- Submissions

Full Text
Open Access Research in Anatomy
Primary Giant Cell Tumour of Soft Tissue in Scalp: An Uncommon Tumour at Uncommon Location
Khairul Shakir A1, Ikmal Hisyam B2*, Mathaneswaran R1, Usman S1, Hasni M2, Ali Ajemi3, Asrul Fahmi A3 and Wan Irnawati4
1Department of Pathology, Hospital Tuanku Fauziah, Malaysia
2Department of Pathology, Faculty of Medicine and Health Sciences, Malaysia
3Department of Orthopaedic, Hospital Tuanku Fauziah, Malaysia
4Department of Radiology, Hospital Tuanku Fauziah, Malaysia
*Corresponding author: Ikmal Hisyam B, Department of Pathology, Faculty of Medicine and Health Sciences, Malaysia
Submission: May 30, 2018 Published: September 29, 2021

ISSN: 2577-1922
Volume2 Issue 4
Abstract
Primary Giant Cell Tumour of Soft Tissue (GCT-ST), also known as soft tissue giant cell tumour of low malignant potential, is a rare soft tissue tumour. Histologically, these lesions bear a close resemblance to their bony counterparts, GCT of bone. Although predominantly a benign condition, its capacity to recur or evolve into malignant lesion is well recognized. The lesions are usually superficial and involve lower extremities and trunk but rarely occur in head and neck. Here we report a rare benign primary GCT-ST at an uncommon location. A 27-year-old Malay gentleman presented with painless right forehead swelling for three months. Physical examination revealed a mobile, benign looking superficial skin lesion measuring 3x1cm. Grossly, the lesion showed greyish solid surface enwrapped by thin pseudo-capsule. Microscopically, it composed of round to oval mononuclear cells intermixed with osteoclast-like giant cells. The mononuclear cells displayed mildly pleomorphic vesicular nuclei with small nucleoli and moderate amount of cytoplasm. Mitotic figures were frequent, but no atypical form was observed. The neoplastic cells were weak and diffusely expressing SMA. Homogenous and strong expression of CD68 was noted on the osteoclast-like giant cells. GCT-ST is an uncommon but distinct entity. It is important to recognise this pathological entity in order to avoid misdiagnosis with other fibrous tumour associated with giant cells such as GCT of tendon sheath, nodular fasciitis, benign fibrous histiocytoma and undifferentiated pleomorphic sarcoma. Complete excision with negative margins results in benign clinical course because distant metastasis and tumour-associated death seem to be exceedingly rare.
Keywords:Giant cell tumour; Soft tissue; Scalp; Uncommon location
Introduction
Primary Giant Cell Tumour of Soft Tissue (GCT-ST), also known as soft tissue giant cell tumour of low malignant potential, is a rare slow-growing soft tissue tumour. Histologically, these lesions bear a close resemblance to their bony counterparts, giant cell tumour of bone, consists of two main cell types of mononuclear stromal cells and multinucleated giant cells of the osteoclastic type. Although GCT-ST is predominantly a benign condition, its capacity to recur or evolve into malignant lesion is well recognized. The lesions are usually superficial and involve lower extremities and trunk but rarely occur in head and neck. Here we report a rare benign primary GCT-ST at an uncommon location (scalp) in a 27year-old male.
Case Report
A 27-year-old Malay gentleman presented with painless, slow growing right forehead swelling for three months. The lesion was not associated with traumatic event or insect bite. On physical examination, there was a mobile, benign looking superficial skin lesion measuring 3x1cm. A diagnosis of sebaceous cyst was made, and he was posted for excisional biopsy under local anaesthesia. Intraoperatively, the lesion was well encapsulated, and the excisi was complete. Grossly, the lesion was greyish in colour and has smooth external surface. It measured 20x9x6mm. On cut opening, the lesion has greyish solid surface enwrapped by thin pseudocapsule. There was no areas of necrosis or haemorrhage present.
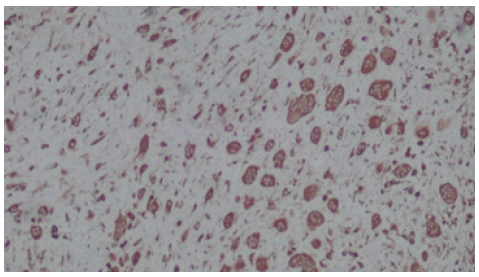
Microscopic examination of the lesion using Hematoxylin and Eosin (H&E) stain showed a well circumscribed but encapsulated tumour. It composed of round to oval mononuclear stromal cells intermixed with capillary-sized blood vessel networks (Figure 1). The neoplastic mononuclear stromal cells were mildly pleomorphic with vesicular nuclei, a single small nucleoli and moderate amount of cytoplasm (Figure 2). Mitotic figures were frequent, but no atypical form was observed (19 in 10 high power fields). Osteoclast-like giant cells were also seen, intimately associated with the neoplastic cells (Figures 1&2). Osseous metaplasia was occasionally present in areas. The neoplastic cells were weak and diffusely expressing Smooth Muscle Actin (SMA) (Figure 3). Homogenous pattern and strong expression of CD68 was noted on the osteoclast-like giant cells (Figure 4).
Figure 1:The lesion composed of round to oval mononuclear stromal cells intermixed with capillary-sized blood vessels. Scattered osteoclast-like giant cells are visible at this magnification (Hematoxylin and eosin stain, original magnification x100).
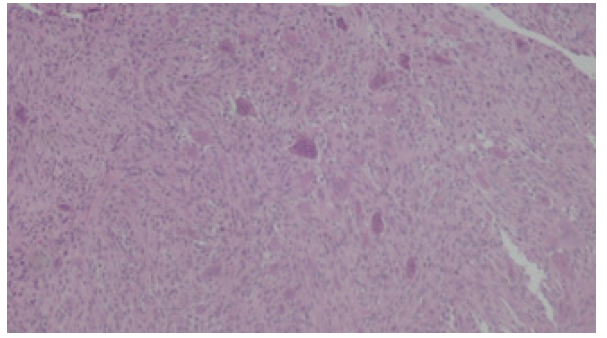
Figure 2:The neoplastic cells displayed mildly pleomorphic vesicular nuclei with a single small nucleoli and moderate amount of cytoplasm. Osteoclast-like giant cells were intimately associated with the neoplastic mononuclear stromal cells (Hematoxylin and eosin stain, original magnification x 400).
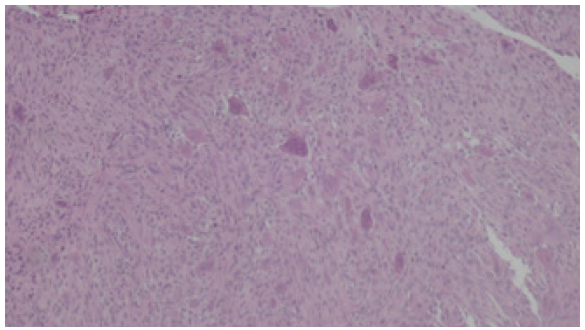
Figure 3:The neoplastic mononuclear stromal cells were weak and diffusely expressing SMA (Immunohistochemical stain, original magnification x 100).
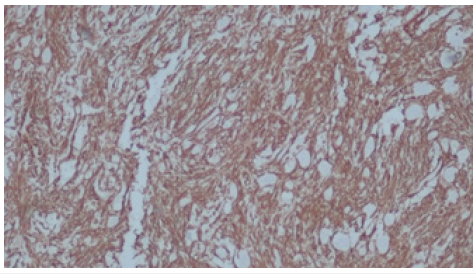
Figure 4:Homogenous pattern and strong expression of CD68 is noted on the osteoclast-like giant cells (Immunohistochemical stain, original magnification x 100).
Discussion
Primary Giant Cell Tumour of Soft Tissue (GCT-ST) is an uncommon, slow-growing soft tissue tumour but with distinct entity [1,2]. It was first described by Salm and Sissons in 1972 and later followed by Guccion and Enzinger [2]. Recently, Alpana C et al. [3] and Flope et al. [4], proposed the term of giant cell tumour of low malignant potential because of its capacity to recur. In the study, four out of 19 patients developed tumour recurrence (mean 3 years and median 1-7years) but none has developed distant metastasis [4].
Epidemiologically, it GCT-ST has a wide range of age at presentation (between 5 to 80 years old), but usually occur at the age of 40 years old and above [5]. There is no gender predilection even though a few authors reported that females are more effected than males (3:2) [3]. In majority of the cases, the most common presentation is painless growing mass between two to 12 months duration. The lower limbs were the most common site (50%), followed by the trunk (31.8%) and the upper limbs (13.6%) [5]. Tumour location at lip, head and neck is exceedingly rare [2,3]. The tumour size ranged from 1 to 10cm and usually superficially located, forming well circumscribed and multinodular masses [3,5].
GCT-ST is similar to GCT of bone histologically and phenotypically [1,5-7]. It consists of a mixture of mononuclear stromal cells showing vesicular, rounded to oval nuclei admixed with osteoclastlike multinucleated giant cells with similar nuclei [5,6,8]. Stromal haemorrhage, metaplastic bone formation and aneurismal bone cyst-like areas are occasionally identified. Necrosis is rarely seen. Mitotic figures as high as 30 mitoses per 10 high power fields can be present but abnormal mitosis is always absent. Vascular invasion is also not uncommon [3,5]. It lacks nuclear atypia or pleomorphism even though GCT-ST with nuclear atypia had been reported [1,5].
Immunohistochemical study is usually not performed and not necessary for diagnosis. The tumour exhibits strong positive immunoreactivity for CD68 within the multinucleated osteoclast like giant cell [9]. The mononuclear stromal cells express SMA, Tartrate-Resistant Acid Phosphatase (TRAP), vimentin and CD68, but lack CD45, S100, desmin and lysozyme [4].
The possible differential diagnoses include soft tissue tumour rich in giant cells such as GCT of tendon sheath, nodular fasciitis, benign fibrous histiocytoma, plexiform fibro histiocytic tumour and undifferentiated pleomorphic sarcoma with giant cells [2]. GCT of tendon sheath usually has heterogeneous population of cells including xanthoma cells, siderophages and lymphocytes. Giant cell form of undifferentiated pleomorphic sarcoma by definition should have significant level of nuclear atypia including atypical mitosis and necrosis. GCT-ST is differentiated from fibro histiocytic tumour by the bimodal population of cells [9].
The treatment of choice for GCT-ST is complete surgical excision. Several studies have been conducted to demonstrate the role of bisphosphonates (zoledronic) as a potentially attractive therapy, to reduce osteoclast activity and control tumour growth [10].
Conclusion
It is important to recognise this pathological entity in order to avoid misdiagnosis with other fibrous tumour associated with giant cells. Complete tumour excision with negative margins of GCTST results in a benign clinical course because episodes of distant metastasis and tumour-associated death seem to be exceedingly rare.
Acknowledgement
The authors would like to thank the Director of Health Malaysia for permission to publish this paper. The authors declare that there is no conflict of interest to disclose.
References
- O'Connell JX, Wehrli BM, Nielsen GP, Rosenberg A (2000) Giant cell tumors of soft tissue: A clinicopathologic study of 18 benign and malignant tumors. Am J Surg Pathol 24(3): 386-395.
- Bandyopadhyay A, Khandakar B, Medda S, Soumit D, Chandra P (2015) Giant cell tumour of soft tissue in neck: An uncommon tumour in an uncommon location. J Clin Diagn Res 9(12): ED19-20.
- Alpana C, Alok C, Rakesh K, Anjali J (2016) Cystohistological diagnosis of soft tissue giant cell tumour of neck-A rare presentation. International Archives of Integrated Medicine 3(8): 283-285.
- Folpe AL, Morris RJ, Weiss SW (1999) Soft tissue giant cell tumor of low malignant potential: A proposal for the reclassification of malignant giant cell tumor of soft parts. Mod Pathol 12(9): 894-902.
- Oliveira AM, Dei Tos AP, Fletcher CD, Nascimento A (2000) Primary giant cell tumor of soft tissues: A study of 22 cases. Am J Surg Pathol 24(2): 248-256.
- Holst V, Elenitsas R (2001) Primary giant cell tumor of soft tissue. J Cutan Pathol 28(9): 492-495.
- Lau YS, Sabokbar A, Gibbons CL, Henk G, Nicholas A (2005) Phenotypic and molecular studies of giant-cell tumors of bone and soft tissue. Hum Pathol 36(9): 945-954.
- Rodriguez J, Lopez F, Fernandez J (2001) Primary giant cell tumor of soft tissues similar to bone giant cell tumor: A case report and literature review. Pathol Int 51(1): 60-63.
- Kulkarni MM, Joshi AR, Patil V, Tabassum A (2016) Giant cell tumor of soft tissues of low malignant potential: A rare diagnosis on fine needle aspiration cytology. J Cytol 33(2): 106-108.
- Clézardin P (2005) Anti-tumour activity of zoledronic acid. Cancer Treat Rev 31(Suppl 3): 1-8.
© 2021 Ikmal Hisyam B. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






