- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Echocardiographic Evaluation of Left Ventricular Function After Coronary Artery Angioplasty
A Hadi*, D Benzaroual and M Elhattaoui
Service de Cardiologie-Centre hospitalier universitaire de Marrakech, Morroco
*Corresponding author: Abdelali Hadi, Service de Cardiologie-Centre hospitalier universitaire de Marrakech, Chu Mohamed Vi Marrakech, Morroco
Submission: May 15, 2018;Published: June 06, 2018

ISSN 2578-0204Volume2 Issue2
Abstract
Objectives: Coronary angioplasty has revolutionized the management of coronary artery disease. It has not ceased to develop to become the reference method of myocardial revascularization. The aim of our study is to evaluate the ultrasound parameters of left ventricular function after coronary angioplasty.
Patients and methods: This is a prospective analytical study including patients with stable coronary artery disease with a known coronary artery anatomy programmed for coronary angioplasty. Transthoracic echocardiography was performed four hours before and seven days after myocardial revascularization.
Results: 56 patients were collected, 38 of them were male (67.9% of the cases). The mean age was 60.11±7.92 years. Modifiable cardiovascular risk factors were dominated by diabetes in 64.3% of cases, followed by hypertension in 57.1% of cases. The clinical symptoms were dominated by a typical stable angina in 53.6% of cases. At the ECG, the antero-septo-apical territory was the most affected in 52% of the cases followed by the posterior territory in 46% of the cases; the depression of the ST segment was noted in 46% and negative T waves in 32% of cases. . The left anterior descending artery was affected in 66% of cases followed by right coronary artery in 13% of cases. Echocardiography was performed in all our patients 4 hours before and 7 days after angioplasty, the EF mean was 49.68% ±12 vs 55.32±12 (p=0.0001). The early mitral diastolic velocity was improved after angioplasty 66.55±16 vs 69.7±18cm/s (p=0.02). As well as the tissue doppler, the E’ wave significantly improved 9.48±2.29 vs 10.02±3.38cm/s (p=0.02) whereas the left ventricular end diastolic diameter and end diastolic volume did not change after angioplasty.
Conclusion: This work emphasizes the value of revascularization in stable coronary arteries not only to improve clinical symptomatology but also to improve left ventricular diastolic function.
Keywords:Coronary angioplasty; Diastolic dysfunction; Pulsed doppler; Tissular doppler
Introduction
Diastolic dysfunction is the first consequence of myocardial ischemia in patients with severe coronary lesions. In the absence of early management, it progresses to global dysfunction. Transluminal coronary angioplasty has revolutionized the management of coronary heart disease. It has continued to develop to become the gold standard for myocardial revascularization. To evaluate improvement in left ventricular function after coronary revascularization, we conducted a study comparing ultrasound parameters of left ventricular function before and after coronary angioplasty.
Patients and Methods
This is a prospective analytic study including 56 patients suffering of chronic stable angina who are candidates for percutaneous coronary intervention (PCI) for coronary stenosis >75% of diameter. We excluded from our study all patients with atrial fibrillation, cardiomyopathy, systemic hypertension, valvular or congenital disease and patients with multi-truncal coronary lesions without complete revascularization or previous coronary revascularization. Once selected, all our patients have had a transthoracic echocardiography examination 4 hours before and 7 days after successful coronary angioplasty. We collected all the data of the diastolic and systolic left ventricular function: In TM and 2D mode (left ventricular end-systolic diameter LVES-D, left ventricular end-diastolic diameter LVED-D, the left ventricular endsystolic volume LVES-V and left ventricular end-diastolic volume LVED-V, regional wale motion abnormality- and LV biplane ejection fraction LVEF).In pulsed Doppler mode (the peak of the E-wave , A-wave , the ratio E/A, TDE, IVRT and the ITV of the aortic flow). In tissue Doppler mode (the peak of the E ‘-wave, A’ and the S ‘wave of the left ventricle. All data were analyzed using an SPSS version 17 and expressed as mean on ±SD. For all analyses a p value < 0.05 was considered significant.
Results
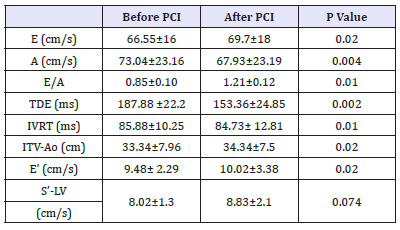
Fifty-six patients were collected and evaluated in our study. Table 1 summarizes their main clinical characterestics. The average age was 60.11±7.92 years (40-80 years). 86% of patients had at least three cardiovascular risk factors dominated by diabetes in 64.3% of cases followed by hypertension (57.1%), The history of myocardial infarction was noted in 10% of patients. The clinical history was dominated by stable angina in 53.6% of cases. In Electrocardiogram, the anterior-septo-apical territory was the most affected in 52% of cases followed by the inferior territory (46%), the depression of the ST segment was noted in 46% and negative T waves in 32% of cases. Coronary angiography showed a single vessel disease in 82% of cases dominated by left anterior descending artery’s stenosis in 66% of cases followed by right coronary (13%), marginal artery (12%), and circumflex (9%) (Figure 1). Echocardiography was performed in all our patients four hours before and 7 days after angioplasty. In TM and 2D mode, the mean left ventricular ejection fraction (LVEF) was 49.68%±12 vs 55.32±12 (p=0.0001). Analysis of regional wale motion showed severe hypokinesia in 57.1% of cases vs 41.1% after angioplasty (p=0.0035), while LVED diameters and volume did not change after angioplasty 43.9±7.22mm vs 42.68± 9mm (p=0.1) 114.6±18.8ml vs 110.16±23.85ml (p=0.06) respectively (Table 2). In pulsed Doppler, the early diastolic velocity of mitral flow (E) was improved after angioplasty 66.55±16 vs 69.7±18cm/s (p=0.02). The tissue Doppler showed an improvement of E ‘ wave significantly after PCI 9.48±2.29 vs 10.02 ±3.38cm/s (p=0.02). However, there was no significant difference of systolic wave (S’) of Left ventricle (Table 3).
Table 1:Clinical characteristics of patients: cardiovascular risk factors and history.
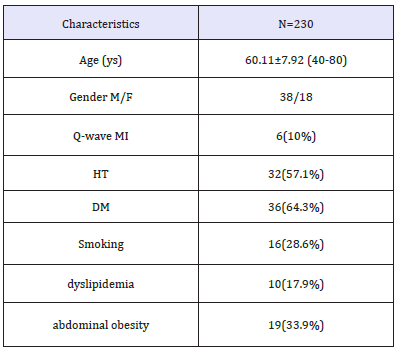
Figure 1:The results of coronarography.
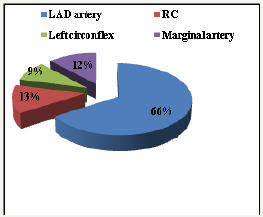
Table 2:TM and 2D mode echocardiography.
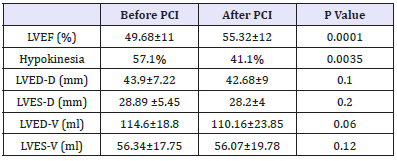
Table 3:Pulsed and tissue doppler mode echocardiography
Discussion
Echocardiography is the gold standard for evaluation of left ventricular function in chronic stable angina. The study of transmitral Doppler flow velocities, TDE, IVRT and the ratio E/A coupled to the peaks of tissue Doppler velocities reported early left ventricular diastolic dysfunction before the occurrence of the systolic dysfunction [1]. Several studies report early or late improvement in LV diastolic function following PCI. Bayata et al. [1] found that Doppler derived LV diastolic abnormalities improved within 24 hours after angioplasty. Masuyama et al. [2] report an improvement of these parameters within two days after angioplasty and continued to improve up to 9 days. Leung et al. [3] concluded that left ventricular dysfunction improved on the tenth day after revascularization and significantly better after one month. All these studies proved that the earliest echocardiographic abnormalities observed in chronic stable angina is the relaxation disorder characterized by the reduction in the E/A ratio becoming < 1, the decrease in E wave, the increase in A wave and increase in TDE and IVRT [4]. In this study we noted a statistically significant difference between the E wave; A; TDE; TRIV and E ‘after angioplasty showing improvement in abnormalities of left ventricular diastolic function. Leung et al. [3] showed a significant correlation between improvement in ventricular abnormalities and the severity of coronary stenosis. On the other hand, no significant correlation was found in Bayata et al. [1] study. Arbeille and al was interested by the evaluation of the myocardial wall contraction after angioplasty by Speckle tracking and showed a significant improvement of the global longitudinal Strain within 24 hours following angioplasty without significant difference in LVEF [5-7].
Conclusion
In this present study, we demonstrate that the revascularization of chronic stable angina was associated with an clinical and functional left ventricular improvement. Hence, we have to select the coronary patients who are symptomatic at the appropriate time to benefit from PCI.
Acknowledgment
To all personnel of cardiology department CHU Mohamed VI Marrakech-Morroco.
References
- Bayata S, Susam S, Pinar A, Dinckal MH, Postaci N, et al. (2000) New doppler echocardiographic applications for the evaluation of early alterations in left ventricular diastolic function after coronary angioplasty. Eur J Echocardiogr 1(2): 105-108.
- Masuyama T, Kodama K, Nakatani S, Nanto S, Kitabatake A, et al. (1988) Effects of changes in coronary stenosis on left ventricular diastolic filling assessed with pulsed Doppler echocardiography. J Am Coll Cardiol 11(4): 744-751.
- Leug WH, Lau CP (1991) Correlation of quantitative angiographic parameters with changes in left ventricular diastolic function after angioplasty of de left anterior descending coronary artery. Am J cardiol 67(13): 1061-1066.
- Devereux RB (1989) Left ventricular diastolic function: early diastolic relaxation and late diastolic compliance. J Am Coll Cardiol 13(2): 337- 339.
- Arbeille P, Angoulvant D, Zuj K, Patier J, Desveaux B, et al. (2013) Four dimentional spechle tracking for assessing improvement in left ventricular contractility after angioplasty. Ultrasound Med Biol 39(1): 102-110.
- Beitnes JO, Gjesdal O, Lunde K, Solheim S, Edvardsen T, et al. (2011) Left ventricular systolic and diastolic function improve after acute myocardial infarction treated with acute percutaneous coronary intervention, but are not influenced by intracoronary injection of autologous mononuclear bone marrow cells: a 3 year serial echocardiographic sub-study of the randomized-controlled ASTAMI study. Eur J Echocardiogr 12(2): 98-106.
- Munk K, Andersen NH, Schmidt MR, Nielsen SS, Terkelsen CJ, et al. (2010) Remote ischemic conditioning in patients with myocardial infarction treated with primary angioplasty: impact on left ventricular function assessed by comprehensive echocardiography and gated single-photon emission CT. Circ Cardiovasc Imaging 3(6): 656-662.
© 2018 A Hadi. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






