- Submissions

Full Text
Novel Research in Sciences
Studying and Investigating the Capacity of Dental Prostheses to Increase the Bond Strength of Ceramic Restorations (Case Study)
Sogol Poursamad* and Alexey Feshchenko
1IM Sechenov First Moscow State Medical University (MSMU), Moscow, Russia
2Kemerovo State Medical University, Moscow, Russia
*Corresponding author:Sogol Poursamad, IM Sechenov First Moscow State Medical University (MSMU), Moscow, Russia
Submission: January 23, 2023;Published: February 07, 2023
.jpg)
Volume13 Issue4February , 2023
Abstract
While adhesive cements assure proper bonding, all-ceramic restorations can restore lost functionalities and combine material strength with superior esthetics and long-term stability. The mechanical qualities of dental ceramics used in prosthodontics have significantly improved over the past several years because of new processing methods and improved microstructures. The most prevalent glass ceramic material, lithium desilicated, is a biocompatible and aesthetically pleasing material with exceptional mechanical qualities and a broad range of applications. It is used to fabricate inlays, veneers, and crowns (both anterior and posterior). Additionally, because they can preserve and extend the integrity of the tooth, these materials only need minimally intrusive preparation. The final clinical stage of cementation in permanent prosthesis can be exceedingly difficult. The correctness of two key operations completed during the most recent clinic visit the disinfection of the prepared tooth and cementation determines the durability of restorations.
Keywords: Photodynamic Therapy; Ceramic Restorations; Case Study; Ceramic; Biocompatible
Introduction
A standard technique for treating caries involves removing the soft, damaged dentine before restoring any teeth [1]. However, visual characteristics like the color and hardness of the dentine tissue are typically used to assess the state of the residual dentinal tissue after cavity preparation [2,3]. According to earlier research, this method is extremely arbitrary and is thought to be insufficient to accurately describe the bacterial state. Defect dyes have been proposed as a possible method for removing contaminated tissues, but this would not completely eradicate the microorganisms inside the cavity, and microorganisms would still be present in 20% to 45% of the teeth [4,5].
Dental technology has advanced significantly in recent years, and patient needs are now in line with available restorative options [6]. All-ceramic restorations can restore lost functionalities by fusing the durability of the materials with an aesthetically superior and longlasting finish, while adhesive cements guarantee strong bonding. Furthermore, because they may maintain and extend the integrity of teeth, these materials only need minimally intrusive preparations [7,8]. The final clinical phase in fixed prosthodontics is cementation, which can be quite difficult. The effectiveness of the two primary procedures-cementation and cleaning of the prepared tooth-performed during the most recent clinic appointment determines how long the restorations will survive [9].
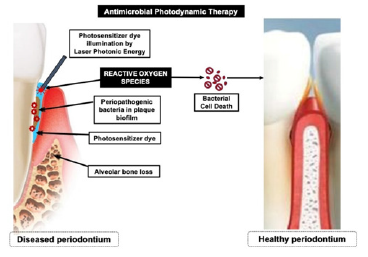
With the use of a photosensitizer, the right wavelength of visible light, and the formation of reactive oxygen species (mostly singlet oxygen), photodynamic treatment is a non-invasive method that causes substantial bacterial damage and death as well as phototoxicity right away. Its effectiveness against Streptococcus mutans, a Gram-positive bacteria that is the principal cause of dental caries, has been proven both in the free-living stage and when organized in biofilms. PDT has the ability to significantly reduce the amount of microorganisms on infected tooth surfaces [10]. When utilized as a cleaning treatment before cementation, photodynamic therapy can also improve adhesion [11]. However, in endodontics and orthodontics, PDT had a negative effect or had no effect on the bond strength and mechanical characteristics of the dentin from the intracanal prosthetic space and the bond strength of orthodontic brackets. We were unable to find any studies that could demonstrate the effect of PDT on prosthodontic cementation [12].
Additionally, it has been reported that microorganisms may continue to live between 0.1 and 2.4 millimeters from the cavity’s base to the dental pulp long after the caries dentine has been removed. In order to reduce post-operative sensitivity, secondary caries, and pulpal inflammation brought on by microorganisms, it is advised to utilize antibacterial adhesive systems, restorative materials, acids, and cavity disinfectants. For either direct or indirect pulp-capping techniques, calcium hydroxide (Ca(OH)2) can be utilized. The high pH of calcium hydroxide-containing cements, which has a damaging effect on bacterial cell membranes and protein structure, has been proven to have antibacterial action [13]. Ozone has also been suggested as a treatment for caries in addition to biotechnological materials because of its antibacterial properties. Previous research has demonstrated that ozonized water and ozone gas drastically diminish the total cultivable bacteria in vitro. S. mutans and Streptococcus sobrinus were much lower on the ozone-treated side of the root caries lesions compared to the control side, according to Baysan and Lynch [14].
Materials and Methods
Experimental design
A power analysis (Power and Precision software, Biostat, Englewood, NJ, USA) was conducted in order to determine an appropriate sample size based on previous studies. It indicated that detection of differences could be obtained with at least 11 teeth at a power of 0.8 (α=0.05). Thus, this study was conducted using 15 teeth per group (90 teeth in total). The study protocol was carried out according to the principles of the Helsinki Declaration, including all amendments and revisions. Collected data were only accessible to the researchers. Patients or their legal representatives gave their informed consent prior to any treatment of the teeth and the study was reviewed and approved by the institutional ethics board of the faculty (no: 118/2) [15,16].
Prosthodontic preparation
45 extracted human teeth (incisors, premolars, and molars) were used as the samples, and they were split into three groups as follows: 15 teeth were prepared for crowns, 15 teeth for class I inlays, and 15 teeth for veneers, with an extension of the preparation on the oral surface (noted from 1F to 15F) (noted from 1C to 15C) [17].
Bacterial contamination
Streptococcus mutans ATCC 25,175 from the Laboratory of Microbiology, Faculty of Biology, and Russia, Moscow, was the strain that was utilized [18]. The research bacteria was injected into the toothed tubes, which were then incubated in BHI-T culture media for 10 days at 36 °C. Teeth were taken out of the immersion environments after the incubation period and set on aluminum stubs with the prepared surface facing up. The samples were next inspected with a Scanning Electron Microscope (SEM) at a low vacuum, 90 Pa of pressure, and 30kV of acceleration. The presence of bacterial biofilm on prepared tooth surfaces was determined by Scanning Electron Microscopy (SEM-Inspect S, FEI) examination at a magnification of 5000 [19].
Prosthodontic restoration fabrication and cementation (Veneers, Inlays, and Crowns)
With Variotime polyvinyl siloxane from Heraeus in Hanau, Germany, impressions of each tooth were made using the sandwich impression method. Wax models were then created using the poured gypsum castings. Following the completion of the PDT previously discussed, each tooth was cemented in accordance with the manufacturer’s recommendations for the Dual-Cure (DC) luting composite Variolink Esthetic. Variolink Esthetic try-in paste was used to apply restorations to teeth, and the adaption was evaluated [20].
Statistical Analysis
The results were analysed using the Statistical Package for Social Sciences (SPSS 17.0 for Windows, SPSS Inc., Chicago, IL, USA). Analysis Of Variance (ANOVA) and Kruskal-Wallis test were used for statistical analysis. P-values of less than 0.05 were considered statistically significant in all tests [16].
Results and Discussion
The best strategy for assessing and developing antibacterial systems is thought to be clinical research. However, in vivo research is expensive, laborious, and time-consuming. The efficacy of the therapy has been linked to manipulation, ambient humidity, and sample choice. In vitro tests, however, are quick, simple, and less expensive. However, in vitro research might not accurately represent the oral environment. When the two procedures are used in tandem and reviewed, the most reliable result will be attained.
This study evaluated the efficacy of PDT as a technique for cleaning extracted teeth’s prepared coronary surfaces. An aggregation of streptococci covering the tooth structures was evident after SEM analysis of dental surfaces that had been prepared but were contaminated. Cells having a characteristic layout, such as solitary cells placed next to one another that had lost their unique chain conformation, were visible in the 8-day-old biofilm [21]. (Figure 1). Post-irradiation images that demonstrated the disappearance of the bacterial biofilm and the presence of only a few solitary remaining bacteria highlighted the antibacterial effect of photodynamic therapy. PDT was able to lower the number of colonizing streptococci on the surface of dental preparations [22]. In this study, we used ceramic prosthesis realized together with an occlusal or incisal bar parallel with their path of insertion, which served for assembling the universal testing machine and performing a mechanical pullout test.
Figure 1:Antimicrobial photodynamic therapy. www. crd.york.ac.uk/PROSPERO/; ref CRD 42019143316).
Conclusions
The growth of the bacterial biofilm and S. mutans adherence to prepared teeth were brought to light by pre-irradiation microscopic investigations. Lithium disilicate ceramic veneers, crowns, and inlays evaluated in terms of adhesive cementation shown good marginal adaptability. When PDT was used prior to cementation, a mechanical pullout test showed enhanced adhesion for all investigated groups. Comparatively to the veneer and crown groups, the inlay group exhibited a stronger connection. To increase the use of lasers in dental prosthesis, further research is required to assess the efficacy of various photosensitizers and lasers on adhesion and disinfection.g system is the main variable that determines the taste of the cheese.
References
- Alharbi N, Wismeijer D, Osman RB (2017) Additive manufacturing techniques in prosthodontics: Where do we currently stand? a critical review. Int J Prosthodont 30(5): 474-484.
- Tisler CE, Chifor R, Badea ME, Moldovan M, Prodan D, et al. (2022) Photodynamic Therapy (PDT) in prosthodontics: Disinfection of human teeth exposed to Streptococcus mutans and the effect on the adhesion of full ceramic veneers, crowns, and inlays: An in vitro Biomedicines 10(1):144.
- Bremer F, Grade S, Kohorst P, Stiesch M (2011) In vivo biofilm formation on different dental ceramics. Quintessence Int 42(7): 565-574.
- Wang Z, Shen Y, Haapasalo M (2014) Dental materials with antibiofilm properties. Dent Mater 30(2): e1-e16.
- Ahmed S, Shahnawaz K, Mandal TK, Ghafir M, Gummaluri SS, et al. (2022) Comparative evaluation of antimicrobial efficacy of herbal formulations of septilin and triphala with conventional 2% chlorhexidine on root canal and oral commensal bacteria using kirby bauer method: An in-vitro Contemp Clin Dent 13(4): 383-388.
- Moon W, Park JH, Lee HA, Lim BS, Chung SH (2021) Influence of additive firing on the surface characteristics, streptococcus mutans viability and optical properties of zirconia. Materials 14(5): 1286.
- Martina SS, Graf A, Preinerstorfer A, Watts DC, Piehslinger E, et al. (2011) Microleakage after thermocycling of cemented crowns-a meta-analysis. Dent mater 27(9): 855-869.
- Magalhaes APR, Santos LB, Lopes LG, Estrela CRdA, Estrela C, et al. (2012) Nanosilver application in dental cements. International Scholarly Research Notices 2012: 1-6.
- Gresnigt M, Cune M, Jansen K, Van der Made S, Özcan M (2019) Randomized clinical trial on indirect resin composite and ceramic laminate veneers: Up to 10-year findings. J Dent 86: 102-109.
- Naji GA-H, Omar RA, Yahya R (2017) Influence of sodalite zeolite infiltration on the coefficient of thermal expansion and bond strength of all-ceramic dental prostheses. J Mech Biomed Mater 67: 135-143.
- Quigley NP, Loo DS, Choy C, Ha WN (2021) Clinical efficacy of methods for bonding to zirconia: A systematic review. J Prosthet Dent 125(2): 231-240.
- Shimada Y, Yamaguchi S, Tagami J (2002) Micro-shear bond strength of dual-cured resin cement to glass ceramics. Dent Mater 18(5): 380-388.
- Ferrari M, Vichi A, Zarone F (2015) Zirconia abutments and restorations: From laboratory to clinical investigations. Dent Mater 31(3): e63-e76.
- Güngör MB, Nemli SK, Bal BT, Ünver S, Doğan A (2016) Effect of surface treatments on shear bond strength of resin composite bonded to CAD/CAM resin-ceramic hybrid materials. J Adv Prosthodont 8(4): 259-266.
- Blatz MB, Sadan A, Kern M (2003) Resin-ceramic bonding: A review of the literature. J Prosthet Dent 89(3): 268-274.
- Gadekar SV, Panse AM, Jathar P, Khairnar PS, Gadekar AV, et al. (2022) A comparative evaluation of shear bond strength of type IX GIC to demineralized dentin in primary teeth with and without application of SDF: An in vitro Journal of South Asian Association of Pediatric Dentistry 5(3): 157-163.
- Zarone F, Russo S, Sorrentino R (2011) From porcelain-fused-to-metal to zirconia: Clinical and experimental considerations. Dent Mater 27(1): 83-96.
- Roshdy NN, Kataia EM, Helmy NA (2019) Assessment of antibacterial activity of 2.5% NaOCl, chitosan nano-particles against Enterococcus faecalis contaminating root canals with and without diode laser irradiation: An in vitro Acta Odontol Scand 77(1): 39-43.
- Gökçen EY, Aksoy MK, Orhan Aİ, Özçelik B, ÖZ FT (2019) Assessment of the effectiveness of ozone theraphy and an antibacterial bonding agent on the cavity disinfection of deciduous teeth: An in vivo Cumhuriyet Dental Journal 22(4): 442-450.
- Bhat SA, Bhagat RK (2019) Evaluation of antibacterial efficiency of different pulp capping materials method against faecalis and S. mutans: An in vitro study. International Journal of Applied Dental Science 5(3): 13-15.
- Arora S, Saquib SA, Algarni YA, Kader MA, Ahmad I, et al. (2021) Synergistic effect of plant extracts on endodontic pathogens isolated from teeth with root canal treatment failure: An in vitro Antibiotics 10(5): 552.
- Khosla A, Gupta SJ, Jain A, Shetty DC, Sharma N (2020) Evaluation and comparison of the antimicrobial activity of royal jelly-a holistic healer against periodontopathic bacteria: An in vitro J Indian Soc Periodontol 24(3): 221-226.
© 2023 Sogol Poursamad. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






