- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Growth Differentiation Factor 15 (GDF-15) Predicts Risk in Cardiovascular Disease -Review of the Literature
Szymon Jonik*
Department of Cardiology, Central Teaching Hospital, Medical University of Warsaw, Poland
*Corresponding author: Szymon Jonik, Department of Cardiology, Central Teaching Hospital, Medical University of Warsaw, Poland
Submission: April 02, 2018;Published: May 08, 2018

ISSN 2578-0204Volume2 Issue1
Abstract
Background: Ischaemic heart disease (IHD) including coronary artery disease and its final result-myocardial infarction is the greatest single cause of mortality and one of the most common cause of disability. To reduce mortality, it is important to pay attention to the diagnosis of ischaemia as well as the inclusion of appropriate treatment.The effectiveness of diagnosis and treatment can be increased by using new cardiac-specific markers characterized by high sensitivity and specificity whose level correlates with the severity and extent of necrosis. Such a novel biomarker seems to be growth differentiation factor 15 (GDF-15).
Methods and Results: The literature has been searched forlarge clinical trials evaluating efficacy of GDF-15 in patients with stable coronary artery disease (CAD) and acute coronary syndrome(ACS). A total number of 17,942 patients with CAD from 4 clinical trials and 26,848 patients with ACS from 8 clinical trials were included to assess the relationship between the level of GDF-15 and risk of death and major cardiovascular events during follow-up. The evaluated level of GDF-15 was proven to be correlate with increased risk of all cause of death, cardiovascular mortality, myocardial infarction, stroke and hospitalization for heart failure.
Conclusion: While the morbidity due to the IHD is still increasing, more modern methods of treatment are applied and new groups of drugs are included in the therapy, it is also understandable that the need for new, easily available and more cardiac-specific markers will be urgent. We hope, that one of them will become GDF-15.
Keywords:Coronary artery disease; Acute coronary syndrome; Growth differentiation factor 15
Introduction
Since in the 1970s, the World Health Organization (WHO) had defined the concept of myocardial infarction by the presence at least 2 of the following: acute coronary pain, dynamic changes in electrocardiogram (ECG) and elevated levels of myocardial necrosis enzymes [1], coronary artery disease (CAD) and myocardial infarction (MI) are still a major cause of morbidity and mortality worldwide. Less than 20 years ago, the new definition of MI was proposed where the importance of serological biomarkers for recognition of myocardial necrosis has been exalted [2]. Then also cardiac troponins (cTn) have been introduced [2] and remains a gold standard nowadays. Due to the large financial outlay and high mortality caused by coronary heart disease and its consequences, rapid diagnosis of chest pain and the inclusion of proper treatment, allow to significantly reduce mortality and improve prognosis. And that is why myocardial necrosis markers are so important -they not only allow to make an accurate diagnosis but also to predict the severity and extent of the disease process and plan the wayof its treatment.
Biomarkers are measurable indicators of the severity or presence of some disease states. An adequate marker of myocardial injury should meet several criteria: 1) myocardial tissue specific, but absent in non-myocardial tissue; 2) detectable in blood serum soon after the myocardial injury; 3) remains elevated in blood serum for several days from the onset of injury; 4) assayed by simple and quick method; 5) correlates with the severity of the disease and the extent of damage. Biomarkers in acute myocardial infarction are associated with various pathophysiological processes including inflammation, neutrophilic activation, necrosis, biomechanical stress and endothelial activation. As many of them are wellestablished, with cTn as a biomarker of choice for diagnosing of MI, the increasing number of novel cardiac-specific biomarkers are found each year. Although the importance of not all of them is fully proven, they may be helpful in the future in assessing the prognosis of patients with CAD or after MI.
One of such novel markers of myocardial injury is Growth Differentiation Factor 15 (GDF-15)-a member of the transforming growth factor-β (TGF-β) cytokine superfamily. It is not normally expressed in the heart, but when it comes to damage of cardiomyocytes, its level rises. The importance of GDF-15 in predicting risk in CAD and MI has been proven in many clinical trials, making it a high-quality marker in the assessment of cardiovascular prognosis [3-14].
Results
Table 1:GDF-15 as a cardiovascular biomarker in stable coronary artery disease (CAD).
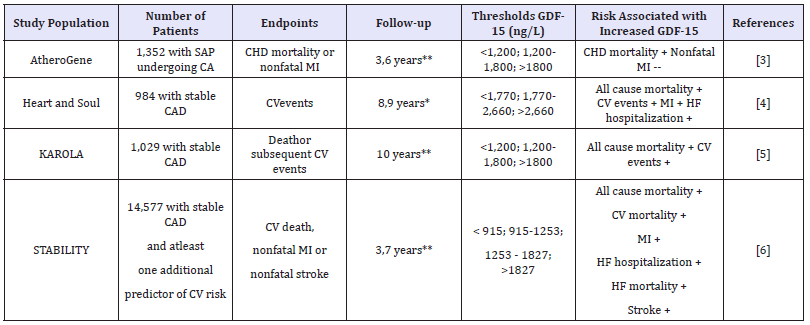
SAP: Stable Angina Pectoris; CA: Coronary Angiography; CHD: Coronary Heart Disease; MI: Myocardial Infarct; CV: Cardiovascular;
HF: Heart Failure
*mean
**median
Table 2:GDF-15 as a cardiovascular biomarker in acute coronary syndromes (ACS).
STEMI: ST-Elevation Myocardial Infarction; NSTE-ACS – Non-STEMI Acute Coronary Syndrome; MI: Myocardial Infarction; CV: Cardiovascular; PCI: Percutaneous Coronary Intervention; HF: Heart Failure;
MACE: Major Adverse Cardiovascular Events
*mean
**median
In this review, the importance of GDF-15 in assessing the risk of patients with CAD and acute coronary syndrome (ACS) based on large randomized trials was evaluated. The results were presented in Table 1 and Table 2. In AtheroGene study it was showed that patients with stable angina pectoris (SAP) presenting with normal (< 1200ng/L), moderately elevated (1200 to 1800ng/L), or markedly elevated (>1800ng/L) GDF-15 levels had 3.6-year CHD mortality rates of 1.4%, 2.7%, and 15.0%, respectively (P< 0.001) [3]. As GDF-15 remained an independent predictor of CHD mortality (P< 0.001), the level of GDF-15 did not predict the future risk of nonfatal myocardial infarction in patients with SAP or ACS [3].
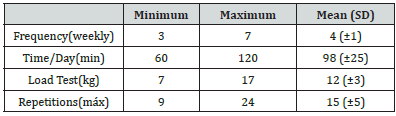
What is more, each doubling in GDF-15 was associated with a 2.5-fold increased rate of CV events (hazard ratio [HR] 2.53, 95% CI 2.13-3.01, P < 0.001) [4]. Participants who had GDF-15 levels in the highest tertile had higher mortality compared with those in the lowest tertile (HR 2.73, 95% CI 1.80-4.15, P ≤0.001 adjusted for all covariates) [4]. Elevated GDF-15 levels were associated with increased MI, HF, CV death, and all-cause mortality what was showed in Figure 1 [4].
Figure 1:Proportion of participants with CV events by tertiles of GDF-15. (From [4]).
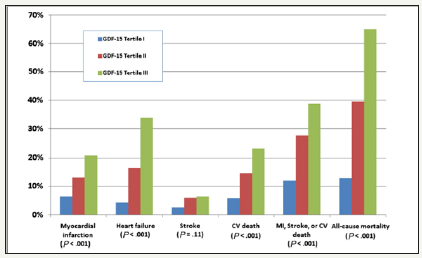
Figure 2:3-year event rates by outcome and continuous GDF-15concentration. (From [6])
In Karola study, a total number of 1,029 patients was observed for death or secondary cardiovascular event (CVE) with median follow-up of 10 years. Compared to participants with GDF-15 < 1200ng/L, increased risk for death was found in participants with GDF-15 ≥1200 and ≤1800ng/L [hazardratio (HR) 1.68 (95% CI, 1.08 -2.62)] and with GDF-15 >1800ng/L [HR 1.73 (1.02-2.94)] [5]. A 1-unit increment of ln GDF-15 was associated with an age- and sex-adjusted hazard ratio (HR) of 2.16 (95% CI, 1.66-2.82) for a subsequent CVE [5]. Compared to the reference group (< 1200ng/L) those with GDF-15>1800ng/L had an age- and sex-adjusted HR of 2.78 (95% CI, 1.90-4.07) for a subsequent CVE [5].
In STABILITY, the largest randomized clinical trial investigating the relationship between the GDF-15 level and CV risk, a total number of 14,577 patients with stable CAD and at least one additional predictor of CV risk was observed for median 3,7 years [6]- Figure 2. The hazard ratio for the composite end point for the highest compared to the lowest quartile ofGDF-15 was 1.8 (95% CI, 1.5-2.2); for CV death, 2.63 (1.9-3.6); for sudden death, 3.06 (1.9- 4.8); for heart failure (HF) death, 4.3 (1.3-14); for hospitalization for HF, 5.8 (3.2-10); for MI 1.4 (95% CI, 1.1-1.9); and for stroke, 1.8 (95% CI, 1.1-2.8) [6].
An increased levels of GDF-15 and its effect on mortality and prognosis in acute coronary syndromes (ACS) have been proven [7-14]. As was firstly showed in 2,081 patients from the GUSTO-4 admission GDF-15 concentrations are closely related to all-cause mortality in non-ST-segment elevation ACS (NSTE-ACS) [7]. Cumulative 1-yearmortality rates were 1.5, 5.0, and 14.1% in patients with low (< 1200ng/L), moderately increased (1200- 1800ng/L), and markedly increased (>1800ng/L) concentrations of GDF-15 (P< 0.001) [7]. Surprisingly, the risk of a subsequent myocardial infarction within 30 days in the respective tertiles was not significantly dependent on the increased GDF-15 level [7].
In 741 patients presented with STEMI the increased levels of GDF-15 measured before thrombolysis were associated with a higher risk of death during 1-year follow-up. Mortality rates at 1 year were 2.1, 5.0, and 14.0% in patients with GDF-15 levels < 1200, 1200-1800, and >1800ng/L, respectively (P < 0.001) -Figure 3 [8].
Figure 3:Cumulative probability of death according to levels of GDF-15 at presentation in 730 patients
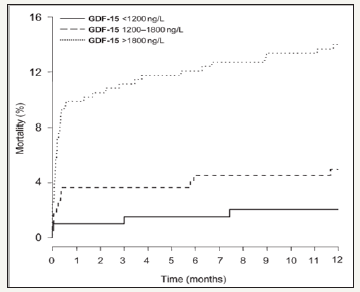
Figure 4:1-year event rate of the different outcomes. (From [9])
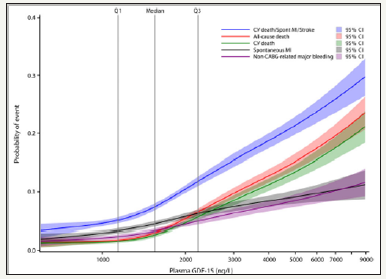
Lately, the prognostic value of GDF-15 has been reevaluated in 16,876 patients with NSTE-ACS or STEMI randomized to ticagrelor or clopidogrel in PLATO - Figure 4 [9]. Higher GDF-15 concentrations were associated with an increased risk of all-cause mortality [HR per 1 SD increase in log GDF-15,1.41 (1.31-1.53)], CV mortality [1.41 (1.30-1.53)], MI[1.15 (1.05-1.26)], and stroke [1.19(1.01-1.42)][9].
In PROVE IT-TIMI 22 the level of GDF-15 was measured in in 3,501 patients after ACS, treated with moderate or intensive statin therapy [10]. By using established cutoff points, GDF-15 (< 1200, 1200-1800, and >1800ng/L) was associated with 2-year risk of death or MI (5.7%, 8.1%, and 15.1%, respectively; P< 0.001), death (P< 0.001), MI (P< 0.001), and congestive heart failure (P< 0.001) [10].
In IABP-SHOCK II trial a total number of 190 patients with NSTE-ACS or STEMI and cardiogenic shock who underwent PCI were recruited [11]. Patients with GDF-15 level greater than the median showed higher rates of death at 30 days: 52% vs. 31%, P =0.005 (hazard ratio (HR) =1.88) [11].
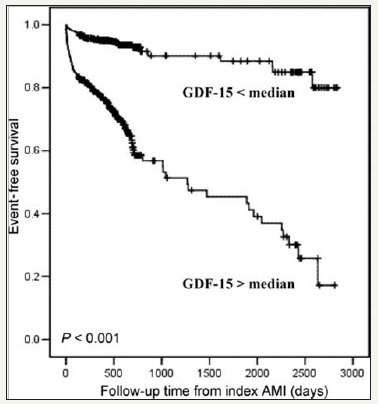
The relationship between the level of GDF-15 and cardiovascular outcomes has also been confirmed in 1,142 post-acute myocardial infarction patients - Figure 5 [12]. The increased level of GDF-15 was significantly related with all-cause mortality and HF hospitalization (P< 0.001), but not with reccurence of MI [12].
Figure 5:Kaplan–Meier survival curves event rate (death or heart failure) in patients grouped according to median levels of plasma GDF-15. (From [12])
Increased GDF-15 level has beneficial role during invasive strategy [13]. In the FRISC-II trial patients with GDF-15 level < 1200ng/L did not get any benefit from the invasive strategy even though they had ST segment depression or a troponin T level >0.01μg/L. Patients withGDF-15 levels >1200ng/L, especially those with 1800ng/L experienced significant (P< 0.001) reduction in the combined end point of death or MI by the routine invasive strategy [13]. Insights from cardiovascular magnetic resonance showed that elevated GDF-15 concentrations over and above the median on admission in 238 patients with STEMI undergoing PCI were a strong predictor of mortality (19 vs one death, P< 0.001) and major adverse cardiac events (27 vs nine events, P< 0.001) at 6 months follow-up [14].
Conclusion
Over the last 50 years biomarkers of myocardial injury, particularly cardiac troponin (cTn), creatine kinase and its isoenzyme creatine kinase myocardial band were commonly used for the diagnosis and making clinical decision in patients with suspected ACS. These established biomarkers are recently supplemented by novel indicators of myocardial necrosis which reflect inflammation, endothelial dysfunction, or hemodynamic stress. One of them is marker of biomechanical stress -GDF- 15. In this review, it was found that the elevated level of GDF- 15 correlates with risk of death from cardiac causes and other major cardiovascular complications and this relationship and this relationship has been strongly proven by numerous studies. Hopefully, in the future, the use of this marker in identifying and making therapeutic decisions in patients with ischaemic heart disease will be on the agenda.
References
- (1979) Nomenclature and criteria for diagnosis of ischemic heart disease. Report of the Joint International Society and Federation of Cardiol ogy/World Health Organization task force on standardization of clinical nomenclature. Circulation 59(3): 607-609.
- Alpert JS, Thygesen K, Antman E, Bassand JP (2000) Myocardial infarction redefined - a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 36(3): 959-969.
- Kempf T, Sinning JM, Quint A, Bickel C, Sinning C, et al. (2009) Growth-differentiation factor-15 for risk stratificationin patients with stable and unstable coronaryheart disease: results from the AtheroGene study. Circ Cardiovasc Genet 2(3): 286-292.
- Schopfer DW, Ku IA, Regan M, Whooley MA (2014) Growth differentiation factor 15 andcardiovascular events inpatients with stable ischemic heart disease (The Heartand Soul Study). Am Heart J 167(2): 186 -192. e1.
- Dallmeier D, Brenner H, Mons U, Rottbauer W, Koenig W, et al. (2016) Growth differentiation factor 15,its 12-month relative change, and risk of cardiovascularevents and total mortality in patients with stable coronaryheart disease: 10-year follow-up of the KAROLA study. Clin Chem 62(7): 982-992.
- Hagström E, Held C, Stewart RA, Aylward PE, Budaj A, et al. (2017) Growth differentiation factor 15 predictsall-cause morbidity and mortality in stable coronary heart disease. Clin Chem 63(1): 325-333.
- Wollert KC, Kempf T, Peter T, Olofsson S, James S, et al. (2007) Prognostic value of growth-differentiation factor-15 in patients with non-ST-elevation acute coronary syndrome. Circulation 115(8): 962-971.
- Kempf T, Björklund E, Olofsson S, Lindahl B, Allhoff T, et al. (2007) Growth-differentiation factor-15 improves risk stratification in ST-segment elevation myocardial infarction. Eur Heart J 28(23): 2858-2865.
- Hagström E, James SK, Bertilsson M, Becker RC, Himmelmann A, et al. (2016) Growth differentiation factor-15 level predicts major bleeding and cardiovascular events in patients with acute coronary syndromes: results from the PLATO study. Eur Heart J 37(16): 1325-1333.
- Bonaca MP, Morrow DA, Braunwald E, Cannon CP, Jiang S, et al. (2011) Growth differentiation factor-15 and risk of recurrent events in patients stabilized afteracute coronary syndrome: observations from PROVE ITTIMI 22. Arterioscler Thromb Vasc Biol 31(1): 203-210.
- Fuernau G, Poenisch C, Eitel I, deWaha S, Desch S, et al. (2014) Growth-differentiation factor 15 and osteoprotegerin in acute myocardial infarction complicated by cardiogenics hock: a biomarker substudy of the IABP-SHOCK II trial. Eur J Heart Fail 16(8): 880-887.
- Khan SQ, Ng K, Dhillon O, Kelly D, Quinn P, et al. (2009) Growth differentiation factor-15 as a prognosticmarker in patients with acute myocardial infarction. EurHeart J 30(9): 1057-1065.
- Wollert KC, Kempf T, Peter T, Olofsson S, James S, et al. (2007) Prognostic value of growth-differentiation factor-15 in patients with non-ST-elevation acute coronary syndrome. Circulation 115(8): 962-971.
- Eitel I, Blase P, Adams V, Hildebrand L, Desch S, et al. (2011) Growth-differentiation factor 15 as predictor ofmortality inacute reperfused ST-elevation myocardial infarction: insights from cardiovascular magnetic resonance. Heart 97(8): 632-640.
© 2018 Szymon Jonik. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






