- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Treatment Strategies of the Left Mean Coronary Artery Lesions
Karaca Özkan1*, Kobat Mehmet A1, Ulutaş Zeynep2 and Kivrak Tarik1
1Firat University Faculty of Medicine Cardiology, Turkey
2Elazig Fethi Sekin City Hospital, Turkey
*Corresponding author: Karaca Özkan, Firat University Faculty of Medicine Cardiology, Turkey
Submission: January 06, 2020;Published: January 21, 2020
ISSN 2578-0204Volume3 Issue2
Abstract
Left main coronary artery (LMCA) disease is the highest-risk lesion subset of ischemic heart disease and has traditionally been an indication for coronary artery bypass grafting (CABG). Recent evidence suggests comparable clinical outcomes between a percutaneous coronary intervention (PCI) and CABG for LMCA disease, with similar rates of mortality and severe composite issues, a higher percentage of stroke with CABG, and a higher rate of repeat revascularization with PCI. In this Review, we describe the pathophysiology of unprotected left primary coronary artery disease, discuss diagnostic approaches in light of new noninvasive and invasive imaging techniques, and detail risk stratification models to aid the Heart Team in the decision- making process for determining the best revascularization strategy for these patients.
Introduction
Significant left main (LM) disease is observed in only 5% of patients referred for a coronary angiogram, involving the distal bifurcation in the majority of cases [1] with a significant prognostic impact [2]. Significant left main coronary artery (LMCA) disease is the highestrisk lesion subset and is associated with poorer clinical outcomes compared with none-LMCA CAD. Medical treatment has yielded unacceptable results with a mortality of around 50% at three years [2] and surgery, considered the gold standard strategy, has shown its superiority over medical therapy on death for decades [3]. With the remarkable improvements in medical device technology, procedural techniques, antithrombotic agents, and background medical therapy during the last two decades, PCI with stenting for LMCA disease has become technically feasible. It shows favourable clinical outcomes [4]. Two randomized clinical trials published in 2016, EXCEL and NOBLE, demonstrated the safety and efficacy of PCI compared with CABG surgery in selected patients with unprotected left main coronary artery disease, showing similar survival with CABG surgery and PCI at midterm follow- up [5,6]. Although studies with long- term follow- up are warranted, PCI might be considered an alternative revascularization strategy for selected patients with unprotected left main coronary artery disease.
Anatomy and Pathophysiology
The left main coronary artery arises from the left aortic sinus, below the sinotubular
junction, and ends by bifurcating into the left anterior descending artery and left circumflex
artery and, in one- third of the patients, by trifurcating with an intermediate ramus. The left
main coronary artery has an average length of 10mm (2-23mm), with a mean diameter of 3.9
± 0.4mm in women and 4.5 ± 0.5mm in men [7], and is divided into three parts: ostium, shaft,
and a distal segment. The lesion may be underestimated, and mathematical models should
be used to determine the correct diameter of the proximal MV according to the distal MV
and SB diameters [8]. The simplified law of Finet can be used in Daily practice (Proximal LM
diameter=0.678 (left anterior descending artery (LAD)+circumflex diameters)) [9].
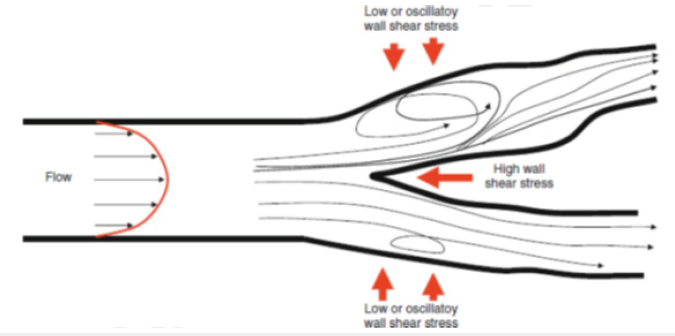
The development of atherosclerosis in the left main coronary artery has been linked to
flow haemodynamics, with atherosclerotic plaques described at areas of low endothelial
shear stress in the lateral wall of the bifurcation (Figure 1), opposite to the carina [10]. Conversely, the carina is often free from disease, probably owing to
the protective effect of high shear stress against plaque formation
(Figure 1); [11]. The length of the left main coronary artery also
influences stenosis location and morphology. In short left main
coronary arteries (<10mm), lesions develop more frequently near
the ostium than in the bifurcation (55% versus 38%). In contrast,
in long arteries, lesions develop predominantly near the bifurcation
(ostium 18% versus bifurcation 77%) [12,13]. Moreover, the PCI
strategy for LM treatment should be anticipated by a thorough
examination of the anatomy of the bifurcation lesion using tools
such as the Medina classification [14], and difficulties should be
assessed utilizing the SYNTAX score allowing a risk stratification of
the procedure into low, intermediate or high-risk [15].
Figure 1:Role of endothelial shear stress in atherosclerotic plaque formation in the left main coronary bifurcation. Endothelial shear stress is the tangential force derived from the friction of the flowing blood on the endothelial surface and is the product of the shear rate at the wall and the blood viscosity. In arterial regions with disturbed laminar flow, low endothelial shear stress shifts the endothelial function and structure towards an atherosclerotic phenotype, thereby promoting atherogenesis, atherosclerotic plaque formation and progression, and vascular remodelling. In contrast, the carina is exposed to high shear stress [13].
Use of Intracoronary Imaging
IVUS can provide an estimate of the ischemic burden of the LM
lesion, and its use following LM PCI improves clinical outcomes [16].
In the multicenter prospective LITRO study [17] of intermediate
LM stenosis between 25% and 60%, deferring revascularization of
LM lesions with minimal luminal area (MLA) of ≥6 mm2 (53% of
lesions) was safe and associated with favourable outcomes at two
years of follow-up (cardiac death-free survival of 97.7%). Although
IVUS is good at describing the anatomical extent of disease, the LMMLA
cutoff for determining a functionally significant lesion differs
between populations. Thus these values need to be interpreted with
caution. The other benefit of IVUS is to ensure stent optimization
of LM PCI. IVUS can ensure adequate expansion and apposition of
stents after LM PCI, which improves clinical outcomes following LM
PCI, particularly in patients with distal LM lesions and those treated
with a 2- stent strategy [16].
In a Korean study, the MLA cutoff for FFR <0.80 was 4.5mm2
with a sensitivity of 77% and a negative predictive value of
75%,[18] whereas another US study yielded a cutoff value of
5.9mm2 with a sensitivity and specificity of 93% and 94%,
respectively, for an FFR<0.75 [19]. Optical coherence tomography
is another intracoronary imaging modality that is often employed
for lesion characterization and PCI guidance in non-LMCAD,
particularly given its higher resolution imaging. Another drawback
of optical coherence tomography use in LM imaging is its limited
penetration depth (2-3mm) as compared with IVUS (4-8mm), given
that the average LMCA diameter is 3.5 to 4.5mm. Finally, literature
regarding clinical outcomes or correlation with physiology for
optical coherence tomography in LMCAD is lacking.
Treatment
A meta-analysis of the early studies showed that patients with unprotected left main coronary artery disease had the highest survival benefit with surgical revascularization (OR 0.32, 95% CI 0.15-0.70, P = 0.0004), establishing CABG surgery as the treatment of choice for these patients [3]. Surgical myocardial revascularization techniques have evolved with developments in off-pump and clampless procedures, periaortic ultrasonography, conduit selection for total arterial revascularization, intraoperative graft assessment, and minimally invasive procedures [20].
The development of drug-eluting stents (DESs) has markedly
improved the prognosis after PCI in patients with unprotected
left main coronary artery disease, with randomized trials
demonstrating a similar survival with PCI and CABG surgery at
midterm follow- up. In the SYNTAX randomized trial, LM PCI with
first-generation DES as compared to CABG in a subgroup of patients.
In patients with a SYNTAX score <33, significant adverse events and
mortality were similar at five years, albeit with an increased risk of
target lesion revascularization in the PCI group (23%) [21].A recent
meta-analysis of the four randomized trials comparing the firstgeneration
DES to CABG in LM disease confirmed the non-inferiority
of PCI concerning mortality and MACE [22]. This meta-analysis
highlighted a higher risk of stroke at one year in the surgery group
and established a higher risk of target vessel revascularization in
the PCI group. The EXCEL study reported an initial benefit of PCI
within the first month concerning the primary endpoint [23].
However, a reversal of results was observed between 30 days and
three years with a higher target vessel revascularization in the
PCI group. Nevertheless, the non-inferiority of PCI for the primary
endpoint was reached at three years.
In the NOBLE study, PCI was inferior to CABG at 5-years’ followup
due to a higher rate of non-procedural myocardial infarction
in the PCI group with an unusual trend towards a higher rate of
stroke in the PCI group [24]. In both these recent trials with newgeneration
DES, target vessel revascularization was comparable to,
and nearly twice as low as the TLR reported in the SYNTAX study,
suggesting improved outcomes with new-generation devices.
Moreover, these two studies provide consistent data suggesting
the safety of both strategies with a long-term benefit associated
with surgery despite a primary benefit of PCI in the EXCEL trial.
Four consecutive randomized clinical trials (RCTs) comparing
early-generation DES and CABG reported similar results [25,26].
Overall, the rates of death or MI were identical between the two
groups; however, stroke was more familiar with CABG, and repeat
revascularization was more common with PCI. Subsequently,
several meta-analyses have confirmed these findings [27,28].
Contemporary standards of PCI for unprotected left main
coronary artery disease include pre-procedural imaging and
functional assessment, procedural planning based on clinical and
anatomical characteristics with the use of new- generation DES
with thin struts and bioresorbable or biocompatible polymer,
lesion preparation and stenting with proximal optimization with
or without kissing balloon inflation based on the chosen technique,
post-procedural imaging and functional assessment with further
optimization as necessary and potent dual antiplatelet therapy
after the procedure [29]. The provisional stenting strategy begins
with implantation of a single stent and allows SB stenting only in
cases of incomplete results. The provisional stent has, consequently,
become the default strategy in bifurcation lesions and is considered
the most appropriate option for LM PCI. The literature shows that
a high rate of single-stent plan can be achieved when provisional
stenting is performed, with a trend towards a lower incidence of
significant events and target lesion revascularization in registries
[30,31], but with a probable bias regarding the flat rate of “true
bifurcation” (Medina 111) in these studies.
A two-stent strategy is implemented in a limited number of
cases and may be needed in the presence of ≥2.50mm SB diameter
and >50% diameter stenosis as well as in lesions difficult to wire or
in cases of extensive disease >5-10mm according to criteria from
the European bifurcation club II trial [32]. Recently, the randomized
DKCRUSH-V study challenged results from registries with less
target lesion failure in patients treated for “true bifurcation” LM
disease with a DK-crush two-stent strategy compared to those with
a provisional stenting strategy [33]. The outcomes of the two-stent
strategies for the LM do not differ in the literature between T-stent
and crush techniques [34]. Still, the incidence of MACE was reduced
with the DK-crush method in comparison to the culotte technique
in a recent trial [35].The European Bifurcation Club recommends
the KISSS principle (Keep it simple, swift and safe) [34]. The T-stent
technique is the most appropriate option for distal LM PCI as the
angle between the LAD, and the circumflex is approximately 90°
and is associated with good outcomes [36]. An optimal view should
be selected to avoid missing the SB ostium during deployment
of the second stent (Figure 1). The TAP technique with minimal
stent overlap is also appropriate for distal LM bifurcation. This
technique should be avoided in narrow angles because of a risk of
late endothelialization associated with the potential presence of a
long metallic carina.
The culotte technique may be appropriate for distal LM if the
angle between the LAD and the circumflex is inferior to 60° and if
both branches have similar diameters. The culotte technique has
been studied in clinical trials with favourable results [32]. The first
stent is deployed from the LM to the most angulated branch, which
is frequently the circumflex. Short stent overlap in the proximal
MV and rewiring of the MV near the carina are recommended. The
V-stent technique, whereby two stents are positioned at the ostium
of the LAD and the the ostium of the circumflex is only used in
the presence of Medina 0, 1, 1 distal LM disease. The mini-crush
technique is a variation of the standard crush technique allowing
minimal overlapping of stent struts. The first stent is usually
deployed in the circumflex with minimal protrusion into the LM
and with simultaneous positioning of the second stent from the LM
to the LAD. The second stent is subsequently deployed by crushing
the proximal part of the circumflex stent. The circumflex is then
rewired through a proximal strut, and the struts are opened. The
DK-crush technique may also be implemented in the presence of
distal LM stenosis (Figure 2). The SB is stented first. A balloon is
crushed in place from the LM to the LAD. The first kissing balloon
inflation is carried out before deployment of the second stent from
the LM to the LAD. The second kissing balloon inflation is performed
once the two stents are deployed [35].
Figure 2:PCI bifurcation techniques for patients with unprotected left main coronary artery disease.

The percutaneous coronary intervention (PCI) provisional onestent technique is the recommended approach for the Majority of bifurcation lesions. After stent implantation in the main branch, proximal optimizing method (POT) allows for the reconstruction of the initial anatomy of the bifurcation and facilitates wire exchange. After POT, a final kissing balloon dilatation (that is, simultaneous inflation of two coronary balloons in the main and side branch) can be performed. For approximately 15% of bifurcation lesions, a two- stent technique is required. The choice is left to the operator, but technique selection might also depend on the bifurcation angulation. T- stenting is preferred for T- shape angulation, whereas T and protrusion (TAP) stenting or culotte stenting is preferred for Y- shape angulation. In all two- stent cases, high- pressure side branch and main vessel dilatation is mandatory to achieve full stent expansion. A final re- POT should be considered to correct for proximal main vessel stent distortion if overlapping of the two balloons occurred proximal to the polygon of confluence. V- stenting and simultaneous kissing stenting (SKS) are less commonly used and can be considered in cases involving only the left anterior descending artery or the circumflex artery. The double- kissing (DK) crush technique has been proposed for unprotected left main coronary artery disease treatment. In DK crush stenting, one balloon is introduced into the main vessel and a stent deployed at the side branch. The balloon in the main vessel is then inflated to crush the side branch stent after its deployment. After rewiring the side branch proximally, first kissing is performed, followed by stenting of the main vessel. Final kissing balloon inflation is conducted after rewiring the side branch from the proximal main vessel stent cell. After stenting both the main vessel and the side branch, POT should be performed to improve main vessel stent strut apposition [37].
Conclusion
Patients with significant unprotected left main coronary artery disease should undergo prompt revascularization. Noninvasive and invasive diagnostic imaging with the use of adjunct methods is often required to assess the need for revascularization. Both PCI and CABG have proven to be therapeutic options for LM disease revascularization with comparable short-term safety in patients with low to intermediate SYNTAX score. Developments in the field of percutaneous revascularization including refinements in patient selection, improvements in device technology, implantation techniques, and medical therapy have made PCI a feasible, safe, and effective alternative to CABG surgery for unprotected left main coronary artery disease. The results of the EXCEL and NOBLE trials may reposition the therapeutic role and change the recommendation for PCI relative to CABG for patients with LMCA disease.
References
- DeMots H, Rösch J, McAnulty JH, Rahimtoola SH (1977) Left main coronary artery disease. Cardiovasc Clin 8(2): 201-211.
- Taylor HA, Deumite NJ, Chaitman BR, Davis KB, Killip T, et al. (1989) Asymptomatic left main coronary artery disease in the Coronary Artery Surgery Study (CASS) registry. Circulation 79(6): 1171-1179.
- Yusuf S, Zucker D, Peduzzi P, Fisher LD, et al. (1994) Effect of coronary artery bypass graft surgery on survival: Overview of 10-year results from randomised trials by the coronary artery bypass graft surgery trialists collaboration. Lancet 344(8922): 563-570.
- Harskamp RE, Park DW (2015) Stenting versus surgery for the significant left main disease. Curr Cardiol Rep 17(4): 18.
- Stone GW, Joseph FS, Patrick WS, Charles AS, Philippe G, et al. (2016) Everolimus- eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med 375: 2223-2235.
- Makikallio, T, Holm NR, Lindsay M, Spence MS, Erglis A, et al. (2016) Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): A prospective, randomised, open-label, non- inferiority trial. Lancet 388(10061): 2743-2752.
- Dodge JT, Brown BG, Bolson EL, Dodge HT (1992) Lumen diameter of normal human coronary arteries. Influence of age, sex, anatomic variation, and left ventricular hypertrophy or dilation. Circulation 86(1): 232-246.
- Motreff P, Rioufol G, Gilard M, Caussin C, Ouchchane L, et al. (2010) Diffuse atherosclerotic left main coronary artery disease unmasked by fractal geometric law applied to quantitative coronary angiography: An angiographic and intravascular ultrasound study. EuroIntervention 5(6): 709-715.
- Huo Y, Finet G, Lefèvre T, Louvard Y, Moussa I, et al. (2012) Optimal diameter of diseased bifurcation segment: A practical rule for percutaneous coronary intervention. EuroIntervention 7(11): 1310-1316.
- Chatzizisis YS, Coskun AU, Jonas M, Edelman ER, Feldman CL, et al. (2007) Role of endothelial shear stress in the natural history of coronary atherosclerosis and vascular remodeling: Molecular, cellular, and vascular behaviour. J Am Coll Cardiol 49(25): 2379-2393.
- Slager CJ, Wentzel JJ, Gijsen FJ, Schuurbiers JC, van der Wal AC, et al. (2005) The role of shear stress in the generation of rupture-prone vulnerable plaques. Nat Clin Pract Cardiovasc Med 2(8): 401-407.
- Maehara A, Mintz GS, Castagna MT, Pichard AD, Satler LF, et al. (2001) Intravascular ultrasound assessment of the stenoses location and morphology in the left main coronary artery about anatomic left main length. Am J Cardiol 88(1): 1-4.
- Chatzizisis YS, Jonas M, Coskun AU, Beigel R, Stone BV, et al. (2008) Prediction of the localization of high-risk coronary atherosclerotic plaques based on low endothelial shear stress: An intravascular ultrasound and histopathology natural history study. Circulation 117(8): 993-1002.
- Medina A, Suárez de Lezo J, Pan M (2006) A new classification of coronary bifurcation lesions. Rev Esp Cardiol 59(2): 183.
- Sianos G, Morel MA, Kappetein AP, Morice M-C, Colombo A, et al. (2005) The SYNTAX Score: An angiographic tool grading the complexity of coronary artery disease. EuroIntervention 1(2): 219-227.
- Torre Hernandez JM, Baz Alonso JA, Gomez Hospital JA, Alfonso Manterola F, Garcia Camarero T, et al. (2014) Clinical impact of intravascular ultrasound guidance in drug-eluting stent implantation for unprotected left main coronary disease: Pooled analysis at the patient-level of 4 registries. JACC Cardiovasc Interv 7(3): 244-254.
- Torre Hernandez JM, Hernandez HF, Alfonso F, Rumoroso JR, Lopez PR, et al. (2011) Prospective application of pre-defined intravascular ultrasound criteria for assessment of intermediate left main coronary artery lesions results from the multicenter LITRO study. J Am Coll Cardiol 58: 351-358.
- Park SJ, Ahn JM, Kang SJ, Yoon SH, Koo BK, et al. (2014) Intravascular ultrasound-derived minimum lümen area criteria for functionally significant left main coronary artery stenosis. JACC Cardiovasc Interv 7(8): 868-874.
- Jasti V, Ivan E, Yalamanchili V, Wongpraparut N, Leesar MA, et al. (2004) Correlations between fractional flow reserve and intravascular ultrasound in patients with an ambiguous left main coronary artery stenosis. Circulation 110(18): 2831-2836.
- Head SJ, Milojevic M, Taggart DP, Puskas JD (2017) Current practice of state-of-the-art surgical coronary revascularization. Circulation 136(14): 1331-1345.
- Morice MC, Serruys PW, Kappetein AP, Feldman TE, Ståhle E, et al. (2014) Five-year outcomes in patients with the left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation 129(23): 2388-2394.
- Capodanno D, Stone GW, Morice MC, Bass TA, Tamburino C, et al. (2011) Percutaneous coronary intervention versus coronary artery bypass graft surgery in left main coronary artery disease: A meta-analysis of randomized clinical data. J Am Coll Cardiol 58(14): 1426-1432.
- Stone GW, Sabik JF, Serruys PW, Simonton CA, Généreux P, et al. (2016) Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease. N Engl J Med 375(23): 2223-2235.
- Makikallio, T, Holm NR, Lindsay M, Spence MS, Erglis A, et al. (2016) Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): A prospective, randomised, open-label, non- inferiority trial. Lancet 388(10061): 2743-2752.
- Buszman PE, Kiesz SR, Bochenek A, Peszek-Przybyla E, Szkrobka et al. (2008) Acute and late outcomes of unprotected left main stenting in comparison with surgical revascularization. J Am Coll Cardiol 51(5): 538-545.
- Ahn JM, Roh JH, Kim YH, Park DW, Yun SC et al. (2015) Randomized trial of stents versus bypass surgery for left main coronary artery disease: 5-year outcomes of the PRECOMBAT Study. J Am Coll Cardiol 65(20): 2198-206.
- Capodanno D, Stone GW, Morice MC, Bass TA, Tamburino C, et al. (2011) Percutaneous coronary intervention versus coronary artery bypass graft surgery in left main coronary artery disease: A meta-analysis of randomized clinical data. J Am Coll Cardiol 58(14): 1426-1432.
- Athappan G, Patvardhan E, Tuzcu ME, Ellis S, Whitlow P, et al. (2013) Left main coronary artery stenosis: A meta-analysis of drug-eluting stents versus coronary artery bypass grafting. JACC Cardiovasc Interv 6(12): 1219-1230.
- Rab T, Sheiban I, Louvard Y, Sawaya FJ, Zhang JJ, et al. (2017) Current interventions for the left main bifurcation. JACC Cardiovasc Interv 10(9): 849-865.
- Morice MC, Serruys PW, Kappetein AP, Feldman TE, Ståhle E, et al. (2010) Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the synergy between percutaneous coronary intervention with TAXUS and cardiac surgery (SYNTAX) trial. Circulation 121(24): 2645-2653.
- Palmerini T, Marzocchi A, Tamburino C, Sheiban I, Margheri M, et al. (2008) Impact of bifurcation technique on 2-year clinical outcomes in 773 patients with distal unprotected left main coronary artery stenosis treated with drug-eluting stents. Circ Cardiovasc Interv 1(3): 185-192.
- Hildick SD, Lassen JF, Albiero R, Lefevre T, Darremont O, et al. (2010) Consensus from the 5th European Bifurcation Club meeting. EuroIntervention May 6(1): 34-38.
- Chen SL, Zhang JJ, Han Y, Kan J, Chen L, et al. (2017) Double kissing crush versus provisional stenting for left main distal bifurcation lesions: DKCRUSH-V randomized trial. J Am Coll Cardiol 70(21): 2605-2617.
- Lassen JF, Holm NR, Banning A, Burzotta F, Lefèvre T, et al. (2016) Percutaneous coronary intervention for coronary bifurcation disease: 11th consensus document from the European Bifurcation Club. EuroIntervention 17: 12(1): 38-46.
- Chen S-L, Xu B, Han Y-L, Sheiban I, Zhang J-J, Ye F, et al. (2015) Clinical outcome after DK crush versus culotte stenting of distal left main bifurcation lesions: The 3- year follow-up results of the DKCRUSH-III Study. JACC Cardiovasc Interv 8(10): 1335-1342.
- Lefèvre T, Girasis C, Lassen JF (2015) Differences between the left main and other bifurcations. EuroIntervention 11(Suppl V): V106-110.
- Zhang JJ, Chen SL (2015) Classic crush and DK crush stenting techniques. EuroIntervention 11(Suppl V): V102–V105.
© 2020 Karaca Özkan. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






