CHB persisted for a long time [4]. After 8 weeks she still had a seconddegree blockage on the pacemaker interrogation. Nevertheless, the ICD and biventricular pacing was probably not necessary as long as LVEF was recovered in a few days. Ventricular arrhythmias can occur in acute phase of TS and ICD has been indicated in selected patients although they did not require device interventions during long-term follow-up [5]. Our patient did not have ventricular arrhythmias either.
Conclusion
In conclusion, it is important to bear in mind that both entities, TS and CHB, may occur at the same time and the clinical challenges are firstly determining which entity precipitates the other and secondly [6,7] evaluating the need for a cardiac implantable device. It would be advisable to manage patients with arrhythmias and TS cautiously with temporary pacemaker or wearable cardioverter defibrillator before deciding permanent device implantation.
References
- McGee MJ, Yu W, McCarthy J, Barlow M, Hackworthy R (2020) Complete heart block complicating takotsubo syndrome: Case Report and literature review. Case Rep Cardiol 2020: 7614836.
- Malanchini G, Del Corral MP, De Filippo P, Ferrari P, Solomon A, et al. (2020) Cardiac arrhythmias and In-hospital mortality amongst patients with takotsubo cardiomyopathy: A retrospective study in an Italian population. Int J Cardiol Heart Vasc 31: 100608.
- Stiermaier T, Rommel KP, Eitel C, Eitel I, Möller C, et al. (2016) Management of arrhythmias in patients with Takotsubo cardiomyopathy: Is the implantation of permanent devices necessary? Heart Rhythm 13(10): 1979-1986.
- Korantzopoulos P, Nikas DN, Letsas K, Gkirdis I, Goudevenoset J, et al. (2015) High-grade atrioventricular block and takotsubo cardiomyopathy: Case report and review of the literature. Int Cardiovasc Res J 9(2): 119-124.
- Migliore F, Zorzi A, Peruzza F, Marra MP, Tarantini G, et al. (2013) Incidence and management of life-threatening arrhythmias in Takotsubo syndrome. Int J Cardiol 166(1): 261-263.
- Rathore A, Banavalikar B, Shenthar J, Acharya D, Parvez J, et al. (2018) An unusual case of complete atrioventricular block causing Takotsubo syndrome. Indian Pacing and Electrophysiology Journal 18(3): 123-125.
- Revilla Martí P, Cueva Recalde JF, Linares Vicente JA, Río Sánchez S, Ruiz Arroyo JR, et al. (2021) High-degree atrioventricular block. An unusual presentation of Takotsubo cardiomyopathy: A case report. Egypt Heart J 73(1): 18.
© 2023 Alberto Hidalgo Mateos. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






