- Submissions

Full Text
Novel Research in Sciences
Intrapartum Spontaneous Vulvar Hematoma Expectantly Handled
Georges Yared1,2,3, Aya Hussein1,4, Aya Ramadan5, Walid Saheb4,6, Charlotte El Hajjar and Kariman Ghazal1,4,6,7*
1Department of Obstetrics and Gynecology, Lebanese University, Lebanon
2Department of Obstetrics and Gynecology, Rafik Hariri Hospital University, Lebanon
3Department of Obstetrics and Gynecology, Lebanese American University, Lebanon
4Department of Obstetrics and Gynecology, Rafik Hariri Hospital University, Lebanon
5Department of Obstetrics and Gynecology, Lebanese American University, Lebanon
6Department of Obstetrics and Gynecology, Makassed General Hospital, Lebanon
7Department of Obstetrics and Gynecology, Lebanese University, Lebanon
*Corresponding author:Kariman Ghazal, Department of Obstetrics and Gynecology, Lebanese University, Lebanon
Submission: December 01, 2022;Published: December 09, 2022
.jpg)
Volume12 Issue5December , 2022
Abstract
Trauma during pregnancy affects around 5% to 7% of all pregnancies. Among the various injuries seen, vulva trauma has not been reported. Even outside of obstetrics, traumatic vulvar hematomas are infrequent. The incidence is unknown, and the literature is limited to previously documented instances. In this case Concerns about managing a non-obstetric traumatic vulvar hematoma in an obstetric patient at term gestation are highlighted in this instance
Keywords: Hematoma; Pregnancy; Term; Trauma; Vulvar; Delivery
Introduction
Vulvar Hematoma refers to a “collection of blood inside the vulva” [1]. A common obstetrical complication highly related to injury of the labial branches of the internal pudendal arteries [2]. Mostly, it is observed amongst the obstetric community following birth traumas involving repaired episiotomies and lacerations. Vulvar hematomas are uncommon amongst the non-obstetric population and typically occur after physical trauma. Saddle injuries have been linked to a variety of things, including bicycle crossbars, children’s toys, and snowboard boot bindings [3-5]. vulvar hematomas may suddenly occur without warning and cases have been documented in both pregnant and non-pregnant women [6-8]. It may be fatal when left undiagnosed and untreated [1]. Furthermore, there is very little research on the preferred management after a spontaneous hematoma appearance in terms of delivery route. The current case discusses the difficulties in managing a spontaneous rapidly expanding vulvar hematoma in a pregnant woman who is at term gestation.
Case Report
A 26-year-old Filipino primigravida presented at 38 weeks of gestation to our delivery suite reporting labor discomfort. The patient had a smooth pregnancy course and was followed in our outpatient department, she denied any history of bleeding or any other complaints. All her Antenatal investigations were within normal range, an Ultrasound done on 36+3 weeks revealed a Single intrauterine pregnancy [9]. The patient was seen and examined upon arrival to the delivery ward, her vitals were within normal range with pulse 86bpm and blood pressure 110/70. On per Vaginal examination cervix was 6cm dilated, with 80% effacement. She was admitted, and epidural analgesia was given at the request of the patient. The patient had a normal labor progression and reached full cervical dilation around 10 hours after admission. When the patient was being prepped and draped for normal vaginal delivery, in-out catheterization of the urinary bladder was done, given the patient was on epidural analgesia. Moments later, we noted the development of a right-sided vulvar hematoma, expanding rapidly and causing the patient exquisite pain despite the epidural.
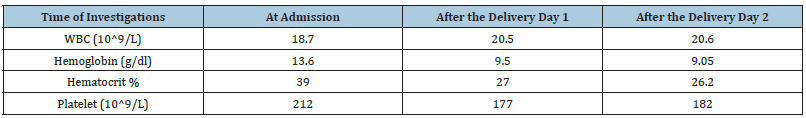
The hematoma reached a size of 10cm x 5cm (Figure 1) in less than 5 minutes and was still expanding while the patient is reporting a sudden excruciating back pain. The decision was taken to proceed with emergency cesarean delivery. On cesarean section, a liveborn baby girl weighing 3330 grams was delivered and transferred to the nursery. Intra-operatively, Uterus was normal, no intra-abdominal or pelvic hematomas were seen. After the cesarean section, we noted no further expansion of the hematoma. The decision was taken to apply ice packs and monitor the hematoma closely for any increase in size. IV antibiotics were given, and the urinary foley catheter was kept for 48 hours. Serial lab investigations revealed a drop in hemoglobin seen on day 1 post op (Table 1). Her vital signs were within normal range post-partum .The patient did not require any transfusion. The patient was discharged on day three post-delivery in stable condition, She was instructed to continue oral antibiotics for a total of 10 days. She presented for a wound check-up 10 days later, the hematoma had then decreased in size.
Figure 1:Follow up at 6 week post-partum revealed that the vulvar hematoma had resolved completely.

Table 1:
Discussion
Vulvar Hematomas are relatively common in the obstetrical community. They occur usually due to an injury involving a branch originating from the pudendal artery, this may occur after episiotomy or from perineal lacerations [4]. Many factors are involved in the development of a spontaneous vulvar hematoma including: first baby, macrosomia, rapid labor, extended second stage of labor, hypertension, varicosities or even clotting disorders [6,7]. The incidence of non-obstetric hematoma is not clear. The literature is limited to a few recorded cases. Due to its rarity, no general management guidelines exist. However, when the product of both hematoma diameters, longitudinal and transverse, is less than 15cm Benrubi G et al. [10] observed that conservatively handled patients had a longer hospital stay and required more procedures in the future [10]. Kanai et al. [5] reports managing large hematoma with surgery if the diameter reached more than 5cm. He reported complete recovery of all his patients without any complications [5] In our case the vulvar hematoma occurred spontaneously without instrumentation prior to delivery. Spontaneous vulvar hematomas are more common on the right side as in our case, because of the dextro-rotation of the uterus [5]. In our case the patient was primiparous however none of the other factors are applicable. Conservative therapy was typically beneficial in the absence of acute hematoma growth according to a retrospective analysis by Propst et al. [11] Selective arterial embolization was suggested to be useful in treating vulvar hematomas in both puerperal and nonpuerperal women [4,8]. Only a few case reports exist in the literature on the treatment of vulvar hematoma intra partum [6]. In another example, a spontaneous antepartum hematoma was successfully drained at 35 weeks gestation followed by an uncomplicated vaginal birth four weeks later [7]. Authors were doubtful about the mode of delivery in the instance of a second mother at 32 weeks. The woman arrived with a huge vulvar hematoma, despite that the hematoma was drained quickly the abdominal route was chosen for delivery at term due to the potential rebleeding of the arteries in the hematoma cavity during normal vaginal delivery [12]. The hematoma which was presented in a patient who was pregnant to term was steadily increasing in this case as well. Management of vulvar hematomas depends on: the hematoma size, degree of expansion, the hemodynamic state of the patient and the medical resources available. Small non-expanding hematomas will mostly resolve with expectant management [5,8].
This includes ice packs, sitz bath, antibiotics and even blood transfusion if needed in addition to administration of suitable analgesia or painkillers. Surgical management can involve surgical exploration or selective arterial embolization [5,9,10]. Large and expanding hematomas require surgical intervention in which ligation of the bleeding vessels is done to achieve hemostasis, followed by obliteration of the dead space then vaginal packing to compress the culprit site [10]. In case of failed surgical management arterial embolization is a therapeutic option [11]. In our case the hematoma reached a significant size of 10cm x 5cm in less than 5 minutes. However it stopped expanding on its own within a few moments after cesarean delivery. Thus we decided to go with conservative management. Vulvar injury trauma scoring systems should be updated to include clear guidelines on the management of hematomas. This will allow patients who report to the emergency room receive early care. Perplexities about the route of delivery for women in active labor after a rapidly expanding vulvar hematoma appearance must be addressed. More such instances must be reported in order to make evidence-based decisions about the route of delivery.
Conclusion
Vulvar hematoma is a serious complication, we need clear scoring systems in order to manage further emergency complications properly. Vulvar injury scoring systems should take pregnancy into consideration. This will allow patients who arrive to the emergency room to receive proper care in a timely manner to ensure a positive outcome on both the fetus and the mother. In cases where a woman in active labor may possibly require surgical therapy following hematoma repair. The question of whether a vaginal delivery is safe or whether a caesarean delivery is necessary in order to avoid further wound disturbance must be addressed. The more such occurrences are reported, the more evidence-based decisions concerning distribution routes may be made taking into consideration stable hematoma size in addition to the hemodynamic status of our patient. In certain cases, vulvar hematomas could be treated expectantly with complete resolution.
References
- Oong G, Eruo F (2022) Vulvar hematoma.
- Mangwi A, Ebasone P, Aroke D, Ngek L, Nji A (2019) Non-obstetric vulva haematomas in a low resource setting: Two case reports. Pan African Medical Journal 33: 314.
- Virgili A, Bianchi A, Mollica G, Corazza M (2000) Serious hematoma of the vulva from a bicycle accident: A case report. J Reprod Med 45(8): 662-664.
- Kunishima K, Takao H, Kato N, Inoh S, Ohtomo K (2008) Transarterial embolization of a nonpuerperal traumatic vulvar hematoma. Radiat Med 26(3):168-170.
- Kanai M, Osada R, Maruyama KI (2001) Warning from nagano: Increase of vulvar hematoma and/or lacerated injury caused by snowboarding. J Trauma 50(2): 328-331.
- Joy SD, Huddleston JF, McCarthy R (2001) Explosion of a vulvar hematoma during spontaneous vaginal delivery: A case report. J Reprod Med 46(9): 856-858.
- Nelson EL, Parker AN, Dudley EJ (2012) Spontaneous vulvar hematoma during pregnancy: A case report. J Reprod Med 57(1-2): 74.
- Egan E, Dundee P, Lawrentschuk N (2009) Vulvar hematoma secondary to spontaneous rupture of the internal iliac artery: Clinical review. Am J Obstet Gynecol 200(1): 17-18.
- Moore EE, Jurkovich GJ, Knudson MM, Cogbill TH, Malangoni MA, et al. (1995) Organ injury scaling. VI: Extrahepatic biliary, esophagus, stomach, vulva, vagina, uterus (nonpregnant), uterus (pregnant), fallopian tube, and ovary. J Trauma 39(6): 1069-1070.
- Benrubi G, Neuman C, Nuss RC, Thompson RJ (1987) Vulvar and vaginal hematomas: A retrospective study of conservative versus operative management. South Med J 80(8): 991-994.
- Propst AM, Thorp JM (1998) Traumatic vulvar hematomas: Conservative versus surgical management. South Med J 91(2): 144-146.
- Hacivelioglu S, Haydardedeoglu B, Simsek E, Cok T (2012) Giant vulvar hematoma during pregnancy after sexual intercourse: A case report. East J Med 17: 94-96.
© 2022 Kariman Ghazal. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






