- Submissions

Full Text
Novel Research in Sciences
Reevaluating the Pathogenesis and Classification of Thoracic Outlet Syndrome
Farid Gharagozloo*
Institute for Advanced Thoracic Surgery, Florida
*Corresponding author:Farid Gharagozloo, Institute for Advanced Thoracic Surgery, Florida
Submission: May 05, 2022;Published: May 19, 2022
.jpg)
Volume11 Issue1May, 2022
Abstract
Keywords: Keywords: Neurogenic; Venous; Surgical; Pathogenesis; Angiography; Subclavia; Cervical rib; Thoracic
outlet; Neurovascular; Tomograms; Venography; Hypothesized
Abbreviations:TOS: Thoracic Outlet Syndrome; PSS: Paget Schroetter Syndrome; SV: Subclavian Vein;
SC: Costo-Sternal; MRA: Magnetic Resonance Angiography
Introduction
Since 1956, with the publication of a paper by Peet, a diverse group of patients with symptoms in the shoulder and upper extremity who present with pain, numbness, tingling, and swelling, have been classified under the umbrella of “Thoracic Outlet Syndrome” (“TOS”) [1]. Conventionally, TOS has been thought to be characterized by compression of the neurovascular structures that traverse the thoracic outlet. Accordingly, TOS has been divided into 3 subtypes, Neurogenic (NTOS), Arterial (ATOS) and Venous (VTOS) which are thought to be the result of the compression of the brachial plexus, subclavian artery, or subclavian vein, respectively. However, in the six decades since Peet’s publication, TOS have been associated with the confusion among medical practitioners, difficulty in making the diagnosis, and poor results with surgical intervention. In the past decade, a number of observations, have resulted in reevaluation of the pathogenesis, diagnosis, and treatment of TOS. This communication outlines these observations which provide the evidence for the hypothesis that perhaps in the majority of patients, the complex upper extremity symptoms in TOS may be the result of the compression of the Subclavian Vein (SV) by a congenitally malformed medial aspect of the first rib and theresultantven congestion of the tissues that are fed by the subclavian vessels, as opposed to direct compression of structures in the thoracic outlet.
Venous TOS (Paget Schroetter Syndrome PSS)
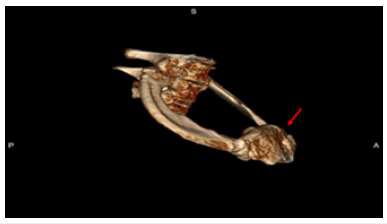
Examination of the medial aspect of the resected first ribs in patients with PSS has demonstrated the presence of a congenitally malformed bony tubercle which forms a tighter and wider joint at the junction of the first rib and the sternum [2]. It has been observed that the wider and less mobile cost-sternal joint “locks” the medial aspect of the first rib into place and results in extrinsic compression by the boney tubercle onto the Subclavian Vein (SV) at its junction with the innominate vein. This abnormal tubercle on the medial aspect of the first rib can be seen on Three-Dimensional (3D) reconstruction of computerized axial tomograms and can be demonstrated on dynamic Magnetic Resonance Angiography (MRA) with maneuvers as well as dynamic venography [3]; (Figure 1). Furthermore, these studies have demonstrated that the SV compression increases with elevation of the arm above the shoulder. In patients with PSS, it has been shown that disarticulation of the Costo-Sternal (SC) joint and resection of the “offending portion” of the first rib (portion of the rib medial to the SA) results in decompression of the SV and relief of Paget Schroetter Syndrome with return to full function of the affected upper extremity [4].
Figure 1: Three Dimensional reconstruction of the junction of the first rib and the sternum demonstrating the abnormal tubercle at the costo-sternal joint which results in extrinsic compression of the subclavian vein at the subclavian innominate junction.
Neurogenic TOS
Detailed assessment of symptoms in patients who present with
VTOS or Paget Schroetter Syndrome (PSS), has revealed a significant
history of unrecognized upper extremity neurologic symptoms
which predated the clotting of the subclavian vein and onset of
Paget Schroetter Syndrome (PSS). The neurologic symptoms were
relieved after undergoing resection of the abnormal portion of the
first rib for PSS. Therefore, it has been hypothesized that in a subset
of patients, NTOS may be the manifestation of compression of the
subclavian vein, and venous congestion resulting in venous ischemia
of the upper extremity nerves which lead to diffuse neurologic
symptoms unrelated to nerve compression.This hypothesis has
been supported by 4 observations:
i. The anatomic features of the first rib in normal individuals
was compared to the first ribs resected from patients with
NTOS who experienced complete postoperative symptom relief
following first rib resection. In patients with NTOS, the first
rib exhibited an abnormal bony tubercle immediately lateral
to the costo-sternal joint [5]. The tubercle was found in place
of the subclavian groove which is seen in normal first ribs. In
normal individuals, the rib thickness at the subclavian groove
was 0.2cm which represented an indentation of 0.8cm from the
rib surface. It was surmised that at the time of extension of the
upper extremity above the shoulder and elevation of the first
rib, the presence of this groove prevents compression of the
subclavian vein by the rib. On the other hand, in patients with
NTOS the thickness of the first rib at the abnormal tubercle was
1.4cm, which represents a differential elevation of 1.2cm above
the subclavian groove. Given the fact that the subclavian vein
has an average diameter of approximately 1cm in its position
over the first rib, it was concluded that the tubercle compressed
the subclavian vein at rest, and significantly occluded the vein
with extension of the arm above the shoulder [6].
ii. A study of patients with neurogenic TOS who
experienced persistent upper extremity pain following first
rib resection revealed persistent extrinsic compression of
the subclavian innominate junction on dynamic MRA. These
patients underwent video-assisted exploration of the chest
which showed a persistent SC joint despite evidence for prior
removal of the first rib. Disarticulation of the cost-sternal joint
and removal of the remaining portion of the first rib which
bore an abnormal tubercle alleviated the extrinsic compression
of the subclavian-innominate vein junction on postoperative
dynamic MRA and resulted in relief of Neurogenic symptoms in
all patients[7].
iii. In a proof-of-concept study, 97% of patients with NTOS
had complete relief of symptoms after robotic resection of the
medial aspect of the first rib and disarticulation of the SC joint
and relief of the extrinsic boney compression of the SV [8].
iv. Studies have demonstrated that the blood-nerve barrier
in the nerve root was more easily broken by venous congestion
than by arterial ischemia. Venous con- gestion may be an
essential factor precipitating circulatory disturbance in nerve
roots and inducing neurogenic intermittent claudication
[9]. Therefore, compression of the SV at its junction with the
innominate vein may result in elevation of venous pressure, a
decrease in arterial flow, and relative ischemia of the nerves of
the upper extremity. Venous ischemia of the upper extremity
nerves may manifest as pain, tingling, paresthesia and
numb- ness, and varying degrees of neurogenic intermittent
claudication depending on the degree and duration of venous
compression. Elevation of the extremity above the shoulder,
may result in greater compression of the SV, further venous
congestion, further decrease in arterial flow, greater degree
of ischemia of the upper extremity nerves, and exacerbation
of symptoms. This phenomenon is demonstrated on dynamic
Magnetic Resonance Imaging (MRI) and venography. The
pathophysiology of nerve pain in this setting has been likened
to symptoms that result from “crossing one leg over the knee”.
These observations have led to the hypothesis that NTOS
may be caused by “Venous ischemia” resulting in secondary neurologic symptoms as opposed to the direct “compressive” of
the nerves themselves.
Proposed Classification of Thoracic Outlet Syndrome
Peet’s classification of TOS was based on anatomic rather than symptomatic presentation of the disease. Based on recent studies, in order to decrease con- fusion and to improve therapeutic results with TOS, it is proposed that the disease should be classified based on the underlying pathologic entity. Acquired and traumatic abnormalities of the clavicle and first rib should be classified separately. Clearly after the more common and objectively supported diagnoses of conditions that result in neurovascular symptoms of the upper extremity such as cervical spine disease, carpal tunnel disease and nerve entrapment syndromes, have been ruled out, there remains a group of patients who are suspected of having TOS. In these patients rather than the historic classification such as arterial, venous, or neurogenic, the more accurate approach from a diagnostic and therapeutic approach may be to classify them as
Cervical Rib Disease (CRD)
In these patients an abnormal cervical rib or the associated bands that insert onto the first rib result in compression and displacement of the nerves or vessels in the neck. These patients can present with neurologic or vascular compromise. Patients with CRD can have complications relating to compression of the SA and the brachial plexus secondary to a well-formed cervical rib, or to an incompletely formed first rib, fibrous band associated with a rudimentary cervical rib, or a giant transverse process of C7. Although in the past, these patients have been classified as TOS, separation of these patients into CRD allows for a more precise diagnostic and therapeutic strategy and perhaps more importantly clears the way to a better understanding of diseases that result from anomalies of the first rib.
Thoracic Outlet Syndrome (TOS)
In these patients an abnormal first rib at the costo-sternal joint results in compression of the SV at the subclavian- innominate junction. Compression of the vein results in venous hypertension in the upper extremity and resultant neurologic symptoms. With prolonged compression of the subclavian-innominate junction, the vein clots giving rise to PSS. Therefore, patients who have been previously classified as neurogenic and venous TOS represent a variable symptomatic presentation of the same patho-logic entity which affects the SV. The term arterial TOS should be abandoned as these patients are better classified under cervical rib disease or under traumatic causes. On the other hand, neurogenic and venous TOS appear to be caused by the same pathophysiologic process which compresses the SV at its junction with the innominate vein. They represent different clinical manifestations of the same disease and represent the spectrum from pain to venous thrombosis. It is suggested that these conditions may best be classified “subclavian vein compression syndrome”.
References
- Peet RM, Henriksen JD, Anderson TP (1956) Thoracic outlet syndrome: Evaluation of a therapeutic exercise program. Proc Staff Meet Mayo Clin 31(9): 281-287.
- Gharagozloo F, Meyer M, Tempesta B (2012) Proposed pathogenesis of Paget-Shroetter disease: Impingement of the subclavian vein by a congeni- tally malformed boney tubercle on the first rib. J Clin Pathol 65(3): 262-266.
- Gharagozloo F, Tempesta B, Werden S, Meyer M (2020) Robotic first rib resection for thoracic outlet syndrome. Surg Tech Int 36: 239-244.
- Gharagozloo F, Meyer M, Tempesta B (2019) Robotic transthoracic first-rib resection for paget-schroetter syndrome. Eur J Cardiothorac Surg 55(3): 434-439.
- Gharagozloo F, Atiquzzaman N, Meyer M, Werden S (2021) Modern concepts in the diagnosis and management of thoracic outlet syndrome: A Review. American Journal of Surgical Research and Reviews 4: 27.
- Fortune JB, Feustel P (2003) Effect of patient position on size and location of the subclavian vein for percutaneous puncture. Arch Surg 138(9): 996-1000.
- Gharagozloo F, Atiquzzaman N, Meyer M, Tempesta B, Werden S (2020) Robotic first rib resection for thoracic outlet syndrome. J Thorac Dis 13: 10.
- Gharagozloo F, Meyer M (2022) Robotic transthoracic first rib resection for neurogenic thoracic outlet Syndrome. World J Cardiovasc Surg 12: 1.
- Kobayashi S, Takeno K, Miyazaki T (2008) Effects of arterial ischemia and venous congestion on the lumbar nerve root in dogs. J Orthop Res 26(11): 1533-1540.
© 2022 Farid Gharagozloo. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






