- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Painful Left Bundle Branch Block Syndrome: An Underrecognized Entity
Badre El Boussaadani1*, Ourtassi H2, Benali M1 and Zainab R1
1Cardiology Department of Tangier University Hospital, Abdelmalek Essaadi university, Morocco
2Cardiology B Department of CHU Ibn Sina, Morocco
*Corresponding author: Badre El Boussaadani, Cardiology Department of Tangier University Hospital, Abdelmalek Essaadi university, Morocco
Submission: November 04, 2022;Published: December 13, 2022

ISSN 2578-0204Volume4 Issue1
Abstract
Painful Left Bundle Branch Block (LBBB) syndrome is a rare condition, defined by an exertional chest pain associated with intermittent LBBB in the absence of myocardial ischemia. The exact mechanism is still unclear. Various treatments were described, conduction system pacing such as His Bundle Pacing or Left Bundle Branch Area Pacing have proven to be most effective. The present report introduces the case of A 52-year-old male presented with a constrictive chest pain. ECG on admission showed a complete LBBB with a precordial S/T wave ratio of 2.3. Chest pain disappeared simultaneously after resolution of LBBB. Stress myocardial perfusion scan revealed an onset of chest pain concomitant with a transition to complete LBBB in the second stage, along with an aspect of myocardial ischemia. Complementary coronary angiography was normal, a negative Methergin testing eliminated the possibility of a vasospasm. Based on the above-mentioned findings we diagnosed “Painful LBBB Syndrome”. After debating all therapeutic options, The patient was initially treated with Betablockers with no improvement. Therefore, it was decided to refer him for His Bundle Pacing.
Keywords: Chest pain; Painful left bundle branch block; Myocardial ischemia; His bundle pacing
Introduction
Painful Left Bundle Branch Block (LBBB) syndrome is a rare condition, defined by the association of exertional chest pain with intermittent left bundle branch block (LBBB), in the absence of myocardial ischemia [1]. Its exact mechanisms are still unclear; the most postulated hypotheses include dyssynchronous systolic motion of the septum and generalized interoceptive sensitivity [2]. Treatment options such as submaximal exercise regimens, b-blockers, Right Ventricular (RV) and biventricular pacing, have only shown modest success [3]. Conduction system pacing, namely permanent His Bundle Pacing (HBP) and Left Bundle Branch Area Pacing (LBBAP), has recently proven to be more effective for patients with painful LBBB syndrome. With less than 60 cases reported in the literature [2], this condition continues to be underdiagnosed especially when coronary artery disease is associated. The present study will report one case of painful LBBB syndrome, highlighting its clinical, electrocardiographic, nuclear imaging and angiogram features.
Case Report
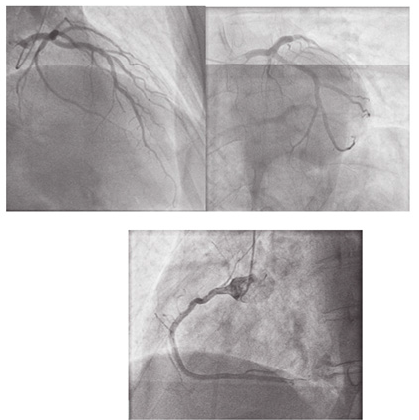
A 52-year-old male with a history of active smoking and hypertension was admitted to the ER for a constrictive chest pain radiating to the left arm, persistent for 15 minutes, associated with a hypertensive spike. ECG on admission revealed a complete LBBB with a precordial S/T wave ratio of 2.3 (Figure 1) followed by a spontaneous transition to sinus rhythm with narrow QRS complexes (Figure 2) a few minutes later, concomitant with pain resolution. The patient was discharged against medical advice and performed a week later a Stress Myocardial Perfusion Scan (SPECT) which revealed a transition to complete LBBB in the second stage, concomitant with an onset of chest pain, and an aspect of myocardial ischemia in the basal third of the anterior wall (1 segment /17) and a chronic hypoperfusion of the anteroseptal segment, most probably linked to the LBBB (Figure 3). Complementary coronary angiography was normal, with a negative Methergin testing that could eliminate the possibility of a vasospasm (Figure 4). Based on the abovementioned findings we diagnosed Painful LBBB Syndrome. After debating all therapeutic options, The patient was initially treated with Betablockers but did not report any improvement. The case was discussed over a staff meeting concluding to the necessity to refer the patient to a specialized center for His Bundle Pacing.
Figure 1:ECG on admission revealing a complete LBBB at a heat rate of 72 bpm, normal QRS axis, with a precordial S/T wave ratio of 2.3 concordant with a new-onset LBBB.
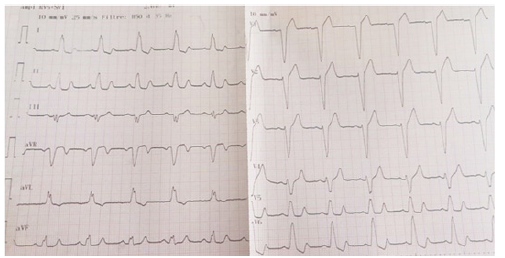
Figure 2:ECG revealing spontaneous transition to narrow QRS complexes concomitant with pain resolution.
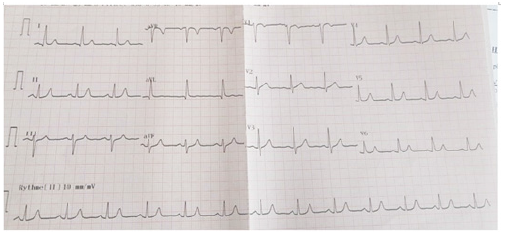
Figure 3:Stress Myocardial Perfusion Scan (SPECT) revealing an aspect of myocardial ischemia in the basal third of the anterior wall (1 segment /17) and a chronic hypoperfusion of the anteroseptal segment, most probably linked to the LBBB.
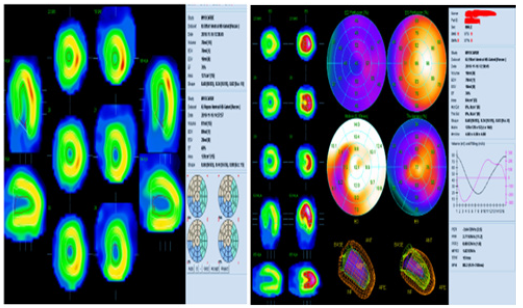
Figure 4:Normal coronary angiography, with negative Methergin testing.
Discussion
Painful LBBB syndrome was first described in 1946 [4]. Since then, less than 60 cases were reported in the literature [2]. That must be due to the fact that this condition is underdiagnosed, especially when associated with coincidental coronary artery disease. Indeed, reports have ruled out myocardial ischemia as the cause of painful LBBB syndrome. The onset/ offset character of pain, the failure of Nitroglycerine to relieve pain [5], the resolution of pain after conversion from intermittent to permanent LBBB [6], the invariable absence of perfusion defects on nuclear imaging and coronary sinus lactate sampling data were all argument against ischemia [7,8]. Vasospasm was also ruled out by ergotamine infusion at the time of coronary angiography [2]. Thus, it is important to objectively document myocardial ischemia before linking LBBB to the sole angiographic presence of coronary artery disease. The exact mechanisms of painful LBBB are yet to be perfectly elucidated, the most postulated hypotheses include the alteration of ventricular activation pattern as observed by kinetography and cardiac MRI, associated with an increase in generalized interoceptive awareness [3].
When it comes to the diagnosis of painful LBBB syndrome,
Shvilkin et al. [2] established in 2016 the following criteria:
1. Abrupt onset of chest pain coinciding with the
development of LBBB.
2. Simultaneous resolution of symptoms with resolution of
LBBB (although occasionally a walk-through phenomenon may
be present);
3. Normal 12-lead ECGs before and after LBBB (occasionally
T-wave inversions may be present with morphology pattern
consistent with that of T-wave memory).
4. Low precordial S/T wave ratio (measured immediately
after LBBB onset) consistent with new-onset LBBB (<1.8 in
their series) and inferior QRS axis.
5. Absence of myocardial ischemia during functional stress
testing.
6. Normal left ventricular function and the absence of other
abnormalities to explain symptoms.
In our case, chest pain was concomitant with LBBB finding and disappeared simultaneously after resolution of the latter, as documented on ECG. However, the S/T wave ratio could not be measured immediately after LBBB onset. In a retrospective study, a precordial S/T wave ratio of <2.5 separated new-onset LBBB (<24- hour duration) from chronic LBBB with 100% sensitivity and 89% specificity [9], which makes our case a new-onset LBBB with a 2.3 ratio.
Nuclear imaging on the other hand, showed defects that were considered to be false positives. Indeed, the presence of a left bundle branch block is a well-known factor that is frequently associated with false-positive stress perfusion findings [10,11]. Another argument that ruled out the possibility of myocardial ischemia was the finding of a normal coronary angiography, along with a negative methergin test. There are various treatments reported in the literature to relieve symptoms of painful LBBB syndrome such as a physical exercise regimen, AV nodal blockers [12], right ventricular and biventricular pacing, showing modest success [3]. More recently, His Bundle Pacing (HBP) has shown to be very effective in resolving LBBB and associated symptoms [2,3]. However, routine use of HBP might necessitate lead revisions due to higher capture thresholds at implantation and increased risk for late rise in HBP thresholds [13]. Left Bundle Branch Area Pacing (LBBAP) is another technique that can significantly narrow the QRS duration in patients with LBBB according to recent studies by Vijayaraman et al. [14] and Zhang et al. [15]. The two first known cases to be successfully treated with such technique were reported by Garg et al, achieving complete resolution of the LBBB, narrowing of QRS, and a significant improvement of symptoms. The advantage of this technique is avoiding the sensing- and threshold-related issues seen with HBP. However, more studies are necessary in order to determine the best pacing modality in painful LBBB syndrome.
Conclusion
Painful LBBB syndrome continues to be an underrecognized disorder especially that it can coexist with coronary artery disease. It should be suspected in patients with chest pain and LBBB in the absence of ischemia. Further criteria such as ECG features could be used to enforce the diagnosis. Chest pain in this condition is most likely due to ventricular dyssynchrony caused by LBBB. Many treatment options have been reported, however, the most successful ones so far are based on conduction system pacing (His bundle or LBBA) which can result in complete resolution of LBBB and associated symptoms.
References
- Loubeyre C, Tison E, Neuville C, Degroote P, Ducloux G (1991) The block of branche gauche douloureux d'effort. Ann Cardiol Angeiol 40: 613-617.
- Shvilkin A, Ellis ER, Gervino EV, Litvak AD, Buxton AE, et al. (2016) Painful ful left bundle branch block syndrome: Clinical and electrocardiographic features and further directions for evaluation and treatment. Heart Rhythm 13(1): 226-232.
- Suryanarayana PG, Frankel DS, Marchlinski FE, Schaller RD (2018) Painful left bundle branch block syndrome treated successfully with permanent His bundle pacing. Heart Rhythm Case Reports 4(10): 439-443
- Eichert H (1946) Transient bundle branch block associated with tachycardia. Am Heart J 31: 511-518.
- Vieweg WV, Stanton KC, Alpert JS, Hagan AD (1976) Rate-dependent left bundle branch block with angina pectoris and normal coronary arteriograms. Chest 69(1): 123-124.
- Bory M, Karila P, Sainsous J, Cohen S, Djiane P, et al. (1985) Simultaneous appearance of precordialgia and a block of the branche gauche on exertion. Study in 6 patients with normal coronary angiography. Arch Mal Coeur Vaiss 78(9): 1326-1331.
- Kafka H, Burggraf GW (1984) Exercise-induced left bundle branch block and chest discomfort without myocardial ischemia. Am J Cardiol 54: 676-677.
- Ninan M, Swan J (2002) Can left bundle branch block cause chest pain? Br J Cardiol 9: 230-232.
- Shvilkin A, Bojovic B, Vajdic B, Gussak I, Ho KK, et al. (2010) Vectorcardiographic and electrocardiographic criteria to distinguish new andold left bundle branch block. Heart Rhythm 7(8): 1085-1092.
- O'Keefe JH, Batman TM, Silvestri R, Barnhart C (1992) Safety and diagnostic accuracy of adenosine thallium-201 scintigraphy in patients unable to exercise and in those with left bundle branch block. Am Heart J 124(3): 614-621.
- Larcos G, Gibbons RJ, Brown ML (1991) Diagnostic accuracy of exercise thallium-201 single photon emission computed tomography in patients with left bundle branch block. Am J Cardiol 68(8): 756-760.
- Heinsimer JA, Skelton TN, Califf RM (1986) Rate-related left bundle branch block with chest pain and normal coronary arteriograms treated by exercise training. Am J Med Sci 292(5): 317-319.
- Bhatt AG, Musat DL, Milstein N, Pimienta J, Flynn L, et al. (2018) The efficacy of His bundle pacing: lessons learned from implementation for the first time at an experienced electrophysiology center. JACC Clin Electrophysiol 4(11): 1397-1406.
- Vijayaraman P, Subzposh FA, Naperkowski A, Panikkath R, John K, et al. (2019) Prospective evaluation of feasibility, electrophysiologic and echocardiographic characteristics of left bundle branch area pacing. Heart Rhythm 16(12): 1774-1782.
- Zhang W, Huang J, Qi Y, Wang F, Guo L, et al. (2019) Cardiac resynchronization therapy by left bundle branch area pacing in patients with heart failure and left bundle branch block. Heart Rhythm 16(12): 1783-1790.
© 2022 Badre El Boussaadani. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






