- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Clinical Prediction of Acute Heart Failure Patient for Hospital Admission form ED
Sricharoen P1, Yuksen C1*, Phinyo P2,3, Patumanond J2, Piyayotai D4, Sittichan buncha Y1, Likittanasombat K5, and Cheuathonghua E1
1Department of Emergency Medicine, Ramathibodi Hospital, Mahidol University, Thailand
2Department of Family Medicine, Chiang Mai University, Thailand
3Center for Clinical Epidemiology and Clinical Statistics, Chiang Mai University, Thailand
4Department of Medicine, Thammasat University, Thailand
5Department of Internal Medicine, Ramathibodi Hospital, Thailand
*Corresponding author: Yuksen C, Department of Emergency Medicine, Ramathibodi Hospital, Thailand
Submission: December 16, 2020;Published: December 22, 2020

ISSN 2578-0204Volume3 Issue3
Abstract
Introduction: Delay hospitalization in acute heart failure patients was the risk of complications, delay definite diagnosis, and treatment. This study aims to create a predictive score to predict hospitalization in acute heart failure patients.
Methods: Retrospective cohort design and collected data of acute heart failure patients in the emergency department. Predictive factors obtained from patients’ characteristics, underlying diseases, medical signs, vital signs on admission, a preliminary examination in the emergency department, and factors were stimulating acute heart failure in patients. Predictive factors were chosen from multivariable logistic regression and converted into predictive scores.
Result: 151 patients stayed in the hospital for more than 24 hours, and 62 patients stayed in the hospital for less than 24 hours. Predictive factors included NYHA (New York Heart Association) functional class, temperature, and patients’ breathing rate observed on admission, albumin levels, factors stimulating acute heart failure in patients caused by the acute coronary syndrome. Scores could predict more than 24 hours of hospital stay. AuROC was 85.27% (95% CI; 79.82, 90.73). Predictive scores were divided into 3 groups as the group with high scores (7.5-13.5), moderate scores (3.5-7), and low scores (0-3) being at risk of hospitalization longer than 1- day by 100%, 72.7% (95% CI;65.7, 79.8) and 16.7% (95% CI; 1.8, 31.6) respectively.
Conclusion: The scores can be used to predict hospitalization or ED length of stay for more than 24 hours for acutely decompensated heart failure patients in the emergency department.
Introduction
Acute heart failure is an important public health problem of the global population. In
the United States, nearly one million patients visit emergency departments every year, and
83.7% were admitted on averagely of 3.4 days [1], and the mortality rate about 4-5% [2]. In
Thailand, the hospitalization rate was averagely 7.5 days, and the mortality rate was about
5.4% [3]. One of the possible reasons was patient hospitalization assigned by the emergency
physician was more delayed; there was not enough bed for hospitalization, ending up in a
higher mortality rate [4].
The factors affecting the hospital stay was gender [5-7], age [8], diabetes [9,10], coronary
heart disease [9,11], chronic kidney failure [9,12,13], arrhythmia [14], patients with high
New York Heart Association (NYHA) functional class [15,16], patients with edema, patients
with low levels of hemoglobin, sodium, and albumin [10-13,15]. However, each study had
a difference in determining hospital stay from 4-7 days [5-15], and patients with delayed
hospital admission had a higher mortality rate [4].
Generally, the severity of decompensated heart failure ranges from patients experiencing
slight tiredness, shall have the preliminary treatment in the emergency department and
discharged. Patients shall admit to the hospital for further treatment in moderate symptoms
and severe symptoms requiring immediate treatment and admission in an intensive care unit [16]. In a mild and moderate acute heart failure symptom,
the patients need to be treated in the emergency department,
and clinical observation. The average length of stay in acute heart
failure patients was 29.76 hours. Delay in hospitalization was the
risk of complications, including emergency department crowding,
delay definite diagnosis and treatment [4].
In the Emergency department, Ramathibodi hospital, Mahidol
University, a university-affiliated super tertiary care hospital in
Bangkok, Thailand. There was overcrowding in ED and not enough
bed for admission of all mild and moderate heart failure. They had
to treat and observe in ED; if the clinical did not improve within 24
hours, the patients would be assigned to hospitalization. There was
no study to predict the heart failure patients to stay in the ED for
more than 24 hours and necessary to hospitalization. This study
aims to create a predictive score to predict hospitalization in acute
heart failure patients.
Methods
Study design and setting
This is retrospective cohort study included the acutely decompensated heart failure patients visiting the emergency department from January 2016 to December 2017 in Ramathibodi hospital; 62,991 patients receive services at the emergency department. The ethics committee approved the research methodology, data collection, and result interpretation. MURA2017/650/ID 09-60-40 and MTU-EC-ES-0-026/61. This research does not require a process of informed consent since it was a retrospective study of medical records.
Participant
We collected the data from electronic medical records (EMR). We included the participant who older than 18 years, visiting the emergency department from January 2016 to December 2017, diagnosed with acute decompensated heart failure, code I110, I130, I500, I509, and E877. We excluded the patient’s need for endotracheal intubation within the first 6 hours in ED because they seemed to have severe symptoms and were required hospitalization. We excluded the patients who transferred from other hospitals and refused treatment.
Definitions and procedures
Data were collected from retrospective medical records, and the
variable was obtained within the first 6 hours of patients arriving
at the ED. We include the decompensated heart failure according
to Framingham criteria [17] (either 2 major criteria or 1 major 2
minor criteria), and the pro-BNP value was more significant than
300pg/mL.
We collect all of the variables that may confound the
decompensated heart failure patients to stay in the ED for more
than 24 hours and necessary for hospitalization. All variables
included gender, age, underlying diseases (diabetes, coronary heart
disease, chronic kidney failure, arrhythmia), NYHA functional class,
edema, blood pressure, body temperature, heart rate, breathing
rate, levels of hemoglobin, sodium, albumin, and N-terminal probrain
natriuretic peptide (NT-proBNP), and chest x-ray results. We
used the complete-case analysis for the missing data.
We used the data from the pilot study to calculate the sample
size. A pilot study was conducted in 30 decompensated heart
patients who arrived at the emergency department, using inclusion
and exclusion criteria. We used STATA version 14, setting power of
80% and a significance level of 5% (two-sided). The ratio of sample
size was 1:1 found that the minimum sample size should be 150.
Data gathering
We recorded all of the variables and the outcome of a length of stay in the ED and divided the decompensated heart failure into two groups (more than 24 hours and less than 24 hours length of stay in the ED).
Statistical analysis
We used t-test and exact probability test to compare the
prediction factor. Each factor was predicted using univariable
logistic regression and showed an area under the receiver operating
characteristic (AuROC) curve and 95% confidence interval (95%
CI). Variables with high AuROC and significant p-value (<0.05)
were used as predictors and calculated using multivariable logistic
regression.
The obtained scores were considered to be predictive factors
of hospitalization for more than 24 hours using logistic regression.
The goodness of fit statistics (GOF) was tested using the Hosmer-
Lemeshow statistics. The predicted results from the scores were
compared with actual outcomes and illustrated by calibration plots.
The obtained scores were divided into three groups; high, medium,
and low. Prediction ability was shown as a chance that patients shall
stay in the hospital longer than 24 hours when patients being at a
particular group (positive predictive value), 95% confidence, and
a statistical significance level. The bootstrap method was used to
examine the equation’s inner parts to find its prediction efficiency
using the existing data to run a random test within 500 times. The
AuROC curve illustrated the efficiency of the internal examination.
Result
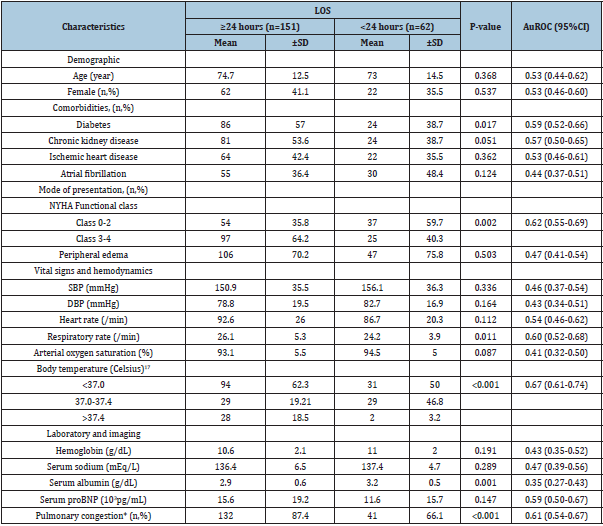
All 213 patients comprise 151 patients hospitalized more than 24 hours, and 62 patients hospitalized less than 24 hours. The findings showed that factors affecting hospitalization more than 24 hours were patients had diabetes (57% vs 38.7%, p=0.017), NYHA functional class 3-4 (64.2% vs 40.3%, p=0.002), patients had high breathing rate (26.1±5.3 vs 24.2±3.9, p = 0.011), body temperature was higher than 37.4 degree Celsius (18.5% vs 3.2%, p< 0.001), low albumin levels (2.9±0.6 vs 3.2±0.5 g/L, p=0.001), x-ray result showing pulmonary congestion (87.4 % vs 66.1%, p < 0.001) as shown in Table 1.
Table 1:Baseline clinical characteristics of study participants categorized by length of stay.
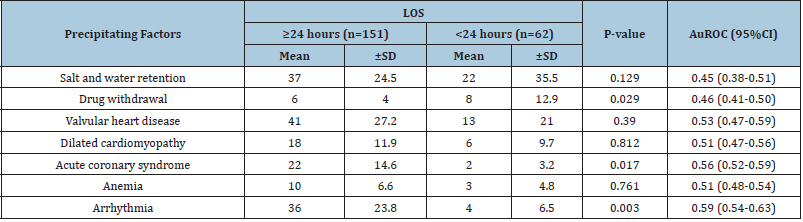
The precipitating factors of acute decompensated heart failure that affecting hospitalization more than 24 hours were arrhythmia (23.8% vs 6.5%, p=0.003), acute coronary syndrome (14.6 % vs 3.2 %, p = 0.017), and drug withdrawal (4 % vs 12.90 %, p=0.029) as shown in Table 2.
Table 2: Precipitating factors of acute decompensated heart failure.
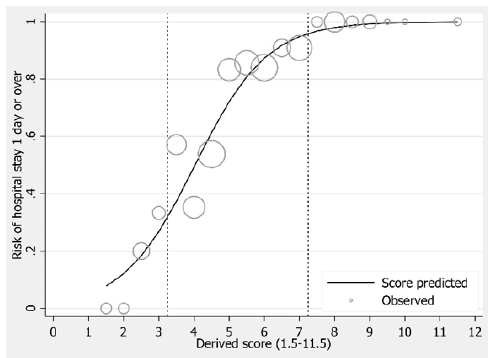
The best predictive factors to predict a chance of hospitalization more than 24 hours were NYHA functional class 3-4, breathing rate more than 24 per minute, body temperature, albumin level lower than 3.5 g/dL, chest x-ray result showing pulmonary congestion, stimulating factors from arrhythmia and acute coronary syndrome. The predictive factors were converted into scores using the logistic regression coefficient, as seen in Table 3. The predictive scores were combined with being the total scores of each patient. The total scores ranged from 0 to 13.5 points. The obtained total scores could predict a chance of hospitalization for more than 24 hours of patients, AuROC curve reached 85.27% (95% CI; 79.82, 90.73) (Figure 1), and the Hosmer-Lemeshow test was 0.8902.
Figure 1:Parametric ROC curve.
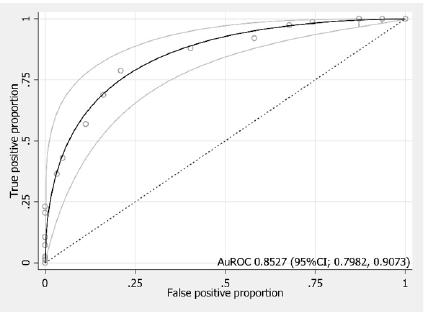
Table 3:Multivariable prognostic prediction model of prolonged ED stay.
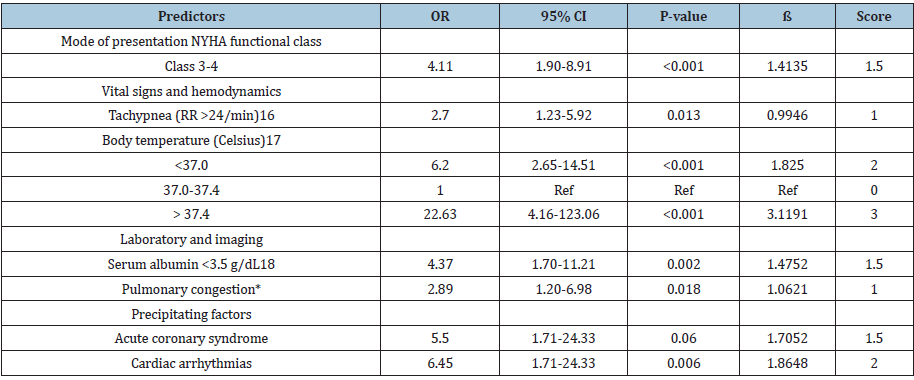
Table 4: Classification of risk groups.
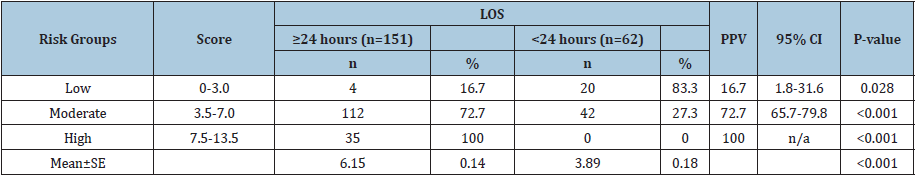
If scores were more significant, a higher chance of being hospitalized for more than 24 hours would become (Figure 2 & Figure 3). Based on Figure 2 & Figure 3, patients’ scores were divided into three groups. The group with scores of 0-3 points was a low chance of hospitalization. The group with scores of 3.5-7 points was a moderate chance of hospitalization, and the group with scores 7.5-13.5 points was a high chance of hospitalization. Positive predictive values were 16.7% (95% CI; 1.8, 31.6), 72.7% (95% CI; 65.7, 79.8) and 100% respectively (Table 4).
Figure 2:Internal calibration plots.
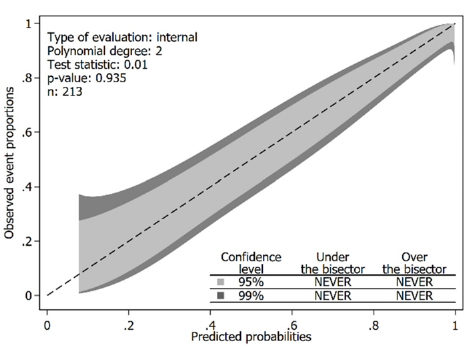
Figure 3:Internal calibration plots.
Discussion
This study aims to seek a predictive equation to predict
the acutely decompensated heart failure patients visiting the
emergency department, in the group without severe symptoms,
who have a chance to be hospitalized or ED length of stay more than
24 hours. The predictive equation consists of 7 variables: NYHA
functional class [3,4], breathing rate faster than 24 per minute,
body temperature less than 37 and higher than 37.4 degree Celsius,
albumin level lower than 3.5 g/dL, chest x-ray result showing
pulmonary congestion, precipitating factors from arrhythmia and
acute coronary syndrome. Patients with a score higher than 7 points shall be in the group of patients having a chance to be hospitalized or
ED length of stay for more than 24 hours. The emergency physician
should admit the high chance of hospitalization group as soon as
possible. If delay hospitalized, patients would delay treatment in
the emergency department, resulting in emergency department
crowding and complications in patients [18].
The study of Nam-Kyoo L et al. [19] in Korea was conducted
to evaluate the prediction factor to predict the 30 days revisit.
The prediction factor accordingly with our variable was NYHA
functional class, systolic blood pressure. In the previous studies,
variables were used to predict treatment outcomes from history
(NYHA function class), vital signs, laboratory results, and drug use
after patient discharge. In the NYHA functional class at level 3 and
above, the patients were the worst outcome [19-21].
The patients’ vital signs on admission were used to predict
patients’ 30 days mortality but were not used to predict
hospitalization. Patients with low systolic blood pressure and
breathing rate higher than 24 times per minute were increasing a
chance of 30 days of mortality. Variables related to albumin levels in
blood and arrhythmia were found to enable patients to stay in the
hospital again, but it was not found that they were used to create an
equation [22,23]. The prediction of patients’ body temperature on
admission, chest X-ray result showing pulmonary congestion, and
factors stimulating acute heart failure to calculate predictive scores
since patients with non-normal body temperature had a chance
to have an infection, causing them to stay in the hospital longer
than 24 hours [24,25]. The patients with pulmonary congestion
shown by chest X-ray tended to be hospitalized longer as well [26].
Patients expected that coronary heart disease is the cause of acute
coronary syndrome; they had a poor disease prediction and need to
be hospitalized [23,27,28].
Limitations
There are some limitations to this study. First, this study was a retrospective study, and some patients having incomplete medical records were excluded. Second, a cut-off at 24 hours of hospitalization was different from other studies, depending on the ED context with hospital beds’ deprivation. Meanwhile, only internal validation was conducted in this study, in which external validation should be conducted further.
Conclusion
The scores can be used to predict hospitalization or ED length of stay for more than 24 hours for acutely decompensated heart failure patients in the emergency department.
Declarations
Acknowledgements
No
Conflict of interest statement
None of the authors have any conflicts of interest to disclose.
Source of funding
The publication funding support by Ramathibodi hospital, Mahidol university.
Data availability statement
The data are not available for public access because of participants privacy concern but are available from the corresponding author upon reasonable request.
Authors’ contribution
All authors met the criteria for gaining authorship based on the recommendations of the International Committee of Medical Journal Editors.
References
- Storrow AB, Jenkins CA, Self WH, Alexander PT, Barrett TW, et al. (2014) The burden of acute heart failure on U.S. emergency departments. JACC Heart Fail 2(3): 269-277.
- Thomas S, Andrew J, Gary B, Francis S (2009) Optimizing clinical outcomes in acute decompensated heart failure. US Cardiology 6(1): 50-54.
- Moleerergpoom W, Hengrussamee K, Piyayotai D, Jintapakorn W, Sukhum P, et al. (2013) Predictors of in-hospital mortality in acute decompensated heart failure (Thai ADHERE). J Med Assoc Thai 96(2): 157-164.
- Silvester K, Harriman P, Walley P, Burley G (2014) Does process flow make a difference to mortality and cost? An observational study. International Journal of Health Care Quality Assurance 27(7): 616-632.
- Alnajashi MA, Almasoud MA, Aldaham SA, Acuna JM, Zevallos JC (2016) Association of gender and length of stay among Puerto Ricans hospitalized with decompensated heart failure. Medicine (Baltimore) 95(29): e4255.
- Formiga F, Chivite D, Manito N, Mestre AR, Llopis F, et al. (2008) Admission characteristics predicting longer length of stay among elderly patients hospitalized for decompensated heart failure. Eur J Intern Med 19(3): 198-202.
- Joshi AV, D'Souza AO, Madhavan SS (2004) Differences in hospital length-of-stay, charges, and mortality in congestive heart failure patients. Congest Heart Fail 10(2): 76-84.
- Frigola-Capell E, Comin-Colet J, Davins-Miralles J, Gich-Saladich I, Wensing M, et al. (2013) Trends and predictors of hospitalization, readmissions and length of stay in ambulatory patients with heart failure. Rev Clin Esp (Barc) 213(1): 1-7.
- Krantz MJ, Tanner J, Horwich TB, Yancy C, Albert NM, et al. (2008) Influence of hospital length of stay for heart failure on quality of care. Am J Cardiol 102(12): 1693-1697.
- Whellan DJ, Zhao X, Hernandez AF, Liang L, Peterson ED, et al. (2011) Predictors of hospital length of stay in heart failure: Findings from get with the guidelines. J Card Fail 17(8): 649-656.
- Krumholz HM, Chen YT, Bradford WD, Cerese J (1999) Variations in and correlates of length of stay in academic hospitals among patients with heart failure resulting from systolic dysfunction. Am J Manag Care 5(6): 715-723.
- Martin-Sanchez FJ, Carbajosa V, Llorens P, Herrero P, Jacob J, et al. (2016) Length of stay in patients admitted for acute heart failure. Gac Sanit 30(3): 191-200.
- Armola RR, Topp R (2001) Variables that discriminate length of stay and readmission within 30 days among heart failure patients. Lippincotts Case Manag 6(6): 246-255.
- Oduncu V, Erkol A, Karabay CY, Kurt M, Akgun T, et al. (2013) The prognostic value of serum albumin levels on admission in patients with acute ST-segment elevation myocardial infarction undergoing a primary percutaneous coronary intervention. Coron Artery Dis 24(2): 88-94.
- Weintraub NL, Collins SP, Pang PS, Levy PD, American Heart Association Council on Clinical Cardiology and Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, et al. (2010) Acute heart failure syndromes: Emergency department presentation, treatment, and disposition: Current approaches and future aims: A scientific statement from the American Heart Association. Circulation 122(19): 1975-1996.
- Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, et al. (2008) Respiratory rate: The neglected vital sign. Med J Aust 188(11): 657-659.
- Omar HR, Guglin M (2018) Longer-than-average length of stay in acute heart failure: Determinants and outcomes. Herz 43(2): 131-139.
- Nam-Kyoo L, Lee SE, Hae-Young L, Hyun-Jai C, Won-Seok C, et al. (2019) Risk prediction for 30-day heart failure-specific readmission or death after discharge: Data from the Korean Acute Heart Failure (KorAHF) registry. Journal of Cardiology 73(2): 108-113.
- Miró Ò, Rossello X, Gil V, Martín-Sánchez FJ, Llorens P, et al. (2017) Predicting 30-day mortality for patients with acute heart failure in the emergency department: A cohort study. Ann Intern Med 167(10): 698-705.
- Pocock SJ, Ariti CA, McMurray JJ, Maggioni A, Køber L, et al. (2013) Meta-analysis global group in chronic heart failure. Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies. Eur Heart J 34: 1404-1413.
- Huynh Q, Marwick T, DePasquale C, Leung D, Hare J, et al. (2015) Roles of nonclinical and clinical data in prediction of 30-day rehospitalization or death among heart failure patients. J Card Fail 21(5): 374-381.
- Tarvasmaki T, Harjola VP, Nieminen MS, Siirila-Waris K, Tolonen J, et al. (2014) Acute heart failure with and without concomitant acute coronary syndromes: Patient characteristics, management, and survival. Journal of Cardiac Failure 20(10): 723-730.
- Ahmed A, Aboshady I, Munir SM, Gondi S, Brewer A, et al. (2008) Decreasing body temperature predicts early rehospitalization in congestive heart failure. J Card Fail 14(6): 489-496.
- Zaprutko J, Michalak M, Nowicka A, Dankowski R, Drożdż J, et al. (2017) Hospitalisation length and prognosis in heart failure patients. Kardiol Pol 75(4): 323-331.
- Kapoor JR, Kapoor R, Ju C, Heidenreich PA, Eapen ZJ, et al. (2016) Precipitating clinical factors, heart failure characterization, and outcomes in patients hospitalized with heart failure with reduced, borderline, and preserved ejection fraction. JACC Heart Fail 4(6): 464-472.
- Pandey A, Golwala H, Sheng S, DeVore AD, Hernandez AF, et al. (2017) Factors associated with and prognostic implications of cardiac troponin elevation in decompensated heart failure with preserved ejection fraction: Findings from the American heart association get with the guidelines-heart failure program. JAMA Cardiol 2(2): 136-145.
- Walter EJ, Hanna-Jumma S, Carraretto M, Forni L (2016) The pathophysiological basis and consequences of fever. Crit Care 20(1): 200.
- Kim S, McClave SA, Martindale RG, Miller KR, Hurt RT (2017) Hypoalbuminemia and clinical outcomes: What is the Mechanism behind the relationship. Am Surg 83(11): 1220-1227.
© 2020 Yuksen C. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






