- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Fibrosing Mediatinitis with Intracardiac Extention: A Rare Crippling Ailment-Case Report
Mariah Obino1*, Riffat Abdulaziz1, Naushad Karim2, Kevin Ombati2, Antony Gikonyo3 and Premanand Ponoth4
1Radiology Resident, Kenya
2Clinical Instructor, Kenya
3Interventional Cardiologist, Kenya
4Chief of Cardiothoracic& Vascular Surgery, Kenya
*Corresponding author: Mariah Obino, Radiology Resident, Kenya
Submission: October 21, 2019;Published: October 31, 2019

ISSN 2578-0204Volume3 Issue1
Abstract
The exact cause of fibrosing mediastinitis is not fully understood, but it is not inherited. Many cases are linked to a specific type of fungal infection called histoplasmosis. Treatment depends on which structures of the mediastinum are affected, the severity of the scarring and, in some cases, the cause of the condition.
Other less common causes of fibrosing mediastinitis include radiation therapy, autoimmune disease, tuberculosis, certain medications, Behcet’s disease, and inflammatory diseases such as sarcoidosis in roughly 10-20% of cases, the cause of fibrosing mediastinitis cannot be determined.
Keywords: Mediastinitis, Fibrosing mediastinitis, Sclerosing non-Hodgkin’s lymphoma, Intra-Cardiac tumors
Introduction
It is commonly seen in young patients with clinical features of obstruction of the superior vena cava, pulmonary vessels, airways or esophagus [1]. Fibrosing mediastinitis is an infiltrative disorder known to encase mediastinal structures [2] seen commonly in young patients. It can often be mistaken for a tumor such as nodular sclerosing Hodgkin’s lymphoma; understanding the imaging appearance and clinical presentation is therefore vital in avoiding misdiagnosis [1]. Fibrosing mediastinitis is also known as mediastinal fibrosis or sclerosing mediastinitis. This is a rare benign disorder caused by x of acellular collagen and fibrous tissue within the mediastinum that may mimic a malignant process on imaging. Two types of fibrosing mediastinitis have been described:
1. Idiopathic/non-granulomatous fibrosing mediastinitis which is an idiopathic reaction to autoimmune syndromes, use of methysergide or radiation therapy to the mediastinum.
2. Granulomatous fibrosing mediastinitis is almost always an idiosyncratic/abnormal immunological response to infectious and inflammatory conditions most commonly tuberculosis and histoplasmosis in different endemic regions [2].
Fibrosing mediastinitis has also been classified as focal and diffuse. The focal type is seen on imaging (CT or MRI) as a localized, calcified mass in the mediastinum or in the pulmonary hila. The diffuse type appears as a diffusely infiltrating, non-calcified mass traversing multiple mediastinal compartments. It is commonly seen in young patients with clinical features of obstruction of the superior vena cava, pulmonary vessels, airways or esophagus [1].
Materials and Methods
17-year-old HIV negative male, living in care home presented to a national tertiary hospital with cough, difficulty in breathing, dyspnea and fever over the past 1 year. He also had bilateral deep venous thrombosis and was on tuberculosis medication and warfarin for suspected TB and pulmonary embolism respectively.
He was referred to our institution after there was no improvement despite treatment. Full haemogram done at our institution was unremarkable except for an Hb of 10.1g/dl. Other investigations done for inflammatory process like CRP, ESR, and for TB like sputum, genetic analysis was inconclusive. The patient also underwent an echocardiogram which showed a markedly dilated right atrium with a mass adherent to the base, and dilated inferior vena cava, severe right ventricular dilatation and severe tricuspid regurgitation.
The patient was referred to the radiology department for a CT chest to further evaluate the cardiac findings as well as to evaluate the chest for evidence of tuberculosis. CT Chest showed multiple small nodes in the superior mediastinum, an ill-defined soft tissue mass extending caudally from the superior mediastinum encasing the blood vessels resulting in occlusion of the superior vena cava. The soft tissue mass extended to the right atrium, pulmonary trunk and right pulmonary artery terminating in the apical segment of the right lower lobe. A similar smaller mass was seen in the course of the left lower lobe pulmonary artery. Multiple small collateral blood vessels were seen in the mediastinum secondary to the SVC occlusion. Abnormal enhancement in the liver due to collateral flow through the vein of Sappy was also seen.
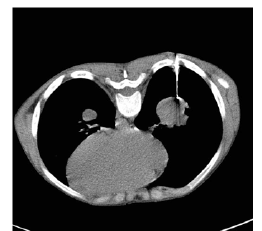
CT scan chest with contrast [Figures 1-4]
This was thought to represent an aggressive sarcoma arising from the blood vessels and the patient underwent a CT guided biopsy of the mass in the right lower lobe which showed benign fibrous tissue with no evidence of malignancy. Zn staining for TB was also negative. Due to the perceived non-concordance of the histology findings with the imaging findings, a repeat biopsy was carried out which revealed similar findings on histology. The patient then underwent an open mediastinal biopsy under cardiopulmonary bypass as the tumor mass was extending intra cardiac [Figure 5].
Figure 1:a) CT scan of the chest with contrast shows a) mediastinal mass (with no calcifications) encasing the mediastinal vessels with formation of collaterals due to resultant compression of the SVC; b) Abnormal hepatic enhancement (veins of sappy).
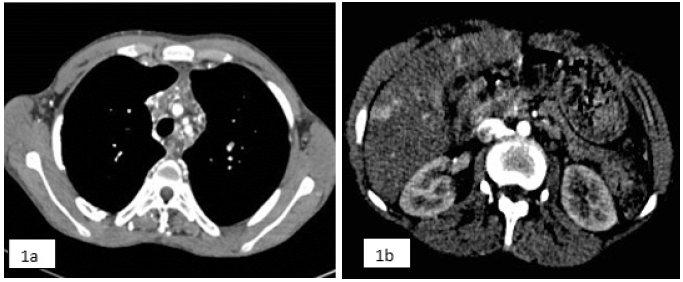
Figure 2:a) Mediastinal mass infiltrating the right atrium; b) Coronal image of the same.
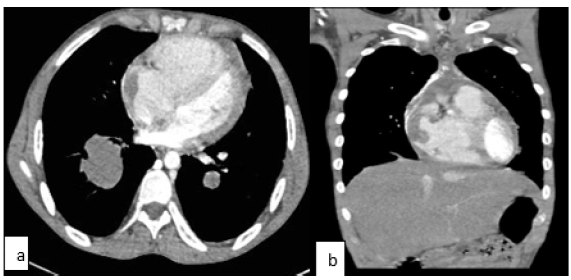
Figure 3:a) SVC not visualized as a result of the mediastinal mass encasing it completely at this level; b) CT lung window showing left bronchial stenosis as a result of the mediastinal mass.

Figure 4:a) CT scan shows encasing of the left pulmonary artery by the mediastinal mass; b) Nodular sclerosing lymphoma mimicking idiopathic fibrosing mediastinitis (images from our institution) note absence of calcifications.
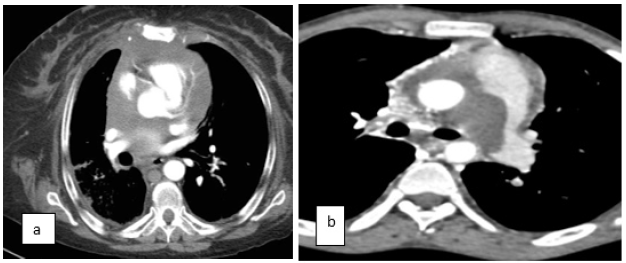
Figure 5:CT guided biopsy of the right lower lobe of right lung.
Surgical findings [Figure 6]
Chest opened by midline sternotomy. Cardiopulmonary bypass achieved with difficulty after cannulating Aorta, and Right Atrium as the whole of RA was filled with the mass, which was extending to the SVC, IVC, and PA. It was thick and fibrous and was densely infiltrating the myocardium. The initial impression was that, it could be an infiltrating malignancy. Hence tissue biopsy was taken from RA and MPA, and with routine closure followed by weaning off the pump. In the post-operative period, he was on high inotropes, and had features of cardiac failure. He succumbed on the 3rd post op day.
Histology [Figure 7]
A diagnosis of idiopathic fibrosing mediastinitis was made.
Figure 6:Per operative picture shows fibrosing mass inside RA extending to SVC, IVC and MPA.
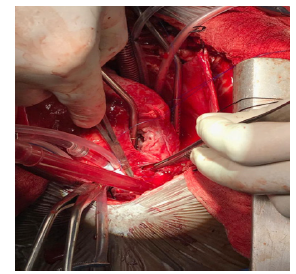
Figure 7:Histologic findings included dense fibrosis, chronic lympho-plasmacytic infiltrate, and widespread calcification.

Discussion
There is no cure for fibrosing mediastinitis, and the benefits of current treatments are unclear. In general, treatment options depend on which structures of the mediastinum are affected (i.e. the heart, large blood vessels, windpipe, esophagus, and lymph nodes), the severity of the scarring and, in some cases, the cause of the condition. For example, fibrosing mediastinitis caused by histoplasmosis may be treated with antifungal medications while cases caused by autoimmune disorders may respond best to corticosteroids. Other treatment options include surgery to removed scarred tissue and local therapies to treat specific problems (stents, laser therapy etc.). The CT findings are in keeping with diffuse type fibrosing mediastinitis which was confirmed on biopsy. The following findings were seen in our patient and have been described in literature and case reports [1-3]:
1. Superior vena cava obstruction with multiple collaterals including enhancing hepatic pseudo lesions representing collateral venous flow through the vein of Sappey.
2. Encasement of mediastinal structures including the ascending aorta without narrowing.
3. Features of right heart failure, [3] enlarged right ventricle, bowing of the interventricular septum to the left, backflow of contrast into the inferior vena cava and hepatic veins.
4. Narrowing of the left main bronchus.
The left main pulmonary artery was compressed, while its branches were encased without any stenosis. The right main pulmonary artery was markedly narrowed proximally and completely infiltrated distally with non-visualization of its branches. These appearances must be differentiated from thromboembolic disease as well as pulmonary artery sarcoma [4]. The clue in this case was extensive involvement of the thoracic inlet and anterior mediastinum not usually seen in thromboembolic disease and the young age of the patient without other risk factors like a known underlying malignancy. However, the history of recurrent DVT is concerning for superimposed thrombosis. Intracardiac masses are a rare entity and the extension of the disease process into the right atrium is unusual and made diagnosis difficult in this patient. Only one previous case of intracardiac mass due to fibrosing mediastinitis has been reported [5]. Fibrosing mediastinitis usually results from an excessive host response to a prior infection that involved the mediastinal lymph nodes. Confirmatory diagnosis of mediastinal fibrosis involves surgical biopsy with a good sample showing only fibrosis without evidence of malignancy. This is important in excluding differential diagnoses that include; sclerosing non- Hodgkin lymphoma, nodular sclerosing Hodgkin disease and pulmonary artery sarcoma [2,4]. Additional tests are usually done to rule out any granulomatous causes like histoplasmosis and tuberculosis. In our patient ZN staining for acid-fast bacilli was negative; although whether tuberculosis was the cause of the fibrosis could not be ascertained as the patient had been on anti-TB medication. It should also be noted that definitive histopathologic proof of infection by demonstrating organisms within affected tissues is absent in many cases [1].
Conclusion
Idiopathic fibrosing mediastinitis is a rare entity and there are only few case reports in the literature. It can rarely extend into the cardiac chambers presenting as an intracardiac mass [5] is even rare. It has a propensity to infiltrate the pulmonary vasculature which has to be differentiated from pulmonary embolism. Extensive mediastinal involvement without calcification in the diffuse type of mediastinal fibrosis can mimic nodular sclerosing Hodgkin’s lymphoma. Familiarity with the various imaging features of fibrosing mediastinitis is important for prompt and accurate diagnosis and may preclude an invasive life-threatening biopsy procedure if images are interpreted in the correct clinical context.
References
- Rossi SE, McAdams HP, Rosado-de-Christenson ML, Franks TJ, Galvin JR, et al. (2001) Fibrosing mediastinitis. Radiographics 21(3): 737-757.
- McNeeley MF, Chung JH, Bhalla S, Godwin JD (2012) Imaging of granulomatous fibrosing mediastinitis. Am J Roentgenol 199(2): 319-327.
- Seferian A, Steriade A, Jaïs X, Planché O, Savale L, et al. (2015) Pulmonary hypertension complicating fibrosing mediastinitis. Medicine (Baltimore) 94(44): e1800.
- Jeong N, Seol SH, Kim IH, Kim JY (2016) Pulmonary artery sarcoma-Multimodality imaging. J Clin Imaging Sci 6: 45.
- Pereira-da-Silva T, Galrinho A, Ribeiro A, Jalles N, Martelo F, et al. (2013) Intracardiac mass due to fibrosing mediastinitis: The first reported case. Can J Cardiol 29(8): 1015.
© 2019 Mariah Obino. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






