- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Reviewing the Basics of Atherosclerosis
Kencis L1, Garcia Caluz NPE1, Saldanha ALR1, Valera Gasparoto AL2, Pantoja Margeotto AP1, Garcia Nosé PM2, Carvalho Abdala BD1, Scartezini M1 and Rocha Martinez TL1*
1Nephrology Department, BP, A Beneficência Portuguesa de São Paulo, Brazil
2Intensive Care Unit, BP, A Beneficência Portuguesa de São Paulo, Brazil
*Corresponding author: Rocha Martinez TL, Nephrology Department, BP, A Beneficência Portuguesa de São Paulo, São Paulo, Brazil
Submission: March 31, 2022;Published: July 18, 2022

ISSN 2578-0204Volume3 Issue5
Abstract
The growing interest in the mechanisms involved in atherogenesis is justifiable when it is verified that most of the deaths occurred in the Western world are due to ischemic syndromes related to atherosclerotic disease, that is, coronary insufficiency, cerebral vascular and peripherical vascular. The basis for formulating the lipid infiltration hypothesis for atherogenesis dates back to studies from the beginning of the century, when spontaneous atherosclerotic lesions in rabbit aortas were described. Ignatowiski and Anitshkow demonstrated that rabbits fed diets high in saturated fat and cholesterol developed atherosclerotic lesions in the aorta. Experimental studies “in vitro” and “in vivo”, using animal model, carried out in recent decades, which elucidated the properties of Low Density Lipoproteins (LDL) and their oxidative modifications, allowed a hypothesis to be proposed for the development of atheroma based on elevated LDL levels.
Keywords: Atherogenesis; Atherothrombotic lesion; Lipoproteins; Triglycerides Remnants; Lipoprotein(a)
Abbreviations: HDL: High Density Lipoprotein; HDL-c: High Density Lipoprotein Cholesterol; IDL: Intermediate Density Lipoprotein; LCAT: Lecithin Cholesterol Acyl Transferase; LDL: Low Density Lipoprotein; LDL-c: Low Density Lipoprotein Cholesterol; Lp(a): Lipoprotein(a); VLDL: Very Low Density Lipoprotein
Pathophysiology of Atherosclerosis
Atherosclerosis is a progressive, multifactorial disease characterized by lipid accumulation, with cell proliferation, causing endothelial dysfunction, thrombosis and inflammation [1- 3]. Hypercholesterolemia is associated with coronary atherosclerosis. Duguid and Aberd were the first to suggest that lipids come from degenerate thrombi (1939). Golfman et al. in a weekly publication on the role of lipids and lipoproteins in atherosclerosis, showed an association between lipoprotein fractions and the risk of atherosclerosis. Chandler, Hand first enunciated the concept of atherothrombosis [4]. In 1987, Glagov [4] demonstrated that there was widening of the coronary artery wall in the sense of accommodating the atherosclerotic plaque. Despite the evolution of the disease, the lumen was not compromised until very late, or rather, until it occupied 40% of the lumen of the vessel. Thus, it was evident that atherosclerosis was linked to lipid accumulation, and that it was intuitive to evaluate the fall in lipid levels and the study related to angiographic progression or regression. Statin therapy does not significantly alter the luminal diameter, but definitely alters the edge of the plate.
Atherosclerosis is considered the leading cause of morbidity and mortality in most countries worldwide. It is a multifactorial disease, and its basis today in the identification of a chronic inflammatory process, which may cause clinical events due to rupture of the atherosclerotic plaque [5]. Dyslipidemia has been pointed out by some authors as the main risk factor for atherosclerotic disease, particularly coronary artery disease. Thus, the elevation of Low Density Lipoprotein Cholesterol (LDL-c) and triglycerides, and the reduction of High Density Lipoprotein Cholesterol (HDL-c), have been identified as independent risk factors.
Lipids of Clinical Importance
Among the lipids of clinical importance one can mention fatty acids, triglycerides, phospholipids and cholesterol. Fatty acids enter the Krebs cycle to generate energy, participate in the synthesis of prostaglandins and provide acetylCoA for the synthesis of other lipids. Triglycerides are obtained by diet or produced by the body from the esterification of glycerol with three molecules of fatty acids for energy use or subsequent storage. Phospholipids have a glycerol molecule, in which two fatty acids are esterified; cell membranes and are part of the surface of lipoprotein particles. Cholesterol is man’s main steroid. It can present in the free form (structural component of the cell membrane and surface of lipoprotein); esterified (inside cells and lipoproteins, and esterification takes place in plasma) and inside the cell (by the Enzyme ACAT). Cholesterol also serves as a precursor for the synthesis of steroid hormones, vitamin D and bile acids [4].
Lipoproteins
Lipoproteins are macromolecules consisting of a lipid fraction (free and esterified cholesterol, triglycerides and phospholipids), and another protein fraction (apolipoproteins). The function of lipoproteins is to transport the lipids obtained by endogenous and exogenous route to the tissues. The largest classes of lipoproteins are chylomicron, Intermediate Density Lipoprotein (IDL), Very Low Density Lipoprotein (VLDL), LDL and HDL. Chylomicron is a large particle produced by the intestine containing 90% of the triglycerides of the diet (exogenous), relatively low in cholesterol and phospholipid, and with 1% to 2% protein. VLDL has very low density, lower than chylomicron. It is also rich in triglycerides (in excess, causes turbidity in plasma). Triglyceride is of endogenous origin, mainly hepatic (about 50% of the particle). LDL constitutes 50% of plasma lipoproteins. They’re small. Cholesterol is esterified and makes up 50% of the particle. The protein fraction is 25% of LDL. HDL has high density and is composed of 50% protein, 20% cholesterol (mainly esterified), 30% phospholipids and triglyceride traces. She’s in charge of reverse cholesterol transport. IDL has intermediate lipid content between VLDL and LDL. Lipoprotein(a) [LP(a)] has lipid composition similar to that of LDL and results from the covalent association by disulfide bridges between apo B-100, of the LDL particle, and a high molecular weight protein, apo(a), which presents structural homology with plasminogen. This union occurs in the outer membrane of the hepatocyte or in plasma, by a mechanism not yet demonstrated. The Lp(a) particle is not removed by hepatic LDL receptors. The physiological function of Lp(a) is not known, but it has been associated with the formation and progression of atherosclerotic plaque. Its concentration in human serum is genetically determined and suffers little influence from diet, drugs or lifestyle.
Relating Lipids and Atherosclerosis
Atherogenic lipoproteins are LDL, VLDL and remnants of chylomicrons, LP(a). Anti-atherogenic lipoproteins are, above all, HDL.
Apolipoproteins
Apolipoproteins are proteins that are part of the structure of lipoproteins and have functions in lipoprotein metabolism in specific receptor binding and in the activation or inhibition of certain enzymes involved in lipid metabolism. They contribute to the solubilization and stabilization of lipids and contribute to the interaction with phospholipids in lipoproteins.
Endothelial vascular effects
The physical and functional integrity of the endothelium is
fundamental. Once established that the process of atherosclerosis
is seen as an inflammatory process of the arterial wall, the
pathophysiological changes that occur in the endothelium are:
a. Altered vasomotricity;
b. Loss of anti-inflammatory effect of the vessel;
c. Loss of antithrombotic effect of the vessel;
d. Cell uptake and migration (monocytes, macrophages and
platelets).
The above, associated with dyslipidemia, systemic arterial hypertension, diabetes and smoking, contribute to the appearance of important clinical events, mainly related to coronary artery disease, cerebrovascular disease and peripheral arterial disease.
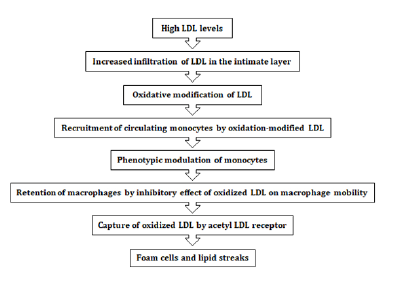
Schematically, we will have: figure 1 Thus, what makes LDL-c a pro-inflammatory agent are the changes that the particle undergoes such as glycation and oxidation. Thus, it is the modified LDL particle that is pro-inflammatory and atherogenic. The liver plays an important role in removing LDL from plasma (75%), and receptormediated (75%) and receptor-independent (25%) withdrawal has been performed. There is also 25% uptake by extrahepatic tissue. Thus, receptor deficiency results in increased cholesterol levels.
Figure 1:
Stages of arteriosclerotic injury
In phases I and II, elevated plasma LDL levels may increase availability in the intima. This LDL, free or bound to the matrix,can be oxidized. Oxidized LDL recruits monocytes. Monocytes differ in macrophages. Then oxidized macrophages and LDL interact forming the foamy cell. Oxidized LDL and the components released by macrophages of foamy cells damage the endothelium. With progression, fatty streak marks appear. There is still the proliferation and migration of smooth muscle cells. In phase III, there is the appearance of extracellular lipids and rupture of macrophages. The lesion of this stage will be a mixture of remnants of foamy cells routes of lipid content, scattered between the layers of smooth muscle cells. In phase IV, the extracellular lipids become coalescent (the lipid core of the plaque) and there is a formation of juxtaposed smooth muscle cells. There are, still, between the lipid nucleus and the endothelial surface, macrophages, mast cells and lymphocytes. In phase V there is fibrous connective tissue, associated with the lipid nucleus (fibroatheroma) [4,6]. In phase VI, a complicated lesion occurs due to plaque rupture and thrombosis.
HDL-c - Reverse cholesterol transport
HDL-c is secreted by the liver and intestine in the form of a discoded particle. A classification system divides HDL into: a) larger and richer lipid sums (HDL-2) and b) the smaller and denser (HDL-3) are the largest and most dense (HDL-3) [7]. The small particles promote the outflow of excess non-esterified cholesterol from peripheral cells, making them esterified through the enzyme Lecithin Cholesterol Acyl Transferase (LCAT). Excess cholesterol is removed to the liver from peripheral tissues. In its nascent discoid form, HDL, under the continuous action of LCAT, develops a cholesterol esther core, transforming the disc into a mature particle (HDL-3). This, in turn, continues to acquire phospholipids and cholesterol of chylomicron and VLDL, being converted into HDL-2, larger and richer in cholesterol than its predecessors.
Thus, the reverse transport of cholesterol from tissues to the liver by means of HDL particles occurs by their hepatic capture, through specific receptors or, indirectly, through the content of cholesterol esters by other lipoproteins also subsequently captured by the liver. Once they reach the liver, they are reused in other metabolic pathways, producing bile acids or being excreted by bile. HDL is very frequently associated longevity by promoting the flow of cholesterol; antioxidant properties; anti-inflammatory properties; antithrombotic properties and anti-apoptotic properties. The protective effect of HDL on coronary artery disease and transient ischemic stroke suggests that, in addition to LDL-c, HDL-c would be a marker for therapeutic interventions, such as increased physical activity to enhance longevity [7].
Considerations related to the heart of the elderly
Like any other part of the body, the cardiovascular system changes with aging. The “normal” heart of the elderly has relatively small ventricular cavities, atria and relatively large arteries. The coronary arteries increase in length and width, logically related to the decrease of the ventricles, which results in the tortuosity of the ventricle. Subepicardial adipose tissue increases with age. Valve leaflets thicken with age, particularly A-V valves. Histological examination is of great importance because it shows the amount of pigment (lipofuccin) in myocardial cells. These changes are present in all population groups, independent of their geographical location and the sea level of lipids. A high systemic blood pressure accelerates and amplifies these “normal” changes, which appear in the cardiovascular system with the evolution of age. The pulmonary arteries and aorta widen and streak with aging. Hence they tend to become tortuous [8]. Increases the thickness of the septum and not of the free wall of the left ventricle; increases the circumference of all heart valves and usually the circumference of the aortic valve is higher than that of the pulmonary valve.
Changes in lipid metabolism [9] that occur with aging are linked
to the following factors:
a. Decreased lipoprotein lipase activity with attenuation of
lipopolitical activity, with consequent slowing of the clearance
of the remaining chylomicrons and VLDL.
b. Decreased intestinal absorption of cholesterol.
c. Increased LDL-c and decreased catabolism speed.
d. Decreased LDL receptor expression.
e. Changes in HDL size and reduced liver lipase activity.
After the age of 70
a. Lower absorption of dietary cholesterol
b. Decrease in bile acids
c. Decreased synthesis of fecal steroids
d. Delayed Cholesterol Turnover
e. Decreased cholesterol synthesis
In the very elderly
Lower cholesterol and LDL-c levels resulting from decreased cholesterol absorption.
Recent molecular biology and genetic studies are demonstrating many more intricate details and metabolic correlations. There is a huge universe of scientific information with hypothesis linking each one of the steps described [10].
References
- Jebari-Benslaiman S, Galicia-García U, Larrea-Sebal A, Olaetxea JR, Alloza I, et al (2022) Pathophysiology of atherosclerosis. Int J Mol Sci 23(6): 3346.
- Malekmohammad K, Bezsonov EE, Rafieian-Kopaei M (2021) Role of lipid accumulation and inflammation in atherosclerosis: Focus on molecular and cellular mechanisms. Front Cardiovasc Med 8: 707529.
- Herrero-Fernandez B, Gomez-Bris R, Somovilla-Crespo B, Gonzalez-Granado JM (2019) Immunobiology of atherosclerosis: A complex net of interactions. Int J Mol Sci 20(21): 5293.
- Sinha AK, Singh BM, Mehta JL (2004) Statins and inhibition of atherosclerosis: Human studies. In: Mehta JL (Ed.), Statins: Understanding Clinical Use. Saunders Publishers, Pennsylvania, USA, pp.37-49.
- Carbonin P, Zuccalà G, Marzetti E, Lo Monaco MR (2003) Coronary risk factors in the elderly: Their interactions and treatment. Curr Pharm Des 9(29): 2465-2478.
- Barter P (2004) HDL: A recipe for longevity. Atheroscler Suppl 5(2): 25-31.
- Kencis L (2001) Dyslipidemia in the elderly. From theory to practice. In: Lopes AC & Martinez TLR (Eds.), Dyslipidemias: from Theory to Practice, Atheneu, São Paulo, Brazil, pp.135-152.
- Shirani J, Yousefi J, Roberts WC (1995) Major cardiac findings at necropsy in 366 American octogenarians. Am J Cardiol 75(2): 151-156.
- Diament J, Forti N, Maranhão RC (2005) Dyslipidemias in the elderly. In: Wajngarten M (Ed.), Cardiogeriatria. Roca, São Paulo, Brazil, pp. 158-173.
- Ginsberg HN, Packard CJ, Chapman MJ, Borén J, Aguilar-Salinas CA, et al. (2021) Triglyceride-rich lipoproteins and their remnants: Metabolic insights, role in atherosclerotic cardiovascular disease, and emerging therapeutic strategies-a consensus statement from the European Atherosclerosis Society. Eur Heart J 42(47): 4791-4806.
© 2022 Martinez TL. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






