- Submissions

Full Text
Novel Techniques in Nutrition and Food Science
Health Education in Schools
Nawal Alissa*
Department of Food Science, USA
*Corresponding author: Nawal Alissa, Department of Food Science, USA
Submission: June 16, 2020;Published: July 21, 2020

ISSN:2640-9208Volume5 Issue1
Mini Review
The United States youth faces the overwhelming issues of rapidly increasing childhood obesity, substance abuse, and teen birth rates that can affect a youth’s future endeavors and successes. Students are often taught the basics of health in schools, but these issues go far beyond their basic knowledge and require health education to be taught in schools. One of the facets of health education is to combat obesity. Teaching students about a healthy diet and reinforcing healthy conceptions of body image can avoid childhood obesity and eating disorders. Because adolescence is one of the most influenceable times in a person's life, health education during this time often is well-received and suitable. Moreover, schools are a logical site for prevention because children spend 6-8 hours a day there during most of the year [1]. If schools implemented health education and developed ways to encourage students to include healthy lifestyle decisions, proper nutrition, and exercise into their regular daily activity, then childhood obesity levels would decrease significantly [1]. For example, children would have the opportunity to take health educational materials home where their parents would then have the chance to see the content, and would hopefully take action to be a part of the program as well as make better decisions not only for their child, but for the entire family.
The percentage of children aged 6-11 years in the United States who were obese increased from 7% in 1980 to nearly 18% in 2010 [2]. Twenty-five percent of children in the US are overweight and 11% are obese [3]. According to the CDC, “childhood obesity has more than doubled in children and quadrupled in adolescents in the past 30 years. In 2012, more than one third of children and adolescents were overweight or obese” [4]. The two leading protective factors for childhood obesity include adequate physical activity and proper nutrition [5]. Yet, the issue of childhood obesity has been an increasing problem for over thirty years with no relief in sight. For that reason, is the U.S. government actually required to mandate health education in schools to address childhood obesity?
Figure 1: Obesity and overweight rates for children ages 2 to 19, NHANES by gender and race [11].
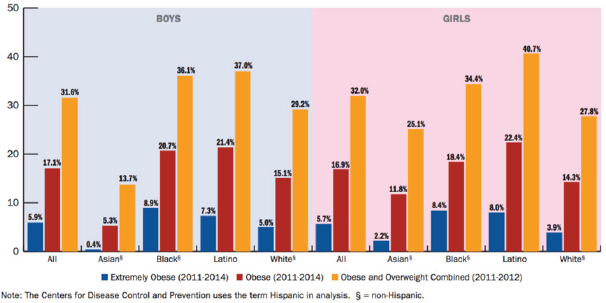
The government has the opportunity to utilize the schools to directly change the lifestyles and food choices children are making (Figure 1). Through health education in schools, lesson plans will focus on the protective nutrition factor for children. School teachers should have the opportunity to educate children about the importance of making healthy decisions and how eating healthy can make a difference in their lives.
Students already have preferences in food choices, but they are still willing to change in response to positive reinforcement by health [6]. Students in a developmental period during which health educators have an important influence on a student’s health behaviors and attitudes. Thus, health educators play an essential role in guiding the eating habits, weight status, and body image of the students [7]. The strategy of involving nutrition in the health education is based on providing the students with knowledge and skills that lead to increase their healthy lifestyles and decrease the risk of obesity. For example, a tool that the United States Department of Agriculture has attempted to use, but has continuously changed, is the MyPlate program. The goal of the MyPlate initiative is to teach students about healthy eating, weight management, physical activity, and healthy lifestyles [8]. Therefore, providing health education in schools provides the appropriate information for the students regarding healthy food choices to promote healthy eating lifestyles and forming healthy habits, thus combat childhood obesity as well as future adult obesity.
Sex Education is another facet of health education. Adolescents are bombarded with new information, inaccurate, unrealistic media messages on sexuality, specifically about sexual performance, making sexual approaches and gay or lesbian issues [9]. How can they know what is accurate information, what is relevant, and how to make healthy decisions? Health education is the way to develop health-literate youth who understand sexuality and use personal and social skills to make healthy decisions in their lives.
Adolescents under pressure to be sexually active and with earlier sex, more sex, and peer pressure, they are challenged to make decisions and cope with their sexuality [9]. In 2014, a total of 249,078 babies were born to women aged 15-19 years [4]. Only 1 in 4 (27%) teens ages 15 to 17 have ever had sex [4]. Health education develops an adolescents’ knowledge and understanding about contraceptive and STI prevention that meet the needs of teens (Figure 2).
Figure 2:
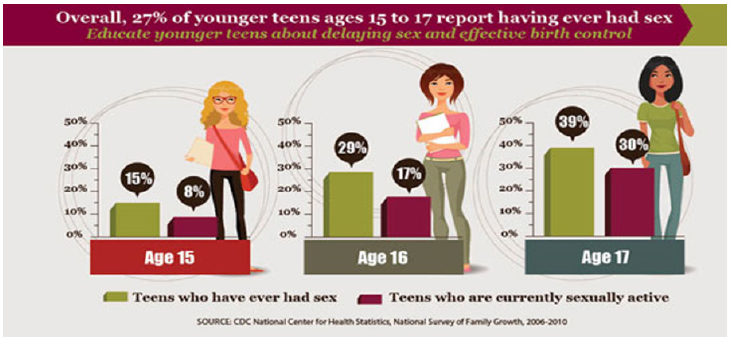
Tupper [10] indicated that when young people reach puberty, they are adapting to new biological, psychological and social roles with a lack of information, knowledge and support. Accurate sex education including information about contraception and teaching teens about the risks of pregnancy, sexually transmitted diseases and the emotional aspects of sexual relationships can help them shape a healthy outlook regarding sex. The elements of sex education curricula include for example methods of contraception, the types of STDs that can occur without proper protection and resources to deal with unwanted pregnancy. Adolescents need to receive accurate and relevant information to develop as individuals and independent sexual decision-makers.
Health education focuses on emotional, mental and social health. Other facets of health education include stress management, dealing with social relationships, and peer pressure. Educating students on the importance of being emotionally and socially healthy builds their motivation. As a result, they strive to maintain good health and avoid risky behaviors such as substance abuse. Instilling the importance of emotional health in schools, helps students to make healthy life choices and strive off risk relationships. It helps them understand the dangers of using illicit drugs, smoking and drinking alcohol. According to CDC, alcohol is the most commonly used and abused drug among youth in the United States [11]. Moreover, excessive drinking is responsible for more than 4,300 deaths among underage youth each year and costs the U.S. $24 billion in economic costs in 2010 [4]. The prevalence of marijuana among persons aged 12-17 years increased from 6.7% in 2006 to 7.1% in 2013 [4]. More than 3.6 million youths under the age of 18 are current daily smokers [4]. There is a need of raising the level of consciousness of self through proper education. Alcohol and drug addiction among youths can be prevented if the youth are taught of its harmful consequences. The young people must be aware of the harmful effects of alcohol and drug abuse. Hence, health education if required at schools, can become the most successful method to reduce and alleviate the problem of alcohol and drug addiction among youth. More than 3.6 million youth under the age of 18 are current daily smokers [11].
If health education is not required in schools, students will not receive the health information they need to build their knowledge and skills to make healthy decisions [12]. The students will not learn about healthy food choices to make healthy food choices to avoid unhealthy dietary habits and thus obesity and diabetes. Without health, students will learn to be proactive rather than to reactive to deal with health issues.
References
- Budd G, Volpe S (2006) School-based obesity prevention: Research, challenges, and recommendations. Journal of School Health 76(10): 485-495.
- Ogden CL, Carroll MD, Kit BK, Flegal KM (2012) Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA 307(5): 483-490.
- Dehghan M, Danesh NA, Merchant AT (2012) Childhood obesity, prevalence and preventions. African Journal of Food, Agriculture, Nutrition & Development 12(2): 1-16.
- Centers for disease control & prevention (2016) Preventing pregnancies in younger teens.
- Centers for disease control and prevention (2013) Childhood Obesity Facts.
- Parental influence on children’s food preferences and energy intake (2009) Obesity-genetic and environmental.
- Davison KK, Jurkowski JM, Li K, Kranz S, Lawson HA (2013) A childhood obesity intervention developed by families for families: results from a pilot study. Int J Behav Nutr Phys Act 10(1): 1-11.
- USA Department of Agriculture (2014).
- Caplan DM (2013) Schools, sex education, and support for sexual minorities: exploring historic marginalization and future potential. American Journal of Sexuality Education 8(4): 246-273.
- Tupper KW (2014) Sex, drugs and the honour roll: The perennial challenges of addressing moral purity issues in schools. Critical Public Health 24(2): 115-131.
- Centers for disease control & prevention (2016) Fact sheets-underage drinking.
- Centers for disease control & prevention (2014) Childhood obesity facts.
© 2020 Nawal Alissa. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






