- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Evolution in Adult Cardiac Surgery: Quo Vadis?
Marzia Cottini*
Department of Heart and Vessels, Cardiac Surgery Unit and Heart Transplantation Center, Niguarda Hospital, Italy
*Corresponding author: Marzia Cottini, Department of Heart and Vessels, Cardiac Surgery Unit and Heart Transplantation Center, Niguarda Hospital, 20162 Milan, Italy
Submission: August 03, 2017;Published: April 27, 2018

ISSN 2578-0204Volume2 Issue1
Abstract
From the cardiopulmonary bypass and first heart transplantation to transcatheter valve implantation and minimally invasive cardiac surgery, there were spent many decades. The cardiac surgery had modelled and evolved according to surgeons’ experience and clinical needs. Nowadays, the minimally invasive surgery and robotic surgery have won the first place in our operation rooms with the more and more emergent transcatheter valve procedure.
Keywords:Cardiac surgery; Minimally invasive surgery; Heart transplantation; Cardiac perspectives; Transcatheter valve
Introduction
For a young cardiac surgeon, it seems that every cardiac surgery procedure were discovered and tried but a more careful analysis could show the cardiac surgery is ever-changing science. From the last half of twentieth century, the cardiac surgery had emerged more and more and become important and reliable medicine discipline. We could indentified two era: before and after cardiopulmonary bypass (CPB). The first cases of cardiac surgery before CPB were dating to 1850-1900, when Dr Hale Williams and Dr. Rehn tried to treat stab wound of the heart. Afterwards, it had arrived the time of heart valve disease: Tuffier (1912), Souttar (1915) and Holmes/ Seller (1948) had done first clinical attempt to open a stentic aortic valve, successful of mitral finger commisurotomy and pulmonary valvulotommy, respectively. Only in the 1952. Hufnagel implanted the first valve in descending aorta.
Figure 1:The cardiac surgery development: the pre- Cardiopulmonary bypass (CPB) era; the CPB era and the advanced CPB era.
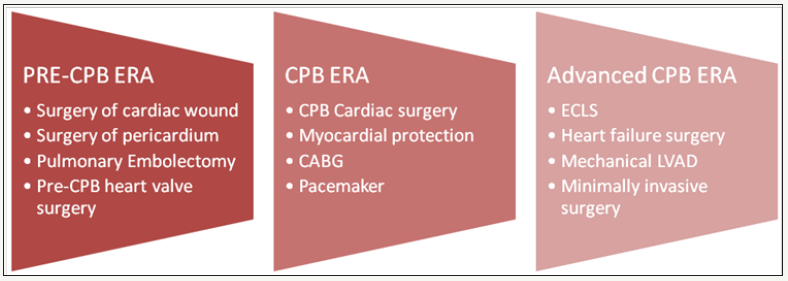
Hence, the cardiac surgery arrived to the a salient period of surgical growth and technological development: the era of CPB characterized by multiple milestones (Figure 1). Carrel and Lindbergh were the pioneers of the CPB and coronary bypass, they had started to create this circulatory support for cardiac surgery in the 1912. In parallel, Dr. Lillehei sought to find alternative circulating support (as cross circulation) to perform cardiac surgery procedure and Dr. Digliotti (Turin, 1950) used a heart-lung machine of his own design to partially support the circulation while he resected a large mediastinal tumor compressing the right side of the heart. We had waited Dr. Gibbon (1953-55), to see the first wellfunctioned heart-lung machine: form here, it was all an escalation of open-heart programs. In the 1953 Gordon performed the first coronary artery bypass using sections of mammary, axillary and carotid arteries to replace diseased left anterior descending artery [1]. Then Albert Starr (1960) had done the first successful orthotopic mitral valve replacement (Starr-Edwards ball valve), followed by Harken’s implantation in aortic position. On the one hand the devices and cardiac surgery procedure had become more and more, on the other side a smaller group of researches was discovering the mechanism of ischemia and perfecting cardioplegia and its solutions [2].
Moreover, the cardiac surgery didn’t stopped: after the conventional CPB period, it arrived the transition phase in which had been experienced multiple alternative to perform surgical procedure and had led to the minimally invasive surgery and hybrid era (Figure 2) [3,4]. In the 1972, it was performed the first extracorporeal life support (ECLS) to treat a 24 year-old man affected by shock lung after blunt trauma. The ECLS was an extension of CPB developed by membrane oxygenator and peripherical cannulation [5,6]. Between 1980 and 2000, there was the spreading of new surgical techniques and more and more technological device. Cardiac surgeons started to use minimally invasive surgery for valve disease and coronary artery bypass, to treat dilated or hypertrophic cardiomyopathy. The next step was the percutaneous valve: many patients with symptomatic severe aortic stenosis are not ideal candidates for surgery due to increased risks so first-in man pioneer was Dr. Alain Cribier who described the first human case of non surgical prosthetic valve implantation (2002). From 2002, the transcatheter valve implantation (TVI) emerged more and more, were used not only for aortic valve but all heart valve in the adult and in the children. The approaches of TVI were several from femoral to apical, aortic, axillary and carotid, and they were simpler and more and more available due to the technological and suitable devices [7].
Figure 2:The evolution of cardiac surgery to new minimally invasive techniques and robotic-surgery. PCI: Percutaneous Coronary Intervention; CAB: Coronary Artery Bypass; PM: Pacemaker

The cardiac surgery is ever-changing science: which would be the future perspectives?
Even if we could think “all was already discovered and done”, it was not so. There were a lot of surgeons and researches that try to increase the quality of biological prosthesis and compared the structure and adaptation of stented, stentless and sutureless valve to perform the best and faster valve implantation in minimally invasive surgery and to guarantee the best patient’s quality of life with longer prosthesis durability but less complications. Furthermore, it was developed alternative surgical strategy to avoid prosthesis implantation in particularly for mitral valve repair: percutaneous mitral valve repair or mitral clips or neochorda implantation procedure were examples of them. Currently, these procedure were limited to specific patients’ clinical conditions but they could become conventional procedure in the future.
The hybrid approach to coronary artery disease grew more and more in our experience: the treatment of culprit lesion with percutaneous coronary angioplasty then the completion of coronary revascularization or vice versa, were more and more frequent in our department and had significantly written the new era of collaboration between cardiac surgeon and cardiologist. In addition to what we have already described, we couldn’t forget the acute and chronic surgical therapy of heart failure (HF). HF continued to be ever-growing public health problem requiring a lot of public health efforts. Despite the evolution of medical drugs and the development of short-, mid- and long-term mechanical support, the HF was the Achilles’ heel of cardiac surgery. The basic and advance researches had offered multiple choices to treat HF and the technologies with the surgeons’ experience had increased survival and quality of life of HF patients. Otherwise, in the world of internet, travel to the space, cellular and molecular medicine, the heart transplantation (HTx) has still held the first place in the cardiac surgery for end-stage HF therapy. From the first case of heterotopic canine HTx described by Carriel and Guthrie to 1967 with the first human-to-human HTx performed by Barnard, from efforts of Shumway and colleagues to improve this procedure worldwide to the Caves’ genial idea of monitoring allograft rejection by transvenous endomyocardial biopsy (1973), from the advent of immunosuppressive agent which changed completely the survival of heart transplant patients (1981), the HTx procedure remained the same all over the world. These pioneers had written the best significant and reliable pages of cardiac surgery for end-stage HF, and the future of HTx would be enclosed in improvement of the quality of organ preservation, the more innovative immunosuppressive therapy, the new non invasive diagnostic exams, the genetic engineering techniques. Maybe the regenerating techniques for cardiomyocites and the reproduction in the laboratory of human tissues would fill the shortages of heartdonor- graft by lab creation. Only research, persistent work and belief would realize that project.
Human Rights Statements and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later revisions.
References
- Stephenson LW (2008) History of cardiac surgery. In: Surgery: Basic science and clinical evidence (2nd edn).
- Dominik J, Zacek P (2010) Heart valve surgery.
- Vinall M (2011) Minimally invasive cardiac surgery. Curr Probl Surg.
- Vanermen H (1998) What is minimally invasive cardiac surgery? J Card Surg.
- Faulkner SC, Taylor BJ, Chipman CW (2009) Mobile extracorporeal membrane oxygenation. Ann Thorac Surg.
- Combes A, Bacchetta M, Brodie D, Müller T, Pellegrino V (2009) Extracorporeal membrane oxygenation. Med J Aust.
- Cribier A, Eltchaninoff H, Bash A, Borenstein N, Tron C, et al. (2002) Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: First human case description. Circulation 106(24): 3006-3008.
© 2018 Marzia Cottini. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






