- Submissions

Full Text
Novel Research in Sciences
Comparison of Dexamethasone with Local Anaesthetic Versus Local Anaesthetic for Laparoscopic Port Infiltration to Assess Effectiveness as Post-operative Analgesia
Ariful Hoque1, Shamima Nasrin Shadia2 and Moazzem Hossain3*
1Junior consultant, Bangladesh
2Senior Lecturer, Bangladesh
3Chairman, Bangladesh
*Corresponding author: Moazzem Hossain, Chairman, Bangladesh
Submission: January 29, 2022;Published: February 28, 2022
.jpg)
Volume10 Issue3February, 2022
Abstract
Early postoperative pain remains the most prevalent complaint after any surgery. Beside conventional IV analgesic medications, subcutanious infiltration has been established as a reliable pain relief technique. Addition of dexamethasone to local anaesthetic (example: bupivacaine, lidocaine) can also be used as it has some beneficial effect than use of bupivacaine only. The objectives of this study to evaluate the duration of analgesic effects of dexamethasone with local anaesthetic as compared to local anaesthetic in post operative patient. This Randomized controlled trial study was conducted among 60 patients who underwent Laparoscopic cholecystectomy. This study was conducted from January,2019 to June,2019. All patients who underwent laparoscopic cholecystectomy surgery were selected by purposive sampling. Data were compiled, edited, analyzed. The SPSS version 23 was used for data analysis. In this study distributing the patient in demographic changes, age, sex, BMI do not show any significant change. Most Group 2 patients have long analgesia effect (NRS score more than 5), delay requirement of first rescue analgesia. NRS (Numerical Rating Scale) score in Group 2 were persistently lower than that of Group 1. This revealed that combination of Bupivacaine and Dexamethasone is quite effective in reducing postoperative port site pain in comparison to Bupivacaine (P=<0.001).
Introduction
Pain- it is not just a sensory modality but an experience. It recognizes the interplay among the objective, physiological sensory aspects of pain and its subjective, emotional & psychological components. The response of pain can be highly variable among different individuals as well as different time. Surgical better outcome prominently depends on control of pain. There are various ways of analgesic technique that ensure satisfaction to patient. With conventional IV, neuroaxial, enteral techniques local surgical site infiltration helps to minimize somatic pain which is a big concern for an anaesthesiologist. That’s why, it gains popularity in various aspect now a days. Many authors keep their focus into the different mechanisms of pain after laparoscopic cholecystectomy. With different intensity and time courses, visceral and parietal pain seems to be the most important during the first 24-48 hours after surgery. Local anaesthetic like bupivacaine has a half-life of 2.5 to 3.5 hours and has been reported to provide pain control for an average of 5 hours [1]. The margin of safety of the local anaesthetic need for anesthesia is wide [2]. The upper limit is 2mg of bupivacaine per kg body weight, 100mg of the drug can be used safely in a patient with a lean body mass of 50kgs [3]. The upper limit is 3mg of lidocaine per kg body weight, 150mg of the drug can be used safely in a patient with a lean body mass of 50kgs.Controversy exists on source of pain after laparoscopic procedures. Our study is designed to evaluate the effect of post operation analgesia after port site infiltration of local anaesthetic drug and dexamethasone for pain relief following laparoscopic cholecystectomy to provide effective control of pain.
Recently dexamethasone has been studied as an adjuvant to local infiltration for postoperative pain management [4,5]. Steroids have nerve block prolonging effects. They might bring about effect by altering the function of potassium channels in the excitable cells. Dexamethasone is effective in pain reduction after surgery. The mechanisms of the pain relief for the effects of dexamethasone through the decrease in cyclooxygenase and lipooxyginase products by suppressing phospholipase in the periphery plays a major role, also reduced bradykinin level and the concentration of nerve proteins secreted from the periphery nerve system are involved in the pain relief effect [6]. It has been reported about dexamethasone that it causes prolong duration of action of local anesthetics. Thus, dexamethasone has selected as an adjuvant with bupivacaine to compare with local anaesthetic only as postoperative pain management of laparoscopic cholecystectomy patients. The aim of our study to evaluate the duration of analgesic effects of dexamethasone with local anaesthetic as compared to local anaesthetic only in surgical incision port for postoperative pain management of laparoscopic cholecystectomy patients.
Material and Methods
This was a prospective comparative double-blind study which was conducted from January,2019 to June, 2019. Total sample was 60 patients were collected by purposive sampling from the study population of patients admitted into the department of Surgery, Bangladesh Medical College Hospital (BMCH) according to the eligibility criteria. Then, they were grouped in two- group 1 and group 2 and among these each group will belong to only 30 patients. They were Study Group 1 (Bupivacaine) = 30 and Study Group 2(Bupivacaine-Dexamethasone)= 30. Data were collected, completed, edited, managed and plotted into tabular and figure form. P value was found statistically significant at <0.05. All the qualitative variables was analyzed by chi square test whereas all the quantitative variables were analyzed by ‘t’ test. The SPSS version 23 was used for data analysis.
Study Procedure
A predesigned questionnaire and a consent form were prepared. The questionnaire consist of parts. The first part comprised demographic information of patients such as Age, sex, residence, Hight & weight for BMI calculation. The second part included questions about presence of diabetic mellitus, Per operative use of Opioid analgesia, NSAID & patient receiving medication for neuropathic pain (eg: gabapentin, pregabaline etc). The third part of questionnaire included first rescue analgesia in both group, postoperative pain score in 48 hours number and amount of rescue analgesia in 48 hours. All the patients were enrolled by purposive sampling. Thereafter, they were scrutinized according to eligibility criteria and 60 patients were finalized. All the patients were divided into two groups named Group-1 and Group-2 stand for Bupivacaine and Bupivacaine with Dexamethasone respectively. Here 12mL of 0.5% bupivacaine solution with 8ml normal saline, total 20mL was infiltrated into the point site (6mL was infiltrated around each midline port sites and 4mL administered in the similar fashion at the lateral port sites) in Group 1. On the contrary, Group 2 patients will have 20mL solution contains 12mL of 0.5%. Bupivacaine solution with 2mL of 10mg Dexamethasone and 6mL of normal saline.
The particular patients and volunteer who will observe as well as collect data in post-operative period were in the dark regarding which drug they are adopting as it is a double blind RCT. Only researcher will know about drugs composition. They were examined by Numerical Rating Scale (NRS) for pain and ask for the perfect expression in the respective score. The scale range from 0-10, with 0 being the mildest pain the patient ever had and 10 being the most severe pain. Respondents are most commonly asked to report pain intensity. In all cases, induction, maintenance and reversal of anesthesia was achieved by standard protocol. After approach through open technique intraperitonial gas was done by CO2 keeping the gas pressure between 12-14mm of Hg. Laparoscopic cholecystectomy was done by surgeon. After extraction of gall bladder, inj. Paracetamol 1gm/100ml IV was given to all patients of this study. Thereafter, when surgeon closed the laparoscopic port with suture, 12mL of 0.5% bupivacaine solution with 8ml normal saline, total 20mL was infiltrated into the point site (6mL was infiltrated around each midline port sites and 4mL administered in the similar fashion at the lateral port sites) in Group 1. On the contrary, Group 2 patients will have 20mL solution contains 12mL of 0.5%. Bupivacaine solution with 2mL of 10mg Dexamethasone and 6mL of normal saline. The time just after infiltration was defined as ‘0’ hour postoperatively. Patient’s pain complain was observed by Numerical Rating Scale (NRS) after 1 hour as because pain complain is least in the beginning first few hours 1 hour for per-operative analgesia as well as infiltration anaesthesia. Pain intensity was measured by continuous monitoring up to 48 hours. Our goal was to documentation the 1st use of rescue analgesia and total number of uses of rescue analgesia in 48 hours in both groups.
Result
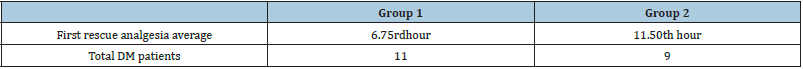
Distributing the patient in demographic changes, age, sex, BMI do not show any significant change. Most Group 2 patients have long analgesia effect (NRS score more than 5), delay requirement of first rescue analgesia. Even total doses of rescue analgesia within 48 hours in Group 2 is lower than group 1. NRS (Numerical Rating Scale) score in Group 2 were persistently lower than that of Group 1. This revealed that combination of Bupivacaine and Dexamethasone is quite effective in reducing port site pain in comparison to Bupivacaine (P=<0.001). In our study among the 60 patients, 34(56.67%) were female and 26 (43.33%) male. Table 1 shows the demography of study population. There are no statistical significance among age, sex and body weight of patients in both group. The Figure 1 shows that, hours of first demand of rescue analgesia is significantly higher in group 2 (Bupivacaine + Dexamethasone) than group 1. Average 10.75 hours in group 2 than 5.50 hours in group 1 (p=<0.05) which is significant. Rescue analgesia requirements & VAS score (N=60; 30 in each group) Table 2 shows that Group-2 patients required statistically significant lower number of rescue analgesia Inj. Pethidine (P=0.003). Total 4(13.3%) and 2 (6.67%) out of 30 patients in group 1 and group 2 in each group required rescue analgesia respectively. Table 3 shows that; in both groups, DM patients need less analgesia than non-DM patients. Moreover, first rescue analgesia in group 2 is longer than group 1.
Table 1: Distribution of patients according to demography (N=60; 30 in each group).
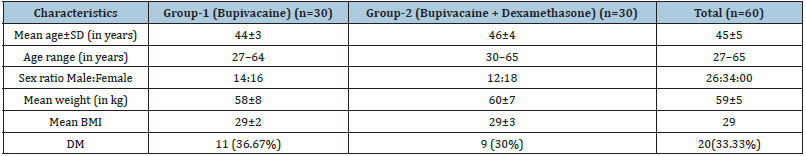
Figure 1: Distribution of patients according to first demand of analgesia.
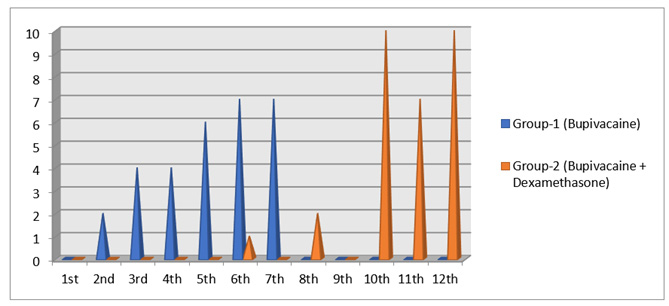
Table 2: Distribution of patients according to rescue analgesia Inj. Pethidine requirements within 48 hours (N=60; 30 in each group).
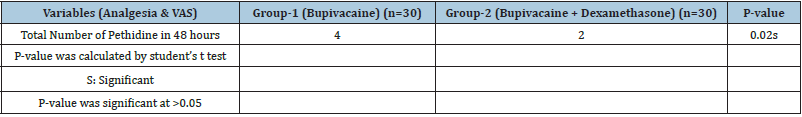
Table 3: Scenario in Diabetic Mellitus (Control) Patients.
Discussion
In the present study patients required statistically significant lower number of rescue analgesia Inj. Pethidine (P=0.003) among study Group-2(Bupivacaine-Dexamethasone). In spite of these studies, the exact mechanism of action of dexamethasone prolongation of the duration of local anesthetic blocks is not yet clearly understood and whether it is due its local or systemic effects. Adequate postoperative pain management is a crucial component in surgical patient care. Effective postoperative pain management not only improves the patient’s level of comfort and satisfaction but also is associated with earlier mobilization, fewer cardiopulmonary complications, reduced risk of thromboembolism, earlier return of bowel function, faster recovery, and reduced hospital costs [7]. Traditionally, opioid analgesics that act on mechanisms associated with pain perception have been used in managing postoperative pain. While opioid medications, including morphine, hydromorphone, fentanyl, and meperidine, are very effective analgesics, they are also associated with numerous adverse side effects that include somnolence, respiratory depression, cardiac instability including hypotension and bradycardia, and nausea, vomiting, pruritus, and constipation [8]. Multimodal pain management aims for additive or synergistic effects by utilizing analgesic medications of various classes that have differing pharmacologic mechanisms of actions in the nervous system [9]. By combining multiple drugs from different classes, multimodal pain management regimens aim to provide adequate pain management, while reducing the amount of required postoperative opioid use and its associated adverse effects. Dilek et al. [10] showed that Infiltration of the incision site with the longacting local bupivacaine after administering general anesthesia [10]. Timing of analgesia play a major role in reduction of postoperative pain score and preventing the development of chronic pain syndrome [11].Our study revealed that combined analgesia with dexamethasone-bupivacaine can reduce postoperative pain in comparison with only Bupivacaine. So, it can be claimed without hesitation that combined analgesia bupivacaine and dexamethasone can also decrease total consumed analgesic. Lim et al. found that intravenous injection of Dexamethasone before and after laparoscopic cholecystectomy has been effective in reducing postoperative pain. A study by Fukami et al. also showed that Dexamethasone in combination with Bupivacaine infiltration in port site has significantly reduced postoperative pain after laparoscopic cholecystectomy [12]. Studies found no increase in infection associated with steroid administration [13]. But in this study, no such event was observed as it was not implemented intravenously. We used injection pethidine as rescue analgesics in our study. Here the dramatic improvement was also noted in Group 2 where only 14(46.67%) patients required rescue analgesia. On the contrary, 27(90%) patients asked for rescue analgesia in Group 1.
If laparoscopic cholecystectomy is to be a routine ambulatory surgical procedure, the pain experienced by the patients during early postoperative period must be addressed. Our study showed that Infiltration of combination of bupivacaine and dexamethasone into the port site in comparison to bupivacaine reduce the peak of pain occurring during the first 9 hours after the surgical procedure and significantly reduces the need for narcotic analgesics. Any reduction in such pain is relevant, particularly if it is statistically significant, whether the lower pain score translated into increased patient’s comfort and compliance is questionable. However, at whatever level they functioned they did so more comfortably.
Conclusion
Combination of Dexamethasone with Bupivacaine infiltration in port site of laparoscopic cholecystectomy is much more significant in reducing post-operative pain, requirements of rescue analgesics and pain score in comparison to only Bupivacaine infiltration in same site. As it works with bupivacaine, it will work with other local analgesics too.
Ethical Clearance
The Ethics Committee of Bangladesh Medical College Hospital approved the study, and all patients gave their written informed consent to participate in the study.
Author Contribution
Md. Ariful Hoque contributions to conception and design,acquisition of data, analysis and interpretation of data, in drafting the manuscript. Shamima Nasrin Shadia contributions to analysis and interpretation of data, in drafting the manuscript . Moazzem Hossain has been involved in analysis and interpretation of data, in drafting the manuscript. All authors read and approved the final manuscript.
Acknowledgement
We thank the Principal, Director and Head of Department of Anaesthesia, Bangladesh Medical College Hospital, Dhaka. We also thank Associate Prof. Rafiqul Hasan Khan and Prof. Dr. Kamal Ibrahim, Department of Anaesthesiology, Bangladesh Medical College & Hospital. This study is not funded by any institutions.
References
- Rana RS, Darpan B, Manbachan S, Avreen SS (2016) Randomized controlled study of effectiveness and timings of bupivacaine at port site in managing pain after laparoscopic cholecystectomy. ISJ 3(4).
- Alexander DJ, Ngoi SS, Lee L, So J, Mak K, et al. (1996) Randomized trial of periportal peritoneal bupivacaine for pain relief after laparoscopic cholecystectomy. Br J Surg 83(9): 1223-1225.
- Cunniffe MG, McAnena OJ, Dar MA, Calleary J, Flynn N (1998) A prospective randomized trial of intraoperative bupivacaine irrigation for management of shoulder-tip pain following laparoscopy. Am J Surg 176(3): 258-261.
- Ikeuchi M, Kamimoto Y, Izumi M, Fukunaga K, Aso K, et al. ( 2014) Effects of dexamethasone on local infiltration analgesia in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 22(7): 1638-1643.
- Ahmed MM, Wesam SD, Sahar E, Ahmed RE, Ahmed AM, et al. ( 2018) Comparison of local and intra venous dexamethasone on post operative pain and recovery after caeseream section. A randomized controlled trial 57(3): 346-350.
- Callery MP (2003) Preoperative steroids for laparoscopic surgery. Ann Surg 238(5): 661-662.
- Joshi GP, Ogunnaike BO (2005) Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiol Clin North Am 23(1): 21-36.
- Oderda GM, Said Q, Evans RS, Gregory JS, Jim L, et al. (2007) Opioid-related adverse drug events in surgical hospitalizations: impact on costs and length of stay. Ann Pharmacother 41(3): 400-406.
- Elvir LOL, White PF (2010) The role of multimodal analgesia in pain management after ambulatory surgery. Curr Opin Anaesthesiol 23(6): 697-703.
- Dilek K, Sývacý RG, Akbulut G, Dilek ON (2006) Preemptive analgesia in laparoscopic cholecystectomy: A randomized controlled study. Pain Practice 6(4): 237-241.
- Pogatzki ZEM, Zahn PK (2006) From preemptive to preventive analgesia. Curr Opin Anaesthesiol 19(5): 551-555.
- Fukami Y, Terasaki M, Okamoto Y, Sakaguchi K, Murata T, et al. (2009) Efficacy of preoperative dexamethasone in patients with laparoscopic cholecystectomy: a prospective randomized double-blind study. J Hepatobiliary Pancreat Surg 16(3): 367-371.
- Waldron NH, Jones CA, Gan TJ, Allen TK, Habib AS (2013) Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth 110(2): 191-200.
© 2022 Moazzem Hossain. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






