- Submissions

Full Text
Open Access Research in Anatomy
Late Repair of Bland-White-Garland Syndrome In a 67-Year-Old Man: How Late Is Too Late?
Dib N1*, Roubertie F1, Metras A1, Pinaquy JB3 and Iriart X2
1Congenital Cardiac Surgery Department, Bordeaux Heart University Hospital, France
2ongenital Cardiology Department, Bordeaux Heart University Hospital, France
3Radiology and diagnostic and interventional imaging department, Bordeaux Heart University Hospital, France
*Corresponding author: Dib Nabil, Congenital Cardiac Surgery Department, Bordeaux Heart University Hospital Haut Leveque, 1 avenue de Magellan 33604 Pessac, France
Submission: December 12, 2021 Published: February 04, 2022

ISSN: 2577-1922
Volume2 Issue4
Abstract
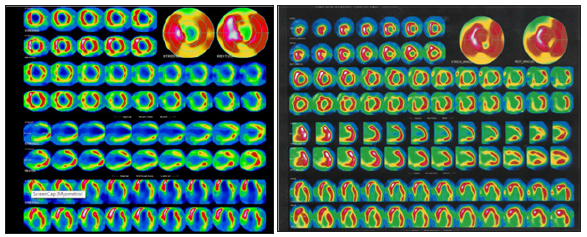
Background: An anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA) is an uncommon congenital anomaly associated with a high mortality rate within the first year of life. The rare adult patient who survives this anomaly usually presents with a moderate to severe ischaemia-induced systolic function impairment that raises the question of the risk-benefit balance of surgical correction. To assess this balance, advanced imaging modality is helpful to assess the potential postoperative recovery of the left ventricular myocardium by distinguishing between necrotic and viable myocardium. Case presentation: We report a case of late diagnosis of an abnormal connection of ALCAPA in a 67-yearold man. Preoperative scintigraphy assessed the myocardium status and found moderate to severe hypoperfusion of the anterior and inferior walls as well as the apex that was not reversible at rest. These sequences suggesting an apical, inferior and anterior necrosis (8 myocardial segments). Despite early postoperative assessment performed by transthoracic echocardiogram showed mild initial LV function improvement, scintigraphy performed at 3 years showed similar myocardial function to preoperative and a mild improvement on myocardial perfusion with 5 myocardial segments affected. Conclusion: Late diagnosis of ALCAPA in adults is rare and often associated with severely impaired LVEF due to chronic ischaemia. The risk-benefit balance of surgical decision-making in such complicated patients could be supported by a multiparametric approach including age, preoperative LVEF and advanced imaging modalities providing accurate data on myocardial perfusion to evaluate potential postoperative LV function recovery
Keywords:Bland-white-garland syndrome; Imaging; Congenital
Abbreviations: ALCAPA: Abnormal Left Coronary Artery From The Pulmonary Artery; LVEF: Left Ventricular Ejection Fraction; LGE: Late Gadolinium Enhancement; LV: Left Ventricular; MRI: Magnetic Resonance Imaging
Background
An anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA) is a rare congenital anomaly in children with a high mortality rate in the first year of life [1]. The creation of collateral networks from the right coronary artery allows survival of the rare adult patient [2].
Case Presentation
We report a case of late diagnosis of ALCAPA in a 67-year-old man, revealed by severe impairment of left ventricular (LV) systolic function on echocardiography, with a left ventricular ejection fraction (LVEF) of 35%, associated with paroxysmal atrial fibrillation and a recent cerebrovascular ischaemic stroke. Initial transthoracic echocardiogram (TTE) showed a severely dilated right coronary artery and absence of the left main coronary artery arising from the aortic root, associated with severe impairment of LV systolic function and moderate mitral regurgitation. The diagnosis of ALCAPA was further confirmed by multislice computed tomography (Figure 1A & 1B), and coronary angiography (Figure 2A & 2B). The patient underwent myocardial scintigraphy showing moderate to severe hypoperfusion of the whole anterior and inferior walls and the apex, not reversible at rest, suggesting a necrosis of 8 myocardial contiguous segments in the left coronary perfusion territory with significant impairment of LVEF (26%) (Figure 3A). We decided to operate on the patient and performed a reimplantation of the left coronary artery into the aorta using a short prosthetic conduit under cardiopulmonary bypass. Early postoperative assessment showed a rapid clinical recovery; early follow up showed progressive LV function improvement (LVEF 45%) on TTE, despite persistent septal hypokinesia. Mitral regurgitation was trivial at last TTE. However, three years post-operative myocardial scintigraphy showed the persistence of a significant LVEF impairment (30%) but with a better perfusion of the apical region (Figure 3B). Furthermore, anterior and inferior necrosis remained (5 myocardial contiguous segments).
Figure 1A and 1B:Multislice computed tomography shows the left coronary artery arising from the pulmonary trunk.
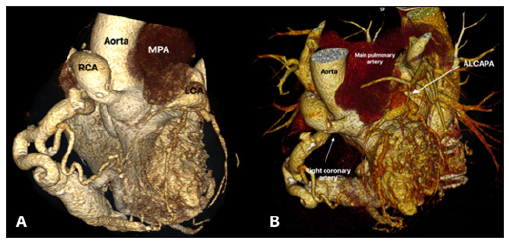
Figure 2:(A) Coronary angiography shows a large dilated and tortuous right coronary artery (RCA). (B) Left coronary artery delayed opacification due to collaterals from the RCA.
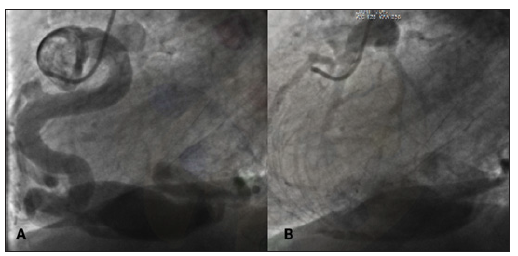
Figure 3:(A) Preoperative myocardial scintigraphy showing hypoperfusion of the anterior and inferior walls and the apex not reversible at rest. (B) Postoperative myocardial scintigraphy showing improved perfusion of the apex area.
Discussion
ALCAPA is part of the ischemic heart disease group. In a recent study focusing on the myocardial viability assessment, it was found that even noncontractile ischemic myocardial tissue can recover after revascularization but the main benefit is due to the protection from acute coronary events damage such as myocardial infarction [3]. MRI and myocardial scintigraphy are imaging techniques allowing an accurate segmental analysis of the myocardium state. These techniques allow to accurately assess the extent and location of areas of myocardial necrosis or hibernation. In addition, scintigraphy dynamically assesses the state of the myocardium by studying myocardial viability with the injection of Thalium. MRI with late gadolinium enhancement is able to give the state of the myocardium by differentiating between myocardial hibernation and necrosis whether transmural or subendocardial. This information allows an accurate preoperative myocardial assessment and helps us to predict postoperative myocardial recovery. If not, it helps us to orient the patient towards medical treatment alone and avoid the risks inherent to surgery. In a meta-analysis of more than 3000 patients [4], patients who underwent revascularization after myocardial viability was found on scintigraphy had a 79.6% reduction in the risk of death compared to medical treatment alone (p<0.0001). In contrast, on patients without myocardial viability found on scintigraphy, no significant difference in mortality was found between revascularized patients or those treated medically (p=0.23). In addition, clinical improvement is not proportional to the increasement of viable myocardial segment. In our case, although that the segmental myocardial perfusion in our patient was improved by surgical revascularization, clinical postoperative patient’s improvement isn’t clear. When LGE MRI or myocardial scintigraphy strongly suggests hibernating or viable myocardium rather than necrosis, segmental improvement of LV function supporting surgical management rather than a conservative medical approach can be expected [4]. Otherwise, as in our case, surgery seems less obvious for myocardial recovery when the state of myocardial necrosis is established.
Conclusion
The benefit-risk balance of surgical revascularization in adult ALCAPA patients could be supported by myocardial perfusion analysis to assess the recovery of potential postoperative left ventricular myocardial function and thus avoid operative risk.
References
- Fannschmidt JP, Ruskowski H, De Vivie ER (1992) Das Bland-White-Garland-Syndrome. 204: 328–334.
- Edwards JE (1964) The Direction of Blood Flow in Coronary Arteries Arising from the Pulmonary Trunk. Circulation XXIX: 163–166.
- Panza JA, Chrzanowski L, Bonow RO (2021) Myocardial Viability Assessment Before Surgical Revascularization in Ischemic Cardiomyopathy: JACC Review Topic of the Week. J Am Coll Cardiol 78(10): 1068–1077.
- Allman KC, Shaw LJ, Hachamovitch R, Udelson JE (2002) Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol 39(7): 1151–1158.
© 2022 Dib N. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






