- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Complete Atrioventricular Block During the Placement of a Central Jugular Tunneled Catheter for Hemodialysis at The University Clinical Hospital of Santiago De Compostela, Spain
Iyad Abuward Abu sharkh*, Igor Romaniouk J, Suleyka Puello Martinez and Candido Diaz Rodriguez
Nephrology Service, University Clinical Hospital of Santiago, Spain
*Corresponding author: Iyad Abuward Abu sharkh, Nephrology Service, University Clinical Hospital of Santiago, Rua de la Choupana s/n, Santiago de Compostela, 15706, Spain
Submission: July 09, 2018;Published: July 19, 2018

ISSN 2578-0204Volume2 Issue3
Abstract
The central venous access is one of the most common procedures in interventional nephrology [1-3]. One of the known complications of this procedure is the right branch lesion of the His bundle that leads to temporary or permanent blockage. This may go clinically unnoticed in some patients, but in others, especially with previous blockage of the left branch, it might lead to a complete atrioventricular block (AVB), placing the patient at risk [4,5]. We present a case of a 70-year-old patient with chronic kidney disease (CKD) stage G5A3 who, after an attempt of placing a right jugular tunneled catheter for hemodialysis, developed a complete atrioventricular block (AVB).
Clinical Case
A 70-year-old woman with chronic kidney disease (CKD) stage G5 with a stage 3 albuminuria of multifactorial origin was followed up in our CKD unit; she was on the “surgical list” of Vascular Surgery, waiting for a vascular access intervention.
figure 1:Left bundle branch block, prior to a tunneled jugular venous catheter placement.
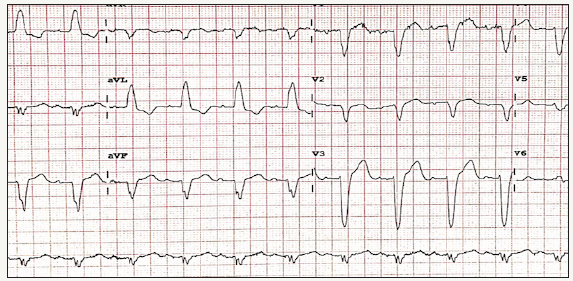
Among the personal history: type I obesity, long term hypertension, asymptomatic block of a left branch (Figure 1). Type 2 diabetes mellitus, hyperlipidemia, hyperuricemia with gout crisis, chronic ischemia of the lower limb, multiple biliary lithialsis, diverticles in the descending colon and sigma. Complicated cyst in right kidney, high grade non-Hodgkin lymphoma diagnosed in 1992 in prolonged remission compatible with cure; Autologous bone marrow transplant in 1993. Intervention of cataracts in 1997. Admission in gynecology for hysterectomy and double adnexectomy in 2001 due to an adenocarcinoma on endometrial polyp. Admission in internal medicine in May 2008th for preseptal facial cellulitis and later in May 2016th for a congestive heart failure with a normal echocardiogram for the patients age, respiratory infection with partial respiratory failure and probable left parahilar pneumonia. The usual treatment consisted of: Aranesp 30msg every 21 days, torasemide 5mg (1-0-1), trajenta 5mg (1-1-0), amlodipine 5mg (1-0-0), carduran neo 4mg (0-0-1), simvastatin 20mg (0-0- 1), alopurinol 100mg (0-0-1 / 2), ferrogradument 105mg (1-0-1), hidroferol 0.266mg every 15 days, fosrenol 750mg (1-1 -1), serc 8mg (1-1-1), bicarbonate 1gr. (1-1-0).
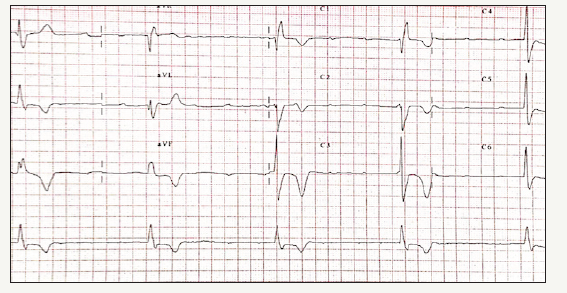
The patient initiates hemodialysis on 30/05/2016. Previously on 25/05/2016th a tunneled central catheter was placed in the right innominate vein. Adequate antiseptic measures were taken, and the patient was monitored at all times. Under ultrasound control, after introducing 20cm of the guide, the patient presents hypotension and bradycardia, and a complete atrioventricular block with a heart rate of 30bpm detected in ECG (Figure 2), after administering atropine, without any response, it is transferred to the intensive care unit placing an external pacemaker. After 24 hours, the patient recovered the base rhythm. Given his cardiological history, it was later decided to place a definitive pacemaker.
figure 2:Complete atrioventricular block when placing a central venous catheter, requiring an urgent pacemaker placement
Conclusion
The right bundle branch block occurs during central line canalization with an approximate incidence of 3-12%, usually caused by direct mechanical trauma of the metal guide on the right branch that is very superficial, while the left branch is deeper in the myocardial tissue [4]. This may go unnoticed except in cases in which there is a previous blockage of the left branch, like this case, which with the induction of the right block leads to complete atrioventricular stop, implying an important vital risk for the patient. The blockage of the right branch in this sort of procedures is usually transient, and lasts less than 24 hours [6,7], with no clinical repercussion. These complications can be avoided by introducing the guidewire from the superior vena cava to the inferior vena cava to avoid the erroneous introduction of the guidewire or “roll up” within the ventricle and therefore, causing damage to the endocardium [8]. This technique requires fluoroscopy monitoring. Another way to avoid incorrect introduction of the guide is to enter the necessary length for safety. Studies conducted in search of the correct length showed that the average distance between the entry point and the junction of the superior cava-atrium is 18 cm, although this must be personalized according to each patient [9,10]. Although an AV block is not a frequent complication during the placement of the right jugular central venous catheter, patients with a cardiovascular history deserve special care, especially if there is a known left bundle branch block, as it was in this case.
References
- Pilar R, Alicia GT, Soldevila A, Panadero J, Miguel Cruz J (2008) Cateteres tunelizados, complicación en su inserción. Nefrologia (Madr.) 28: 543- 548.
- Lopez Fernan M, Mayor Vive S, Elios Yuste Gimenez, Joan Falco F (2008) Catéteres permanentes para hemodiálisis otra alternativa de acceso vascular. Nefrología (Madr.) 28: 543-548.
- Caldwell J, Koppikar S, Barake W, Redfearn D, Michael K, et al. (2014) Prolonged P-wave duration is associated with atrial fibrillation recurrence after successful pulmonary vein isolation for paroxysmal atrial fibrillation. J Interv Card Electrophysiol 39(2): 131-138.
- Enriquez A, Conde D, Femenia F, De Luna AB, Ribeiro A, et al. (2014) Relation of interatrial block to new-onset atrial fibrillation in patients with Chagas cardiomyopathy and implantable cardioverterdefibrillators. American Journal of Cardiology 113(10): 1740-1743.
- Tedford RJ, Forfia P (2013) Hemodynamic evaluation of pulmonary hypertension in chronic kidney disease. Adv Pulmonary Hypertension 12(2): 82-85.
- Kawar B, Ellam T, Jackson C, Kiely DG (2013) Pulmonary hypertension in renal disease: epidemiology, potential mechanisms and implications. Am J Nephrol 37(3): 281-290.
- Sheyin O, Mgbemena M, Magnus Lawson O, Salahudeen L, Pierre Louis B, et al. (2014) High grade atrioventricular block presenting with cardiac arrest. American Journal of Cardiovascular Disease Research 2(2): 31- 35.
- Madsen M, Davidsen M, Rasmussen S, Abildstrom SZ, Osler M (2003) The validity of the diagnosis of acute myocardial infarction in routine statistics: a comparison of mortality and hospital discharge data with the Danish MONICA registry. J Clin Epidemiol 56(2): 124-130.
- Napalkov P, Felici DM, Chu LK, Jacobs JR, Begelman SM (2013) Incidence of catheter-related complications in patients with central venous or hemodialysis catheters: a health care claims database analysis. BMC Cardiovasc Disord 13: 86.
- Aydin Z, Gursu M, Uzun S, Karadag S, Tatli E, et al. (2012) Placement of hemodialysis catheters with a technical, functional, and anatomical viewpoint. Int J Nephrol.
© 2018 Iyad Abuward Abu sharkh. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






