- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Transcatheter Intervention in Neonates and Young Infants with Congenital Heart Disease: Analysis of Cases in a Tertiary Care Hospital of Bangladesh
Nurun NF*
Congenital and Structural Interventionist, Combined Military Hospital, Bangladesh
*Corresponding author: Nurun Nahar Fatema, Congenital and Structural Interventionist, Combined Military Hospital, Bangladesh
Submission: January 10, 2022;Published: March 09, 2022

ISSN 2578-0204Volume3 Issue4
Abstract
Background: Percutaneous catheterization for diagnostic and therapeutic purpose has been used since long for management of neonates and young infant with Congenital Heart Disease (CHD). In Bangladesh these activities are being carried out routinely since 1998. Aim of this study is to analyze the pattern of diseases, intervention and outcome of cases who had catheterization and intervention.
Methods: This is a retrospective study carried out in a tertiary level hospital from Jan 2015 to Jan 2020. Demographics, clinical presentation, diagnostic and procedural parameters were recorded from computerized medical records of various departments of pediatric cardiology.
Result: Total 883 cases were analyzed. Most of the cases were in > 6-month-18 month age group. Male were 444(50.28%) and female were 439 (49.72%) Most of the cases (43.60%) reported with pneumonia and dyspnea and later identified as congenital heart disease. Isolated patent ductus arteriosus (41.33%) was the commonest CHD in the study population. Six hundred ninety-eight (79.05%) cases had transcatheter interventions and 185 (20.95%) cases had cardiac catheterization. Seventy-six (8.60%) cases were neonates. Median Gestational age was 34 weeks for neonates. Most common procedure in neonate was Balloon Atrial Septostomy (BAS) (23.68%) and in infant was device closure (46.38%) of Patent Ductus Arteriosus (PDA). Over all median procedure time was 25min. Overall success rate was 97.27%. Two patient of PDA stenting died from pulmonary oedema. Two patient of PDA device closure died at home after discharge from milk aspiration.
Conclusion: Most of the procedure in neonate and infant was performed as life saving measure. Many procedures were performed for the reason that immediate surgery was not available in our set up. Outcome of the procedures were good.
Keywords: Transcatheter intervention; Congenital heart disease; Newborn; Cardiac Catheterization 3.
Abbreviations: TGA: Transposition of Great Arteries; PA: Pulmonary Atresia; CoA: Coarctation of Aorta; PS: Pulmonary Stenosis; AS: Aortic Stenosis; LPA: Left Pulmonary Artery; RPA: Right Pulmonary Artery; BAS: Balloon Atrial Septostomy; BVP: Balloon Valvuloplasty; GW: Gestational Week
Introduction
Severe form of Congenital Heart Disease (CHD) necessitate early treatment in infancy even in neonatal period. Incidence of severe CHD is 2.5-3 per 1000 live birth [1]. About 25% of death in neonatal period contributed by birth defects or malformation is severe form of CHD [2,3]. Infants with life threatening CHD may be asymptomatic initially or signs may be obscured [4]. These kind of patient can maintain life with fetal circulation. With birth a tremendous change takes place and post-natal circulation no longer require some fetal structures like Patent Foramen Ovale (PFO), Ductus Arteriosus (DA), ductus venosus. Neonates with CHD dependent on Patent Ductus Arteriosus (PDA) flow to maintain pulmonary or systemic circulation or with mixing physiology like Transposition of Great Arteries (TGA) to accentuate left atrial venous return are at great risk to survive with change [5,6]. Immediate initiation of prostaglandin save life until palliative or curative interventions are available [7]. Early prenatal or postnatal diagnosis, timely intervention or surgery can save life and lacking of facility lead to morbidity like brain damage, multi organ failure even death [8]. Recent advance in interventional field and intensive care showed hope for these cases. Complete cure are possible in many disease like critical Pulmonary Stenosis (PS), Coarctation of Aorta (CoA), Aortic Stenosis (AS), PDA, Some Atrial Septal Defect (ASD secundum) and some Ventricular Septal Defect (VSD) cases. With time percutaneous intervention in neonates and children reached higher success rate with lower morbidity compared to surgery in newborn or young infant [9]. This study was intended to analyze the outcome of neonates and young infant with CHD who had undergone various types of intervention.
Materials and Methods
This retrospective study was carried out in two tertiary care hospitals of Bangladesh from January 2015 to January 2020. All patient up to 18 months of age and had undergone cardiac catheterization or transcatheter intervention were included in the study. Pericardiocentesis and temporary pacing was excluded. Informed written consent from the parents or guardian was taken. The study was approved by the ethical committee of the above hospital (Lab Aid Cardiac hospital)
Data collection
Demographic data, diagnosis, clinical data, echocardiography and angiography reports, transcatheter intervention, complications, outcome, duration of hospital stay were analyzed. In ductus dependent circulations, prostaglandin infusion was started. But infusion was stopped two hours before procedure. Infusion pump was standby to restore if patients’ saturation dropped.
Sedation
Whole procedure was performed under deep sedation or general anesthesia for intubated patients. To avoid respiratory depression, cocktail or combination of minimum doses of two to three drugs were used. Injection Ketamine, Injection Midazolum and Injection Phenobarbitone were used in most of the cases. General anesthesia was used in eight intubated neonates.
Procedure
Only arterial access line was used for PDA stenting in pulmonary atresia and intact ventricular septum type of cases. In emergency Balloon Atrial Septostomy (BAS) cases, only venous access was used. For Neonatal Coarctation of Aorta (CoA), only arterial access line was used. For rest cases both arterial and venous access was used unless otherwise failed. Angiography was performed in specific site and haemodynamic data recorded. Interventions were performed following standard steps under Echocardiography and fluoroscopic guidance. Procedure time, fluoroscopy time and complications encountered were noted. Heparin infusion was continued for 48 hours after procedure in PDA stenting, Right Ventricular Outflow Tract (RVOT) stenting cases. Later Aspirin was initiated at 3-5mg/kg/day dose. For ASD and VSD device closure, two more doses of heparin at 50ml/kg doses were given after 4 and 8 hours of the procedure. Aspirin was started at 5mg/kg/day single dose for 06 months. For Coarctation balloon dilatation, one more dose of heparin, 50mg/kg was given after 4 hours and aspirin was advised for 03 months. All patient other than PDA stenting & RVOT stenting were discharged after 24 hours. All stenting cases and intubated cases were discharged once they settled. Follow up at 1,3,6,9,12,18,24 month were advised with ECG, CXR and Echocardiography.
Statistical analysis
All statistical analysis were performed in MS-Excel spread sheet. Quantitative variable are shown as median and range and categorical variables as number and percentage. As it was a single variant study, no comparative testing were performed.
Results
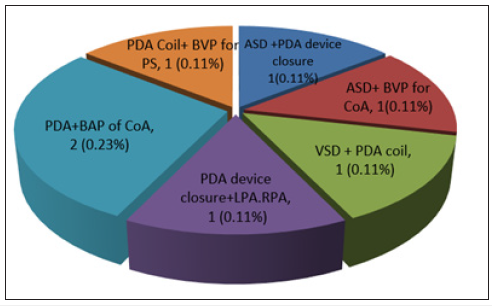
Table 1 Out of 883 cases enrolled, 90 (10.19%) were in 0-02 months age group, 162 (18.34) were in 2-6 month age group and 631 (71.46%) were in more than 06 month age group. Body weight of 92 (10.42%) cases were less than 03kg, 43.60% cases were in between 3-6kg and 45.98% cases were more than 06kg. About 45.98% cases were full term at birth. Figure 1 showed Pattern of presentation in study population. Dyspnea and pneumonia (43.60%) was the commonest presentation followed by failure to thrive (28. 77%) and cyanosis in 6.34%. Table 2 showed pattern of disease. Isolated PDA was the commonest disease (41.33%) followed by Isolated ASD (8.38%) PS (6.34%), Coarctation of aorta (5.21%), ASD & PS (5.78%), VSD 5.66%, TOF 3.92% etc. Table 3 Showed separate analysis of neonates in study population. Nineteen (25%) cases were in less than 07 days age group, 10 (13.16%) were in 7-14 days group and 47 (61.94%) cases were in more than 14 days age group. Age pattern indicates delay in diagnosis in neonatal critical cases. Most of the cases were preterm and in 32-37 gestational weeks (61.84%) (GW). Male were more (64.47%), Weight of most of the cases were between 2.5-3.5kg (46.05%). TGA, pulmonary atresia and coarctation of aorta were the commonest CHDs (23.68%, 23.88%, 22.37%). BAS was the commonest procedure (23.68%) followed by PDA stenting and coarctoplasty (21.05%), Among complications, pulse loss was highest (7.88%). Two cases of PDA stenting died from pulmonary oedema (2.63%). Figure 2 showed distribution of cases in catheterization laboratory. Transcatheter interventions were performed in 698 (79.05%) cases and diagnostic catheterization in 185(20.95%) cases. Table 4 showed pattern of interventions and outcome of the cases. PDA device closure was commonest (50.14%) followed by BVP PS (9.51%), ASD device closure (9.46%), COA balloon angioplasty 5.21%, PDA Coil occlusion 6.25% etc. Two PDA devices were embolized and were referred to surgeon. One PDA stent was embolized but repositioned and 2nd stent implanted. Arrhythmia was noticed in two ASD, one Balloon valvuloplasty of Aortic & Pulmonary valve and one PDA stenting cases. Air embolism was noticed in one ASD device case. Pulmonary oedema was noticed in two PDA stenting cases and they expired later. PDA stenting cases had maximum five various types of complications including death. At one year follow up two PDA device closure cases had mechanical obstruction at aortic end and balloon coarctoplasty was performed. Two PS and one CoA cases had restenosis and treated with balloon dilatation again Figure 3. showed cases who had double intervention. PDA device closure and balloon coarctoplasty was performed in 0.23% cases and rest had combinations of ASD+PS, ASD+PDA, VSD+PDA, PDA+LPA, RPA and cured with device closure and balloon angioplasty and valvuloplasty.
Table 1:Age and sex distribution of patients (N=883).
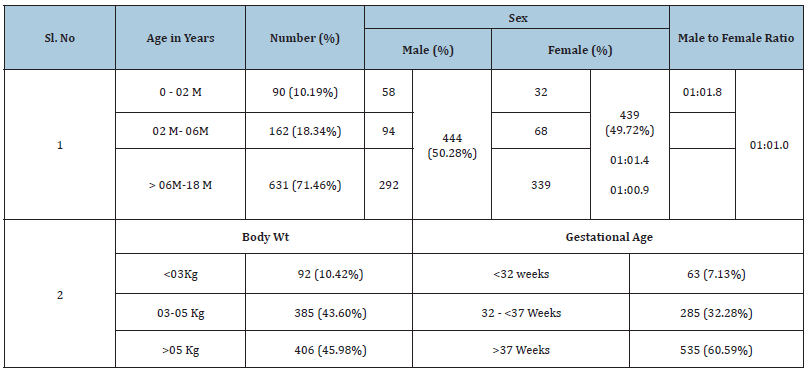
Table 2:Pattern of diseases among study population. N= 883
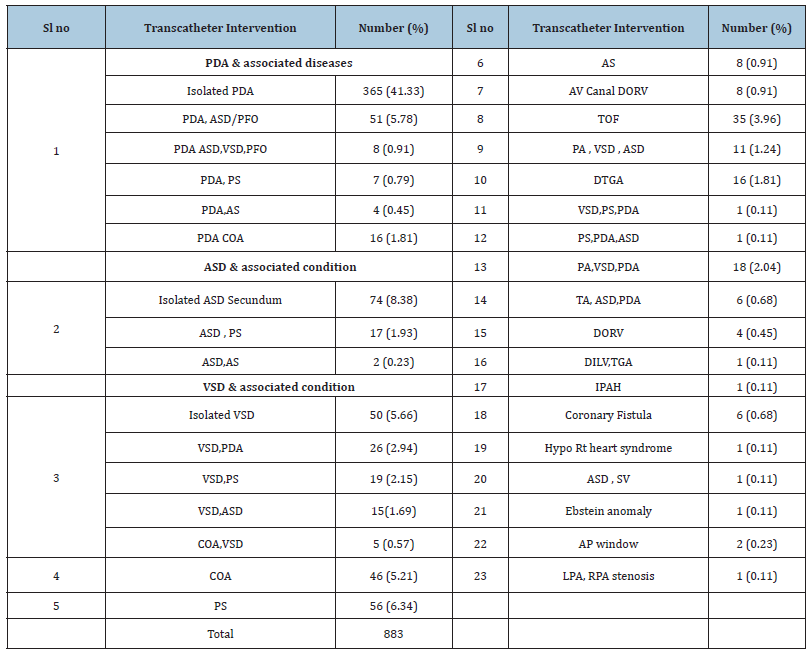
Table 3:Analysis of neonates undergone transcatheter intervention and associated condition N= 76
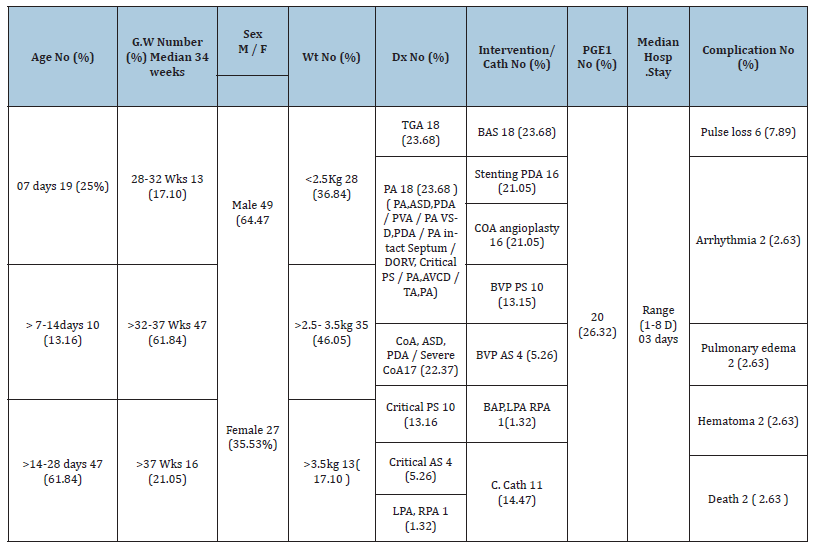
Table 4: Complications and outcome of various transcatheter interventions N-698.
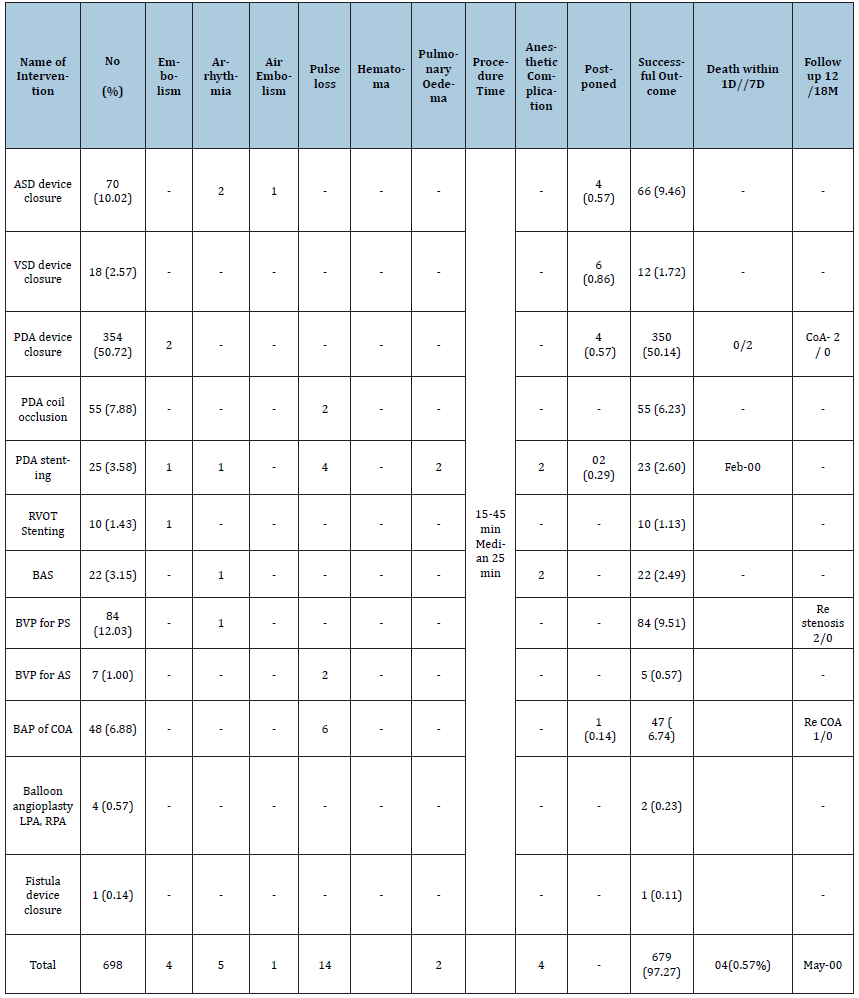
Figure 1:Pattern of clinical presentation N-883.
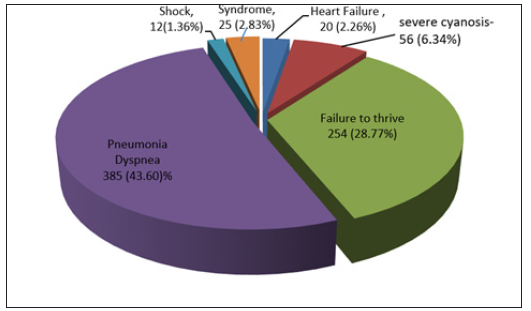
Figure 2:Distribution of cases in catheterization laboratory N=883.
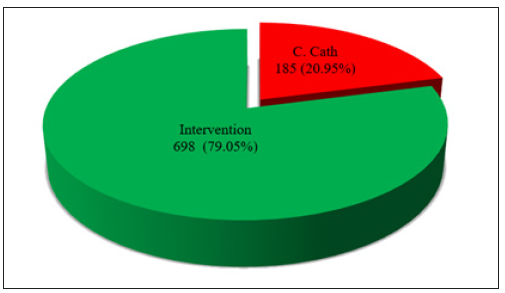
Figure 3:Double Intervention in single setting in study cases N =7.
Discussion
CHD can be classified into three main categories on clinical
consideration:
A. Life threatening CHD where patient may die without early
treatment.
B. Clinically significant CHD where death is unlikely but timely
intervention is mandatory.
C. Clinically non-significant CHD which are anatomical defects of
heart without much clinical significance [10].
Life threatening CHD usually manifest in neonatal period or in
early infancy [11] Neonates or infants with life threatening heart
defects may not have symptoms initially as they continue to depend
on fetal structures like foramen oval or ductus arteriosus as long
as they remain patent. Those neonates/infants are at great risk
of collapse once ductus dependent pulmonary or systemic flow
stops or mixing through PFO stops in diseases like Transposition
of Great Arteries (TGA) [5,6]. In this retrospective study, out of
883 (100%) cases, only 76 (8.60%) patient were newborn which
can reflect the scenario of medical care system in a developing
country. Fetal diagnosis was established in 8 cases only which is the
standard of care in first world country. Ignorance about CHD among
care receivers and care givers, poverty, and lack of facility at grass
root levels lead to delay in seeking help and referral to advance
center. Many newborn die at home before reporting to health care
providers. Male sex outnumbered female in this study 444(50.85%)
which is similar to other study [5]. In majority of the cases parent
or other household identified cyanosis, respiratory distress.
Feeding difficulties or failure to gain weight and sorted medical
advice. Some cases were referred from pediatrician as pneumonia
for cardiac evaluation. Turners syndrome, Down syndrome,
congenital rubella syndrome, Noonan,s syndrome were the
reason for referral in some cases (Figure 1). Most common clinical
manifestation in study cohort was dyspnea (43.60%). Commonest
cause of respiratory distress in absence of lung disease is a large
left to right shunt which also cause tachypnea, dyspnea, feeding
difficulty, lack of weight gain etc. [4]. Cyanosis or decreased oxygen
saturation after excluding respiratory cause is due to cyanotic
CHD where there is mixing of blood and or decreased pulmonary
blood flow. Hyperoxia test was used to differentiate cardiac cause
in neonates like other study [1,7]. Neonates were admitted to
NICU immediately and those with PDA dependent circulation
were started with injection prostaglandin infusion. Gestational age
of most of them were >32 weeks with median 34 weeks. (Table
3) Most of the neonate in this study were candidate for surgery
but low birth weight, complexity of the situation, poor general
condition, comorbidity was the contraindication like other studies
[11]. Moreover, immediate surgical facility was not available in our
set up. As a result, lifesaving and curative transcatheter treatment
were preferred. Recently there has been a significant improvement
in interventional management with availability of smaller size hard
ware and recruitment of more and more lesions in the list. There has been tremendous improvement in pre intervention and post
intervention critical care management [12]. So survival of newborn/
infant is possible until they reach surgery. Some intervention like
balloon coarctoplasty in neonate and infants were performed as
surgical facility was not available. Later complete cure without any
complications in all the cases encouraged the center to take it as
first choice therapy [13,14]. In our set up and background we were
depending on catheter based therapies for multiple reasons:
A. Skilled team is available to manage cases
B. Less expensive
C. Less hospital stay
D. Easy chance of repeatability
E. Good outcome
F. Lack of availability of surgical team for neonates & young
infants. These are prevailed in many other places also [15]
Like Coarctation of Aorta (COA), closure of large tubular PDA in all infants and newborn were performed percutaneously as these cases were refused by all available center initially for surgical ligation. Excellent outcome of the cases led the centre to take it as first choice therapy [16,17]. In this retrospective study, common interventions performed in neonates were Balloon Atrial Septostomy (BAS), Balloon Coarctoplasty, Stenting of ductus arteriosus, Balloon pulmonary and aortic valvuloplasty, peroration of pulmonary valve with wire etc. Among these, coarctoplasty and balloon valvuloplasty were curative interventions (Table 3). BAS and PDA stenting cases were referred to cardiac surgeon later on for specific surgical correction. In this study critical pulmonary valve stenosis mimicking functional pulmonary atresia had excellent outcome after balloon valvuloplasty. In membranous pulmonary atresia cases, pulmonary valve was pierced by stiff wire and later balloon valvuloplasty was performed with PTCA balloon and Tyshak mini balloon. Gradient across pulmonary valve reduced to less than 40mm Hg in all cases. This finding correlates with other study [1,18]. Outcome of PDA stenting was reasonable. Out of 25(3.58%) cases, two neonates died (0.22%) from pulmonary oedema due to increased blood flow to pulmonary circulation. Out of sixteen neonates, twelve were getting injection prostaglandin for stabilization prior to stenting. In Coarctation of aorta, PDA stenting and Balloon aortic valvuloplasty cases, transient pulse loss was experienced but returned to normal after heparin infusion. Commonest intervention in this cohort was PDA device closure. One of the challenging intervention was device closure of large tubular PDA’s with severe pulmonary hypertension. Initially conventional devices (ADO) were used and special technique applied to pull the rounded aortic end inside ductus and pressing against PDA wall. Later double disc devices (VSD muscular device (Lifetech scientific), ADO II (Abbott Vascular, USA), Multifunctional functional occlude (MFO) (Lifetech, Schenzen)) were used. Outcome was excellent and pulmonary pressure reduced in all cases within 48 hours except two. Two cases developed coarctation of aorta later from mechanical pressure effect of aortic end. Balloon dilatation of these two cases were performed later with good result. Two young infant (4 month, 6 month) died from aspiration of milk after discharge. ASD device closure was performed in 66(9,49%) cases of infants as their ASD was increasing in size in subsequent follow up. All had excellent result without any complication up to first eighteen months follow up. VSD device closure was performed in 12(1.72%) out of 18 (2.57%) cases tried. Most of them were muscular VSD who had several pulmonary hypertension with reverse shunt. Multifunctional occluder (MFO) were used and VSD were closed from retrograde approach. Outcome was excellent till last follow up. RVOT stenting was a palliation for TOF, or DORV (TOF like cases) who had cyanotic spell but body weight was inappropriate for surgical correction. Few cases (three) could not arrange cost of surgery, so RVOT stenting was preferred to improve quality of life. All were planned for total correction except one for bidirectional Glenn shunt. Some of the cases had double intervention (Figure 3) in single setting for multiple lesion and outcome was good. Combined intervention of PDA device closure and Balloon coarctoplasty was commonest type (0.23%).
Interventional procedure in young infant and neonates are always a high risk procedure with chances of complications. In this study mortality was (0.56%) and other complication were minimal (34/698). One study reported 13 complication in 46 cases and another reported 03 complication in 20 cases [19]. Most of the cases in this cohort had no antenatal diagnosis and they were referred from Neonatal Intensive Care Unit (NICU) or Pediatric Intensive Care Unit (PICU) or reported to emergency department of pediatrics or pediatric cardiology when emergency arose. Only 8 cases had planned admission with antenatal diagnosis. Most of the procedures were performed after a short time of initial stabilization in intensive care unit. As interventions were life-saving in neonates and timing was important, so complications were more in these cohort group. Pulse loss was the commonest complications but managed efficiently. Respiratory arrest from sedatives used were one of the common anesthetic complications encountered. With gaining experience of dealing such cases, complication rate decreases significantly in later part of study.
Conclusion
Low body weight is a major risk factor both for surgery and transcatheter intervention, yet these group of patient demand urgent treatment for life- saving purpose. Catheter based therapy proved better considering mortality and morbidity and availability of resource and infrastructure. Surgical facility in low and lowmiddle income country is still limited and achieving certain body weight to meet criteria for surgery in some center is even difficult. Life- saving palliative intervention is a bridge to surgery for these kind of cases and curative interventions offer these children a normal life.
References
- Asli Nuriye M, Osman Baspinar (2019) Transcatheter cardiac intervention in neonates with congenital heart disease : A single centre experience. Journal of International Medical Research 47(2): 615-625.
- Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39(12): 1890-1900.
- Lawn JE, Cousens S, Zupan J, Lancet Neonatal Survival Steering Team (2005) 4 million neonatal deaths: When? where? why? Lancet 365(9462): 891-900.
- Chang RK, Gurvitz M, Rodriguez S (2008) Missed diagnosis of critical congenital heart disease. Arch Pediatr Adolesc Med 162(10): 969-974.
- Yee L (2007) Cardiac emergencies in the first year of life. Emerg Med Clin North Am 25(4): 981-1008.
- Friedman AH, Fahey JT (1993) The transition from fetal to neonatal circulation: Normal responses and implications for infants with heart disease. Semin Perinatol 17(2):106-121.
- Mellander M (2013) Diagnosis and management of life-threating cardiac malformations in the newborn. Semin Fetal Neonatal Med 18(5): 302-310.
- Colaco SM, Karande T, Bobhate PR, Rashmi Jiyani, Suresh G, et al. (2017) Neonates with critical congenital heart defects: Impact of fetal diagnosis on immediate and short-term outcomes. Ann Pediatr Cardiol 10(2): 126-130.
- Dancea A, Justino H, Martucci G (2013) Catheter intervention for congenital heart disease at risk of circulatory failure. Can J Cardiol 29(7): 786-795.
- Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, et al. (2005) Newborn screening for congenital heart defects: A systematic review and cost effectiveness analysis. Health Technol Assess 9(44):1-152.
- Sin Weon Yun (2011) Congenital heart disease in the newborn requiring early intervention. Korean J Pediatr 54(5):183-191.
- Celebi A, Yucel IK, Bulut MO, Mehmet Kucuk, Sevket Balli (2017) Stenting of the ductus arteriosus in infants with functionally univentricular heart disease and ductal-dependent pulmonary blood flow: A single-center experience. Catheter Cardiovasc Interv 89(4): 699-708.
- Fatema NN (2017) Transcatheter therapy for coarctation of aorta: Analysis of 150 cases. CVS Journal 10(1): 56-62.
- Fatema NN, Rahman SMM (2003) Balloon angioplasty in coarctation of abdominal aorta-A case report. JAFMC 11(2):95-98.
- Odemis E, Ozyilmaz I, Guzeltas A, Erek E, Haydin S, et al. (2013) Transcatheter management of neonates with pulmonary atresia with intact ventricular septum: A single center experience from Turkey. Artif Organs 37(1): E56-E61.
- Fatema NN, Razzaque AKM (2020) Device closure of large Patent Ductus Arteries (PDA) in young infants: Analysis of cases in Bangladeshi centre. Insights in Pediatric Cardiology 7(7): 1481-1487.
- Nadas AS, Fyler DC (2006) Hypoxemia. In: Keane JF, Lock JE, Fyler DC (Eds.), Nada’s pediatric cardiology. (2nd edn), Saunders Elsevier, Philadelphia, USA, pp. 97-101.
- Yucel IK, Bulut MO, Kucuk M, Sevket Balli, Ahmet Celebi, et al. (2016) Intervention in patients with critical pulmonary stenosis in the ductal stenting era. Pediatr Cardiol 37(6): 1037-1045.
- Karag€oz T, Akın A, Aykan HH, Çeliker A, Alehan D, et al. (2015) Interventional cardiac catheterization in infants weighing less than 2500g. Turk J Pediatr 57: 136-140.
© 2022 Nurun NF. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






