- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
A Case Report of Coarctation of Aorta Presenting as ST Elevation in Anterior Chest Leads of ECG with Severe Left Sided Neck Pain
Hammad S1*, Salahuddin M2 and Altaf A2
1 Postgraduate Resident FCPS-II Cardiology Department, Pakistan
2 FRCP Associate Professor and Consultant Cardiology Department, Pakistan
*Corresponding author: Hammad S, Postgraduate Resident FCPS-II Cardiology Department, Pakistan
Submission: March 18, 2019;Published: March 26, 2019

ISSN 2578-0204Volume2 Issue5
Abstract
Coarctation of aorta is characterized by narrowing of the aortic lumen. Complex lesion are complicated by associated cardiac anomalies and picked in infancy while simple coarctations are not diagnosed until adulthood when it manifests as secondary hypertension or its complications. We are reporting a case of severe coarctation of aorta which presented as ST elevation on anterior chest leads with severe sudden onset left sided neck pain mimicking anterior wall myocardial infarction and patient was thrombolysed due to dynamic ECG changes and new onset severe left sided neck pain. Clinicians and cardiologists worldwide should be aware of such occurrence to prevent unnecessary thrombolysis in patients not fullfiling other criteria of myocardial infarction. Bedside echo assessment and highly sensitive cardiac troponin and inflammatory markers (hs-CRP) could help in correctly aiding to diagnosis and preventing such occurrences from happening which can complicate into life threating hemorrhage.
Abbreviations: DHQ: Head Quater Hospital; STEMI: ST Elevation Myocardial Infarction; DHQ: District Head Quater Hospital; BLIs: Base Line Investigations; RAS: Renin Angiotensis System
Introduction
Coarctation of aorta is characterized by narrowing of the lumen of the aorta. It is important treatable cause of secondary hypertension and has a prevalence of 5-8% in congenital heart diseases [1]. Pathologically it is a result of intimal hyperplasia or medial thickening. Cardiac anomalies associated with it include bicuspid aortic valve, ventricular septal defect, patent ductus arteriosis, aortic stenosis or mitral stenosis. Noncardiac defects associated with it includes gonadal dysgenesis and turner syndrome [2] Aortic coarctation associated with other anomalies is complex and detected early in infancy while simple coarctation remains undetected until adulthood. It manifests mostly in adults as hypertension or its sequential complications. Coarctation by itself has no direct causal relationship with acute coronary syndrome and is not a first line differential diagnosis of cardiac referred pain and ECG showing ST elevations.
Case Presentation
A 37-year-old young patient with no previous history of congenital heart disease was referred to us with complaints of sudden onset severe left sided neck pain for the past 6 hours, which was severe in intensity and radiating to interscapular region. He had associated nausea with no shortness of breath and sweating. The pain had no relationship with food or posture. He was a driver by profession and had no history of alcohol consumption, straining, trauma or vomiting. He went to local District Head Quater Hospital (DHQ), satellite hospital with limited facilities and no cath lab, where he was diagnosed as acute anterior wall ST elevation myocardial infarction (STEMI) on the basis of dynamic ECG changes and atypical neck pain. He was immediately thrombolysed with 1.5 Million units of streptokinase. Arrival ECGs of CCU and subsequent dynamic changes of DHQ satellite hospital are shown in Figure 1(a-b). After thrombolysis patient was referred to us for subsequent management of STEMI. The pain did not decrease in intensity after thrombolysis. On initial examination he had a BP of 140/90 with 94BPM heart rate. Baseline ECG done in ER of our tertiary care hospital showed anterior wall STEMI and tentative diagnosis of failed thrombolysis was made as shown in Figure 2.
Figure 1-a:ECG in CCU of DHQ (satellite hospital) showing ST Elevation in Anterior Chest Leads V2-V4..
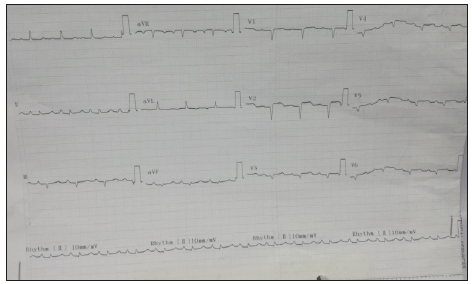
Figure 1-b:Subsequent serial ECG in CCU of DHQ (satellite hospital) showing dynamic changes in leads V2-V5.

Figure 2:ECG in ER of tertiary care hospital showing failed thrombolysis.

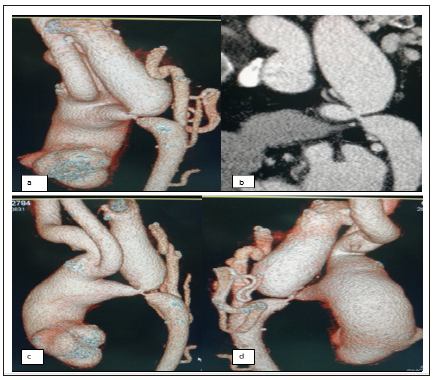
Urgent bedside echo was done which showed no regional wall motion abnormality with LVEF of 60% and a dilated aortic root. Baseline investigations (BLIs) including cardiac enzymes (hs- TROP I) were sent immediately and patient admitted to CCU for observation. To rule out aortic dissection patient was planned for CT Aortogram. In the mean while during detailed examination of the patient a note was made of radiofemoral delay which prompted us to check for BP in lower extremities. BP measurement of both lower feet showed readings of 93/54mmHg and 91/51mmHg respectively. Suspicion shifted to possible diagnosis of coarctation of aorta. BLIs showed a normal hs-TROP I level of 3.8ng/dl with normal serum creatinine of 0.83mg/dl. Chest X-ray showed widened mediastinum. CT aortogram was done which showed severe coarctation of aorta at the origin site of subclavian artery as shown in both routine and 3D reconstruction images in Figure 3. Patient was planned for urgent surgical repair and shifted to cardiac surgey unit for subsequent management where he underwent uneventful successful repair of aortic coarctation.
Figure 4:CT Aortogram
a) sagittal view.
b) 3-D reconstruction oblique view.
c) 3-D reconstruction anterior view.
d) 3-D reconstruction posterior view
Discussion
Simple coarctation of aorta with no associated cardiac and non-cardiac lesions are detected in adult life due to secondary hypertension or investigated due to presence of a murmur. It is very unlikely for patient to survive long term without repairing the coarctation defect as been reported by Cevik S et al. [3] in a very rare case report. There are 2 proposed explanation of hypertension in coaractation of aorta, first a direct causal consequence of mechanical obstruction or secondly due to maladoptation of Renin Angiotensis System (RAS) [4] Hence, hypertension or its associated complications are the sole presentation feature of coarctation of aorta when it is diagnosed in the adulthood [5]. Our case is very unusual and rare because it is diagnosed in adulthood and its presentation was not due to hypertension or its complications but atypical sudden onset neck pain with dynamic ST elevations in anterior chest leads for which he was thrombolysed in satellite hospital with streptokinase. Normal cardiac markers, no regional wall motion abnormality and differential hypertension prompted us to look for alternative diagnosis of severe neck pain. A CT aortogram was performed which diagnosed it as severe coartation of aorta at the origin site of subclavian artery. Two possible explanations for neck pain are compressive cervical myelopathy as been reported by Mourya C et al. [6] or diminished transient blood flow due to vasospasm. Dynamic ECG changes are more in favour of vasospasm but a combination of both can’t be ruled out. Craford was the surgeon who got the distinction of doing first successful surgical repair of coarctation of aorta in 1944 [7] The treatment has evolved afterwards and our case was also referred to cardiac surgeon due to complex anatomical position of the coarctation segment in the aorta.
Conclusion
Coarctation of aorta can rarely mimic STEMI due to vasospasm and compression myelopathy happening together and can result in unnecessary thrombolysis which can have catastrophic outcomes as severe hemorrhage because patients of coarctation are prone to have AV malformations.
Recommendation
Patients should not be diagnosed as STEMI on mere ECG changes and cardiac pain, but complete bedside assessment should be done including physical examinations, bedside echo for regional wall motion abnormality and levels of highly sensitive cardiac and inflammatory markers like hs-Trop I and hs-CRP in blood should be checked to avoid unnecessary thrombolysis.
References
- Rao PS (2005) Coarctation of the aorta. Curr Cardiol Rep 7(6): 425-434.
- Levine JC, Sanders SP, Colan SD, Jonas RA, Spevak PJ (2001) The risk of having additional obstruction lesions in neonatal coarctation of the aorta. Cardiol Young 11(1): 44-53.
- Cevik S, Izgi C, Cevik C (2004) Asymptomatic severe aortic coarctation in an 80 year old man. Tex Heart Inst J 31(4): 429-431.
- Singh HS, Kalim O, Osten M, Bonson LN, Horlick EM (2003) Coarctation of aorta 16: 235-236.
- Puar THK, Mok Y, Debajyati R, Khoo J, How CH, et al. (2016) Secondary hypertension in adults. Singapore Med J 57(5): 228-232.
- Mourya C, Verma A, Bansol A, Shukla RC, Srivastava A (2016) Myelopathy in adult aortic coarctation: Causes and caveats of an atypical presentation. Indian J Radiol Imaging 26(4): 451-454.
- Kvitting JP, Olin CL (2009) Clarence crafoord: A giant in cardiothoracic surgery, the first to repair aortic coarctation. Ann Thorac Surg 87(1): 342-346.
© 2019 Hammad S. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






