- Submissions

Full Text
Novel Research in Sciences
High Sensitivity Troponin and Left Ventricular Function in The Clinical Course of Takotsubo Syndrome (TTS)
Abanador-Kamper N1*, Klostermeier M2, Nadem-Boueini N3, Seyfarth M1, Haage P3, Kamper L3
1Cardiology & Heart Center, HELIOS University Hospital Wuppertal, Germany
2Faculty of Health, Germany
3Diagnostic & Interventional Radiology, HELIOS University Hospital Wuppertal, Germany
*Corresponding author:Abanador- Kamper, Cardiology & Heart Center, HELIOS University Hospital Wuppertal, University Witten/Herdecke, Germany
Submission: January 29, 2023;Published: February 07, 2023
.jpg)
Volume13 Issue4February , 2023
Abstract
Takotsubo Syndrome (TTS) is a disease mainly affecting female patients that leads to an acute leftventricular dysfunction. TTS presents like an acute myocardial infarction, however in contrast to acute coronary syndromes coronary perfusion is inconspicuous. Specific biomarker for the diagnosis of TTS are lacking and classical myocardial laboratory parameters cannot discriminate TTS from acute coronary syndromes in the acute setting. Diagnosis bases on exclusion of an underlying coronary culprit lesion and classical left ventricular imaging findings. Aim of the present study was the analyses of myocardial biomarkers including high- sensitivity troponin T (hs-TnT) and the follow-up of left ventricular function in TTS compared to ST-elevation myocardial infarction.
Methods: We included 79 patients with TTS and 85 patients with ST-Elevation Myocardial Infarction
(STEMI). Myocardial laboratory parameters including hs-TnT were analysed for both groups and we
assessed left-ventricular Ejection Fraction (EF) in the acute setting and three months follow-up by
cardiovascular MRI.
Results: We observed significantly lower levels for hs-TnT (TTS: 328pg/ml vs. STEMI: 2544 g/ml; p<0.001)
and CK-MB (TTS: 33.5U/l vs. STEMI: 151U/l; p<0.001) in TTS patients. A cut-off value of 1131pg/ml
achieves a sensitivity of 100 and specificity 95.9% for the discrimination between TTS and STEMI in our
patients. TTS patients showed a lower left-ventricular EF in the initial assessment (EF: 50%) compared to
STEMI (EF: 57%). After 6 months we observed a significant improvement in TTS (EF: 65.5%) with only a
slightly recovery in STEMI patients (EF: 60%).
Discussion: In our population, we observed lower peak values for hs-TnT and CK-MB in TTS compared
to STEMI. A cut-off value may be able to differentiate TTS and STEMI in context of clinical and diagnostic
findings with optimal sensitivity in females. Initially reduced left ventricular function in TTS showed a
significant greater recovery compared to STEMI patients.
Abbreviations:TTS: Takotsubo Syndrome; CMRI: Cardiovascular Magnetic Resonance Imaging; STEMI: ST- Elevation Myocardial Infarction ; ACS: Acute Coronary Syndromes; LGE: Late Gadolinium Enhancement; LV-EF: Left-Ventricular Ejection Fraction; eGfr: Estimated Glomerular Filtration Rate; SD: Standard Deviation, IQR: Interquartile Range; ROC: Receiver Operating Characteristic; FU-1: First Follow Up
Introduction
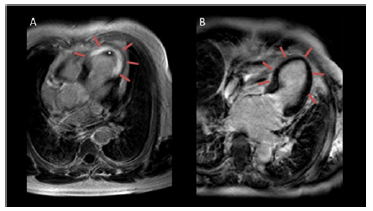
Takotsubo Syndrome (TTS) is an acute, usually reversible heart failure predominantly affecting postmenopausal women with an increasing incidence [1]. Sato and Dote described the disease as an independent entity in the 1990’s [2]. Characteristic finding is the ampulla shaped left ventricle with a round bottom narrow neck in end-systolic imaging, referred to as apical ballooning [3]. The name Tako-Tsubo derives from a Japanese octopus trap that resembles this distinctive left ventricular morphology [4]. Cardiovascular Magnetic Resonance Imaging (CMRI) is an excellent imaging modality for the visualisation of the specific left ventricular morphology in TTS [5] (Figure 1). Stress-induced catecholamine peaks are highly suspicious as pathophysiologic stimulus [5], usually associated with as specific occasion, like illness or death of a close person [4]. TTS is responsible for about two percent of all Acute Coronary Syndromes (ACS) [6]. TTS and ST- Elevation Myocardial Infarction (STEMI) share initial clinical features like chest pain, ECG changes and elevated biomarkers [5]. Therefore, the diagnosis is still challenging. It bases on coronary angiography without a culprit lesion together with apical ballooning in cardiovascular imaging [5]. A recent systematic review failed to identify further specific biomarker for acute or chronic TTS [1]. Aim of this study was to evaluate hs-TnT levels and left-ventricular function in patients with TTS compared to STEMI.
Figure 1:Subendocardial LGE (arrows in A) in a patient
with STEMI (A) due to LAD occlusion and additional
left ventricular thrombus (*). Absent myocardial LGE in
Takotsubo syndrome
(B) together with significant left-ventricular “apical
ballooning” (arrows in B).
Methods
Study design and population
We retrospectively examined data from 79 patients with TTS. A group of 85 STEMI patients served as control-group. TTS patients were examined from June 2009 to December 2018 and control group from May 2016 to December 2018. We documented classical cardiovascular risk factors like diabetes, arterial hypertension, smoking, dyslipidaemia, obesity, and family history of myocardial infarction for each patient.
The TTS group included patients older than 18 years, with angiographic exclusion of coronary artery disease and typical CMR findings, according to the diagnostic criteria of the “ESC Consensus Document” on Takotsubo syndrome [4]. The control group comprised patients with first STEMI due to an identifiable culprit lesion with impaired pre-interventional coronary flow defined by TIMI III flow and successful coronary intervention resulting in post-interventional TIMI II-III flow. Exclusion criteria included cardiogenic shock or other disease-related protocol violation, history of previous myocardial infarction or cardiac bypass surgery and general CMR contraindications. All patients gave their written consent for study participation and the local ethics committee approved the study.
Cardiac imaging
All patients received coronary angiography and CMR assessment. CMR examinations were performed after a median of one day (IQR: 2) after percutaneous coronary angiography for the TTS patients and a median of two days (IQR: 2) after percutaneous coronary intervention for the STEMI group. Complete data for the interval between coronary angiography (TTS group) or intervention (STEMI group) and the CMR examinations together with the follow-up periods are given in (Table 1). CMR protocol included left-ventricular function, wall motion analysis and tissue characterization including myocardial oedema assessment and myocardial necrosis detection, known as Late Gadolinium Enhancement (LGE). Imaging data were evaluated with a dedicated software tool (CMR42, Version 5.1.4.2, Circle Cardiovascular Imaging Inc., Calgary, Canada). We calculated left-ventricular function with a standard steady state free precession technique (2D turbo gradient echo sequence) in short axis, four-chamber, two-chamber and three-chamber views of the left ventricle. Left-Ventricular Ejection Fraction (LV-EF) and left-ventricular parameters were calculated by assessment of the volumes of the endocardial contours in diastole and systole of the four- and two-chamber slices [7]. We documented typical leftventricular wall motion abnormalities as apical, mid-ventricular or basal ballooning. The follow-up CMR examinations comprised applied identical sequence parameters.
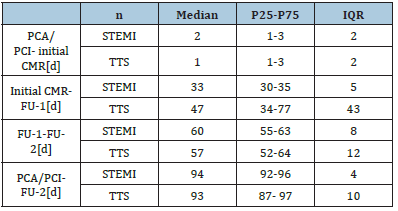
Table 1:Time periods for the patients with ST-Elevation Myocardial Infarction (STEMI), Takotsubo Syndrome (TTS). Data represented as median values with lowerupper quartile and interquartile range (IQR). Percutaneous Coronary Angiography (PCA), Percutaneous Coronary Intervention (PCI), CMR (Cardiovascular MRI), Follow-Up (FU)
Laboratory and clinical parameters
Routine emergency blood samples were taken at the time of hospital admission and in the follow-up until their normalization. We analysed CK, CK-MB, hs-TnT, Creatinine, Estimated Glomerular Filtration Rate (eGFR after CKD-EPI-Formula). Hs-Troponin T was analysed with Elecsys® on cobas e411® (Roche Diagnostics, Basel, Switzerland). CK and CK-MB were analysed based on kinetic procedure on cobas 6000® c501 (Roche Diagnostics Basel, Switzerland). Creatinine was measured according to Jaffé on cobas 6000®. We documented initial and peak values of all laboratory parameters whenever available. Every patient received a 12-channel ECG on hospital admission and during the follow-up.
Statistics
Categorical variables were described by frequencies (number, %). Laboratory parameters and left ventricular EF were described by mean, Standard Deviation (SD), median, lower and upper quartile (P25, P75) and Interquartile Range (IQR). For patients age we used mean values with standard deviations. Fisher’s exact test was used to test for independence between two categorical variables. Whether the mean of laboratory parameters and left ventricular EF of two groups were different was tested by two-sample t-test. Initial mean EF and mean EF at follow-up assessments were compared by one sample t-test. We conducted linear regression adjusted for baseline values to compare the mean difference of initial EF to follow-up of STEMI and TTS patients. Receiver Operating Characteristic (ROC) analysis was used to assess the effectiveness of hs-TnT and the ratio of hs-TnT and CK-MB max to classify patients into those with diagnose STEMI and those with diagnose TTS. Area under curve with 95% confidence intervals were calculated and ROC curves plotted. All statistical tests were two-sided at a significance level of 0.05. Statistical analysis was performed using Stata/IC 16.1 for Unix.
Table 2:Demographic and clinical data for the patients with ST-Elevation Myocardial Infarction (STEMI), Takotsubo Syndrome (TTS) and the TTS subgroup with ST-elevation (TTS-TS). Hypertension (HTN), Diabetes (DM), Hyperlipidemia (HLP), Coronary Artery Disease (CAD), Left Artery Descending (LAD), Right Coronary Artery (RCA), Ramus Circumflex Artery (RCX)
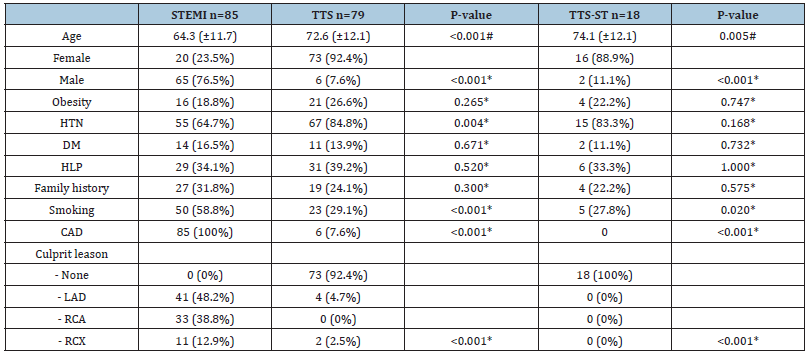
Source: *exact Fisher-Test, # two sample t-test
The resulting cohort comprised 79 TTS patients and 85 STEMI patients. We observed significant differences for age, gender, hypertension, smoking and known coronary artery disease (Table 1). All STEMI patients had a significant ST-elevation. In addition, a subgroup of 18 TTS patients also showed significant ST-elevation in the initial ECG (TTS-ST), with similar demographics compared to the general TTS group, only without significant differences for hypertension compared to the STEMI patients [8] (Table 2). Further ECG changes included T- wave changes (84.6% TTS vs. 50% STEMI), with an inverted T-wave in 73% of the TTS patient as the most common T-waves change. Coronary angiography revealed detectable culprit lesions in six TTS patients (7.6%) compared to 84 patients (98.8%) in the STEMI group, however culprit lesion affection in these six patients was a maximum of 50% stenosis without vascular total occlusion. Furthermore distinctive wall motion abnormalities did not suit affected coronary territory. Coronary culprit lesions were excluded for all patients of the TTSST subgroup (Table 2).
Laboratory findings
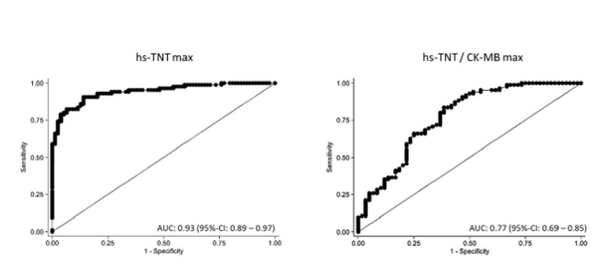
Resulting laboratory parameters are listed in (Table 3). Median values for hs-TnT were significantly higher in STEMI patients (Figure 2) compared to TTS (2544pg/ml. vs.328pg/ml) and compared to TTS-ST patients (2544pg/ml. vs. 504pg/ml). CK-MB values showed also significant differences, with higher median values in the STEMI group compared to TTS (151.0U/l vs. 33.5U/l) and compared to TTS-ST (151.0U/l vs. 42.0U/l). Hs-TnT values higher than 841pg/ml were able to distinguish between TTS and STEMI with a sensitivity of 90.6% and specificity of 86.1%. In an exclusive analysis of female patients a cut-off value of 1131pg/ml achieves even higher results with a sensitivity of 100 and specificity 95.9%. The analysed ratio of maximum hs-TnT and CK-MB was significantly higher in STEMI patients compared to both TTS groups (Table 3). ROC analysis for the diagnosis of STEMI revealed a greater area under the curve by the uses of maximal hs-TNT values alone compared to a quotient of hs-TNT/CK-MB max (Figure 3). Maximum and minimum values for the estimated eGFR did not differ significantly between all patient groups (Table 3).
Table 3:Laboratory results for the patients with ST-Elevation Myocardial Infarction (STEMI), Takotsubo Syndrome (TTS) and the TTS Subgroup with ST-elevation (TTS-TS). Standard Deviation (SD), lower and upper quartile (P25, P75), Interquartile Range (IQR), Estimated Glomerular Filtration Rate (eGFR), High-Sensitivity Troponin T (hs-TNT). Glomerular Filtrationrate (GFR), Creatinine Kinase (CK)
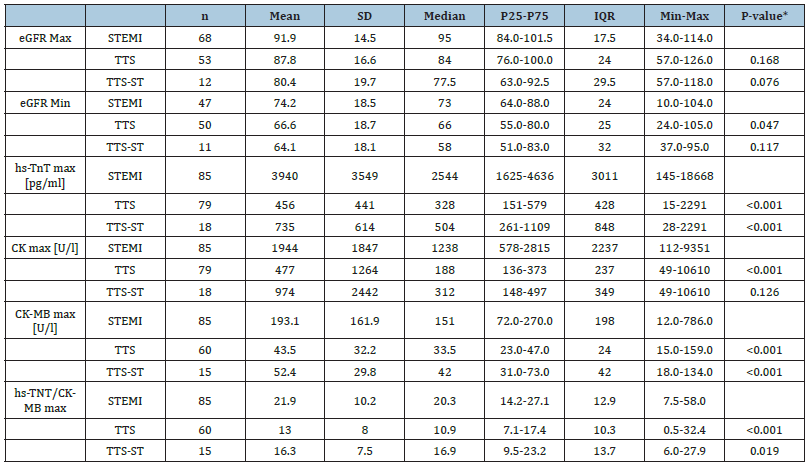
Source: *two sample t-test
Figure 2: Maximum High-Sensitivity Troponin T (hs-TNT) of patients with ST-Elevation Myocardial Infarction (STEMI), Takotsubo Syndrome (TTS) and the TTS subgroup with ST- elevation (TTS-TS) with significant lower means for TTS (p<0.001) and TTS-ST (p<0.001) compared to STEMI.
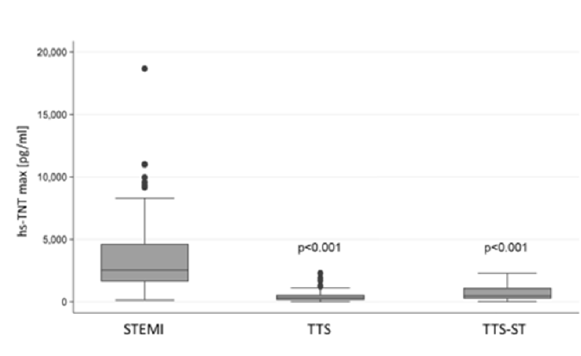
Figure 3: ROC curves of maximum High Sensitivity Troponin T (hs-TNT) and ratio of hs-TNT and CK-MB max for the diagnosis of STEMI, with area under the curves (AUC) and 95% confidence interval (95%-CI).
Left ventricular function
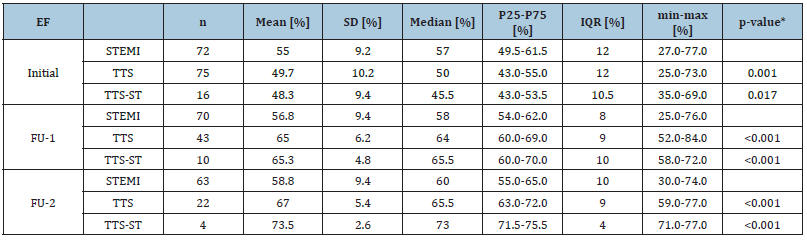
We examined left ventricular-EF for all 75 TTS patients and 72 of the STEMI patients by CMR (Figure 4). Initial EF was significantly lower in TTS patients with a median of 50% compared to 57% in STEMI patients. Lowest EF values were found in the subgroup of 18 TTS-ST patients, with a median of 45.5%, also statistically significant lower compared to STEMI patients. Median EF recovered to 64% in TTS and to 65.5 in TTS-ST patients in the First Follow Up (FU-1) after one month (Table 4), with only slight changes in STEMI patients to a median of 58% (Table 4). After three months (FU-2) we observed median values of 65.5% in TTS, 73% in TTS-ST and 60% in STEMI patients (Table 4).
Figure 4: Left ventricular Ejection Fraction (EF) for the patients with ST-Elevation Myocardial Infarction (STEMI) and patients with Takotsubo Syndrome (TTS). TTS and TTS-ST patients show a significant higher improvement compared to those with STEMI after one (FU-1) and three month (FU-2).
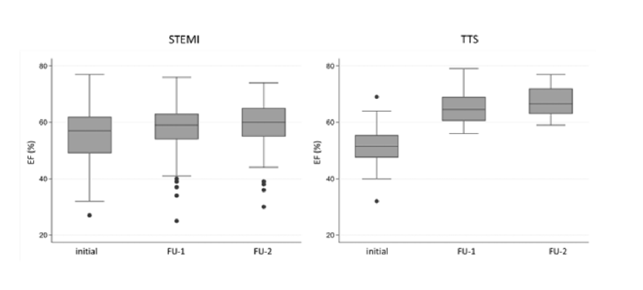
Table 4:Left-ventricular ejection fraction (EF) for the patients with ST-elevation myocardial infarction (STEMI), Takotsubo Syndrome (TTS) together with the TTS subgroup with ST- elevation (TTS-TS) at the initial examination and follow up assessment after one (FU-1) and three months (FU-2). Standard deviation (SD), lower and upper quartile (P25, P75), interquartile range (IQR).
Source: *t-test
Discussion
Diagnosis of TTS remains challenging, because of overlapping symptoms with acute coronary syndrome8. So far, the clinical diagnosis of TTS bases on the angiographic exclusion of coronary artery disease and typical cardiac imaging findings (e.g. apical ballooning). Clinical symptoms and ECG changes are insufficient for a reliable diagnosis [5] and specific biomarker are still lacking [1]. We conducted the present examination to define cut-off values for the cardiac biomarkers in the differentiation between TTS and STEMI patients and evaluate the follow-up of left-ventricular impairment.
Demographics and comorbidities
With a significant majority of middle-aged female patients, gender predominance and age of our findings are comparable to previous published examinations [4]. Data on pre-existing cardiovascular risk factors are inconsistent. Classically male sex, physical triggers and obesity are associated with poor prognosis in TTS patients, as well chronic kidney and pre-existing malignant diseases [9]. Dyslipidaemia, diabetes mellitus, and psychiatric disorders seem to have no obvious impact on TTS prognosis9. Madias revealed a lower prevalence of diabetes mellitus in TTS patients (16.8%) compared to 26.9% in the general population in the National Health and Nutrition Examination Survey [10]. Impaired autonomic innervation due to diabetic neuropathy may explain reduced TTS prevalence in diabetic patients. However, we observed overall lower diabetes prevalence in our cohort with 13.9% for TTS patients compared to the 16.5% in the STEMI group and no statistical significant difference.
Cardiac Biomarkers
Previous studies failed to identify specific biomarkers for TTS [1]. Classical cardiac biomarkers are usually moderately elevated in acute TTS [4]. Today, hs-TnT plays a crucial role in the early diagnosis of myocardial infarction [11]. Our study identified cut-off values for hs-TnT in the differentiation between TTS and STEMI.
In our cohort a maximal hs-TnT higher than 841pg/ml discriminates TTS from STEMI with a sensitivity of 90.6% and a specificity of 86.1%. In the exclusive analyse of our female patients a cut-off value of 1650pg/ml achieved optimal sensitivity (100%) and high specificity (95.5%). Creatine-kinase plays only a supplemental role in the acute setting of TTS. Usually the values show a slight elevation of CK and CK-MB8. Our results confirm these observations with slightly increased values of CK and CK-MB in TTS patients and significantly higher values in STEMI patients.
Left ventricular function and follow-up
We observed a significant reduced mean left ventricular-EF in patients with TTS compared to STEMI in the initial assessment, which in line with previous observations of impaired LV-EF in TTS [12]. In the follow-up EF remarkably recovered in TTS and TTS-ST patients, confirming pervious observations8. TTS was considered as relative benign disease, since left ventricular-EF in TTS usually recovers within a few weeks [13]. This is in line with our findings of significant EF improvement in TTS compared the STEMI patients. However, a report from the SWEDEHEART registry found a comparable prognosis of TTS and NON-STEMI patients [14]. Another study revealed a poorer outcome in TTS compared to patients with myocarditis and myocardial infarction without culprit lesion [12]. In addition, Scally et al. observed impaired cardiac deformation indices and increased native T1 mapping values in 37 patients with prior TTS, despite normalized LV- EF and biomarkers [15]. The authors therefore suspect long-term structural myocardial chances in TTS patients following initial left ventricular EF recovery [15]. In addition, a recent meta-analysis identified clinical predictors for a poor outcome in TTS patients including male sex and advanced age [16]. Further research is necessary to reveal long-term mechanical changes and additional prognostic factors in TTS.
Conclusion
i. Takotsubo syndrome showed lower peak values for hs-
TnT and CK-MB compared to STEMI, even in TTS patients with
electrocardiographic ST-elevation.
ii. Cut-off values for maximum hs-TnT may be able to
discriminate between TTS and STEMI, especially in female
patients with optimal sensitivity.
iii. Our data conform previous findings of significant left
ventricular EF recovery in TTS compared to STEMI patients.
References
- Khan H, Gamble D, Mezincescu A, Abbas H, Rudd A, et al. (2021) A systematic review of biomarkers in Takotsubo syndrome: A focus on better understanding the pathophysiology. IJC Heart & Vasculature 34: 100795.
- Dote K, H Sato, H Tateishi, T Uchida, M Ishihara (1991) Myocardial stunning due to simultaneous multivessel coronary spasms: A review of 5 cases. J Cardiol 21(2): 203-214.
- Chao Jin, Cong Tian, Yan Wang, Carol CW, Huifang Zhao, et al. (2020) A pattern categorization of CT findings to predict outcome of COVID-19 pneumonia. Front Public Health 8: 567672.
- Ghadri JR, Wittstein IS, Prasad A (2018) International expert consensus document on takotsubo syndrome (Part I): Clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J 39(22): 2032-2046.
- Dias A, Núñez Gil IJ, Santoro F (2019) Takotsubo syndrome: State-of-the-art review by an expert panel-Part 2. Cardiovascular Revascularization Medicine 20(2): 153-166.
- Dias A, Núñez Gil IJ, Santoro F (2019) Takotsubo syndrome: State-of-the-art review by an expert panel-Part 1. Cardiovascular Revascularization Medicine 20(1): 70-79.
- Wereski R, Kimenai DM, Taggart C (2021) Cardiac troponin thresholds and kinetics to differentiate myocardial injury and myocardial infarction. Circulation 144(7): 528-538.
- Templin C, Ghadri JR, Diekmann J (2015) Clinical features and outcomes of takotsubo (Stress) cardiomyopathy. New England Journal of Medicine 373(10): 929-938.
- Lu X, Li P, Teng C (2021) Prognostic factors of takotsubo cardiomyopathy: A systematic review. ESC Heart Fail 8(5): 3663-3689.
- Madias JE (2016) Low prevalence of diabetes mellitus in patients with takotsubo syndrome: A plausible ‘protective’ effect with pathophysiologic connotations. Eur Heart J Acute Cardiovasc Care 5(2): 164-170.
- Lipinski MJ, Baker NC, Escárcega RO (2015) Comparison of conventional and high-sensitivity troponin in patients with chest pain: A collaborative meta-analysis. Am Heart J 169(1): 6-16.
- Abanador-Kamper N, Kamper L, Costello-Boerrigter L, Haage P, Seyfarth M (2019) MRI findings in patients with acute coronary syndrome and unobstructed coronary arteries. Diagnostic and Interventional Radiology 25(1): 28-34
- Durowoju R, Li S, Huang GS (2022) Outcomes in takotsubo syndrome following left ventricular ejection fraction improvement. Am J Cardiol 169: 136-142.
- Björn Redfors, Ramtin Vedad, Oskar Angerås, Truls Råmunddal, Petur Petursson, et al. (2015) Mortality in takotsubo syndrome is similar to mortality in myocardial infarction-A report from the SWEDEHEART registry. Int J Cardiol 185: 282-289.
- Caroline Scally, Amelia Rudd, Alice Mezincescu, Heather Wilson, Janaki Srivanasan, et al. (2018) Persistent long-term structural, functional, and metabolic changes after stress-induced (Takotsubo) cardiomyopathy. Circulation 137(10): 1039-1048.
- Pei-Lun H, Zhi-Gang Y, Kai-Yue D, Shan H, Meng-T, et al. (2020) Comparison of clinical profiles between takotsubo syndrome and acute coronary syndrome: A systematic review and meta-analysis. Heart Fail Rev 25(5): 847-860.
© 2023 Abanador-Kamper N. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






