- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Unexpected Ventricular Tachycardia Induced by the Auto Capture Management Function of an Implantable Cardiac Device
Toshiko Nakai* Yukitoshi Ikeya, Rikitake Kogawa, Sayaka Kurokawa, Koichi Nagashima, Kimie Ohkubo and Yasuo Okumura
Department of Medicine, Division of Cardiology, Nihon University School of Medicine, Japan
*Corresponding author: Toshiko Nakai, Department of Medicine, Division of Cardiology, Nihon University School of Medicine, Japan
Submission: February 7, 2022;Published: February 21, 2022

ISSN 2578-0204Volume3 Issue4
Abstract
Auto Capture Management (ACM) is useful in preserving battery longevity and in ensuring pacing. However, ACM sometimes leads to ventricular pacing with unsafe timing. We experienced a case of 30-yearold male with an implantable cardioverter defibrillator in whom RV pacing was performed at unfavorable timing by ACM algorithm. We wish to emphasize the importance of looking at the electrocardiogram for the management of cardiac implantable electrical devices.
Keywords:Cardiac implantable device; Auto capture management; Under-sensing
Case Presentation
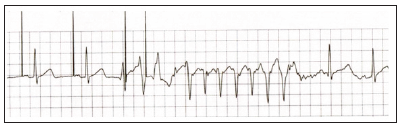
A 30-year-old male received an Implantable Cardioverter Defibrillator (ICD) after resuscitation from Ventricular Fibrillation (VF). The atrial lead (Tendril; Abbott, Chicago, IL, USA) was positioned in the right atrial appendage. The Right Ventricular (RV) lead (Duarte; Abbott) was positioned in the RV apex. Atrial sensing was 5.0mV, ventricular sensing was 12mV, atrial pacing threshold was 0.75V/0.4ms, and ventricular threshold was 0.5 V/0.4ms during implantation. The ICD was programmed in DDD mode with a lower rate of 60 Beats Per Minute (bpm) and an upper tracking rate of 130bpm. The paced Atrioventricular (AV) interval was 200ms and the sensed AV interval was 150ms. Regarding additional programming, Auto Capture Management (ACM) was turned on for future remote monitoring. After ICD implantation, the cardiac monitor detected Non-Sustained Ventricular Tachycardia (NSVT) (Figure 1).
Figure 1:Cardiac monitor tracing during event detection.
What Happened in this Patient and How Can this Problem be Resolved?
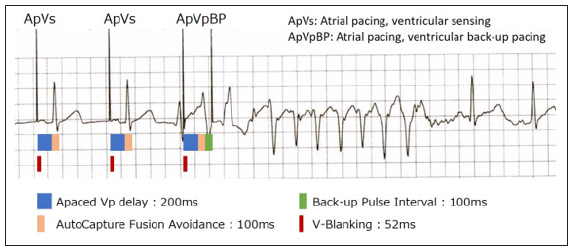
Figure 1 is a post-ICD implantation cardiac monitor recording during the hospital stay. Detailed annotations were added to the cardiac monitor tracing (Figure 2). NSVT was induced following RV pacing at undesirable timing. In this case, the RV ACM function was on. The timing of this RV pacing was not delivered at paced nor sensed AV intervals; this pacing was a backup pacing. ACM has a back-up pacing function where back-up ventricular pacing is performed with a 5-volt output if ventricular capture fails. If the timing of RV pacing results in fusion with an intrinsic R wave, the device cannot confirm capture or lack of capture, and back-up pacing continues even when the patient has a conducted beat. The device was not able to sense the first Premature Ventricular Contraction (PVC) and atrial pacing continued with uncaptured pacing. This was followed by back-up ventricular pacing with the fusion avoidance function, which occurred precisely on the T wave of the second PVC, resulting in NSVT. In this case, use of the ACM function led to an undesirable effect, with the potential for a life-threatening event. Thus, we disabled ACM in this patient.
Figure 2:Cardiac tracing with detailed annotations. Back-up ventricular pacing resulted in the induction of non-sustained ventricular tachycardia.
Discussion
Remote Monitoring (RM) is recommended in the management of cardiac electrical devices (Cardiac Implantable Electronic Devices, CIEDS), according to the statements of the Heart Rhythm Society/ American Heart Association/European Heart Rhythm Society and also the Japanese Heart Rhythm Society [1]. The benefits of remote monitoring have been shown in previous clinical studies [2-5]. When using RM, ACM is generally on (activated). ACM is useful in preserving battery longevity and in ensuring pacing. However, ACM sometimes leads to ventricular pacing with unsafe timing. There are also limitations to self-checks performed by CIEDS. Sensing failure cannot be detected by automatic device checks. The pacemaker cannot recognize whether sensing is detected correctly; for example, the detection may result from far-field sensing, or electromagnetic interference, or noise caused by lead fracture. Sometimes with DDD mode, under-sensing of atrial activity leads to mistimed ventricular pacing, and this can occasionally result in a spike on the T wave. All studies reported that remote monitoring significantly reduces the number of follow-up visits, time spent per visit by patients and physicians, increases patients’ follow-up adherence, and improves outcomes. However, we must be careful to confirm that the device is working correctly and safely, and does not put the patient at risk. We here wish to raise an alert concerning the use of remote monitoring to manage CIEDS without looking at the electrocardiogram. There many potentially concerning issues related to device operation, which may be minor, but may also be severe, and in any case need to be corrected. Careful consideration is needed with the use of remote monitoring and it is important not to place excessive trust in this modality.
Conclusion
ACM function is commonly used in RM management. However, we have to know a pit fall of this function like this case. Many minor issues may be encountered that, even if they are not immediately life-threating, have the potential to lead to serious future problems in these patients. Recently, due to COVID-19, RM has been strongly recommended in clinical practice for follow-up of CIEDS, and we wish to raise the concern that there might be excessive trust in RM. We again emphasize that the aim of RM is not to save clinic time, but to provide better quality in the management of CIEDS as an additional option to the in-person visit. It is important to see the electrocardiogram for the management of CIEDs.
Conflict of interest
T. Nakai belongs to a department established by contributions from Abbott Medical, Biotronik Japan, Medtronic Japan, Japan Lifeline, and Boston Scientific. T. Nakai received lecture fees from Abbott Medical and Medtronic Japan. All of the other authors have no conflicts of interest to report.
References
- Slotwiner D, Varma N, Akar JG, Annas G, Beardsall M, et al. (2015) HRS expert consensus statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm 2015: 12(7): e69-e100.
- Varma N, Epstein A, Irimpen A, Schweikert R, Shah J, et al. (2010) Efficacy and safety of automatic remote monitoring for implantable cardioverter-defibrillator follow-up: The lumos-T safely reduces routine office device follow-up (TRUST) trial. Circulation 122(4): 325-332.
- Crossley G, Boyle A, Vitense H, Chang Y, Mead RH (2011) The clinical evaluation of remote notification to reduce time to clinical decision (CONNECT) trial: The value of wireless remote monitoring with automatic clinician alerts. J Am Coll Cardiol 57(10): 1181-1189.
- Landolina M, Perego GB, Lunati M, Curnis A, Guenzati G, et al. (2012) Remote monitoring reduces healthcare use and improves quality of care in heart failure patients with implantable defibrillators: The evolution of management strategies of heart failure patients with implantable defibrillators (EVOLVE) study. Circulation 125(24): 2985-2992.
- Hindricks G, Taborsky M, Glikson M, Heinrich U, Schmachert B, et al. (2014) Implant-based multiparameter telemonitoring of patients with heart failure (INTIME): A randomised controlled trial. Lancet 384(9943): 583-590.
© 2022 Toshiko Nakai. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






